Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Myocardial and pulmonary perfusion is regulated by a complex array of influences intrinsic and extrinsic to the vasculature. Surgical decisions are generally based on the anatomy of large arteries, where the presence of obstructive lesions and vasomotor state of these vessels can affect myocardial, pulmonary, or other organ perfusion. Under normal circumstances, the microcirculation actually plays a more significant role in the regulation of blood flow. A basic understanding of vascular tone and vasomotor regulation, and the influence of various disease states, is necessary to optimize patient care. Over the past four decades, a great deal has been learned, and this has promoted the understanding of blood vessel regulation and organ perfusion in healthy and in diseased states.
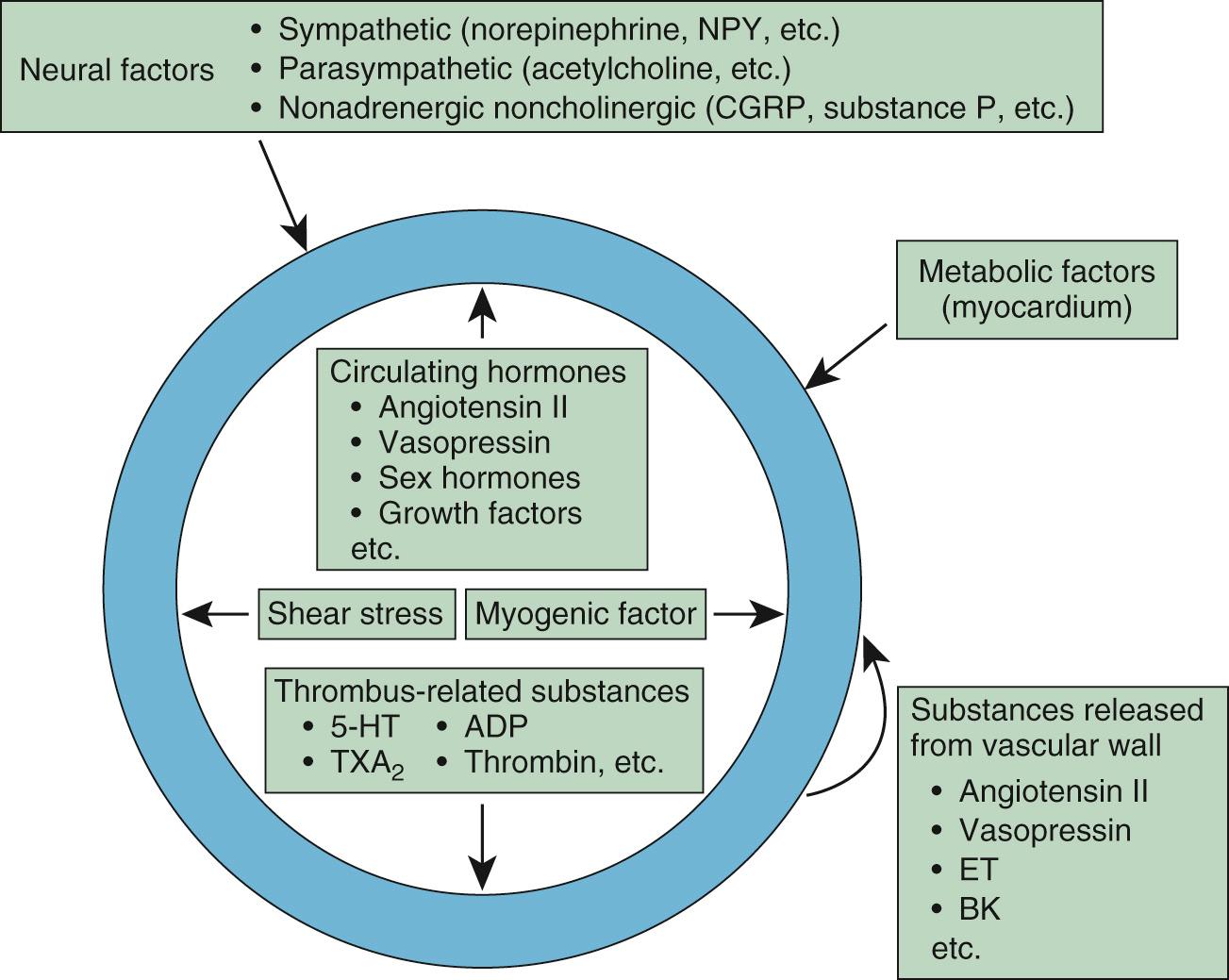
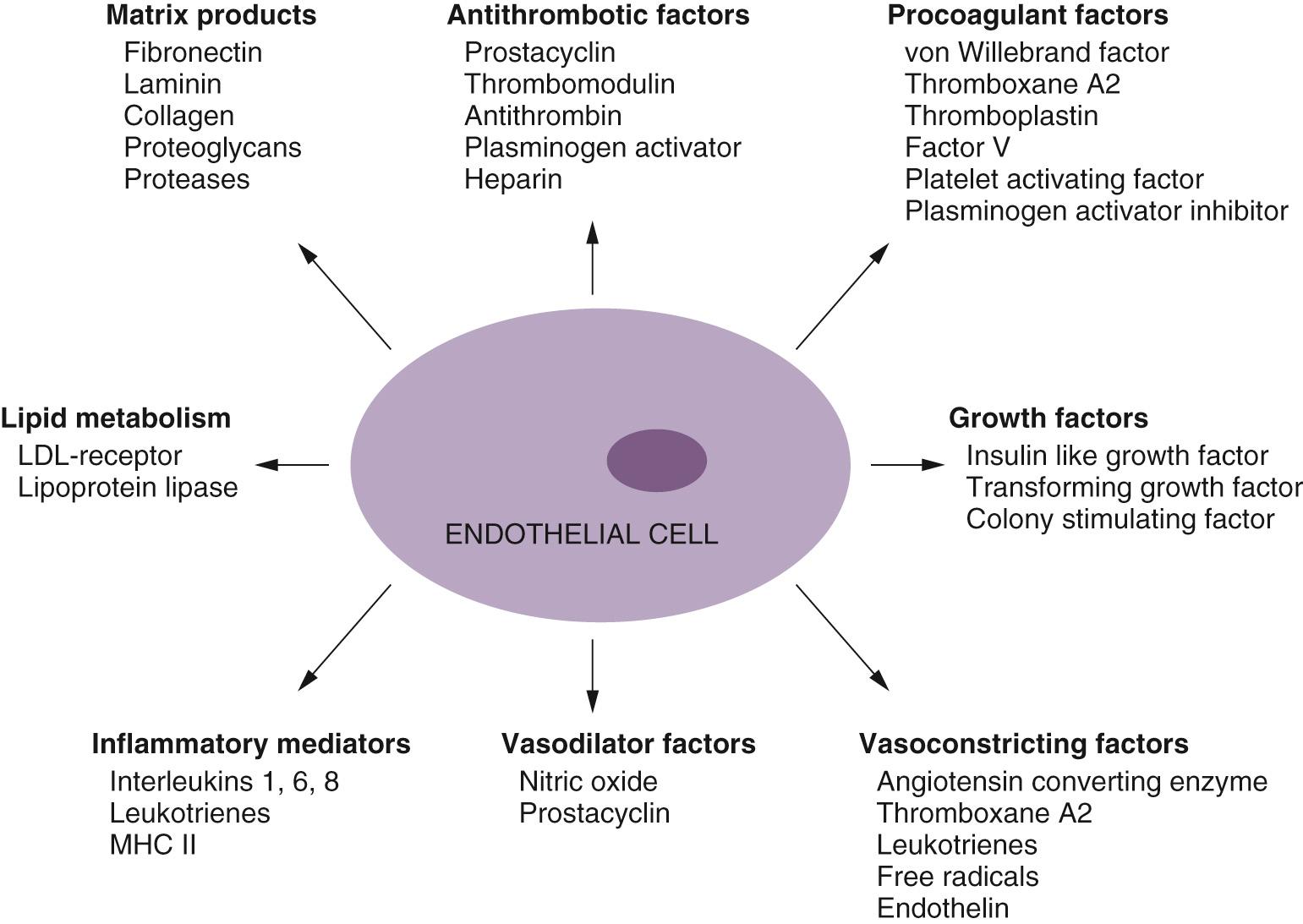
The blood vessel wall is organized in three layers: the intima, media, and adventitia. The innermost, or intimal, layer is made of endothelial cells. Initially, the endothelium was thought to serve mainly as a barrier to the diffusion of macromolecules, but it is now known that the endothelium plays a pivotal role in vascular function, regulation of vascular tone, and control of local blood flow. The medial layer surrounds this intimal endothelial layer, and it is composed of a variable number of smooth muscle cells. Smooth muscle cells also control vascular tone via humoral vasoactive factors, neural mediators, or local paracrine factors ( Fig. 48-1 ). The outermost, adventitial, layer surrounds these vascular smooth muscle cells and provides structural integrity to the blood vessel, particularly larger arteries.
The classification of microvessels based on structural characteristics is rather arbitrary, and there is a lack of uniformity in the definitions of microvascular segments such as small arteries, arterioles, and venules. Furthermore, the transition between these segments is gradual, and there is no clear demarcation between them. In general, microvessels are defined as vessels less than 300 µm in internal diameter. Capillaries are the smallest blood vessels, defined as vessels whose walls are composed of only endothelial tubes. The microvessels through which blood flows toward capillaries are arterial microvessels, and those that drain from capillaries are venous microvessels. Arterial microvessels usually have three coats: (1) a thin tunica intima; (2) a relatively thick tunica media, composed of one to several layers of smooth muscle cells disposed circumferentially; and (3) tunica adventitia, composed of fibrous elements and fibroblasts. Venous microvessels collect the blood from capillaries and have thinner vascular walls than arterial microvessels do. Venules (50 µm in diameter) do not possess smooth muscle cell layers. Smaller venules are composed of only endothelial cells and pericytes. Venules are highly permeable and have an important role in nutrient exchange.
The regulation of myocardial perfusion depends on many intrinsic and extrinsic factors that might be affected by atherosclerotic lesions. In the coronary circulation, it has been shown that vasomotor regulation of vessels, in addition to the actual anatomy, plays an important role in coronary perfusion and operative decision making. Blood flow is also largely dependent on the resistance generated by the microcirculation. Although early studies on vasomotor regulation consisted of indirect assessments using measurements of flow and calculations of resistance, recent investigations into the properties of the intact coronary circulation have yielded much information, as have modern methods of analysis for interpretation of physiologic data.
The microcirculation possesses unique features that allow it to respond to the dynamic changes in nutrient requirements and to interact with surrounding tissue. It is important to note that although the various vascular beds in the body possess many similarities, there are also subtle differences. This chapter will discuss regulation of vascular tone, with an emphasis on coronary and pulmonary circulation, and will review the physiologic and molecular basis of recent advances in ischemic cardiac disease.
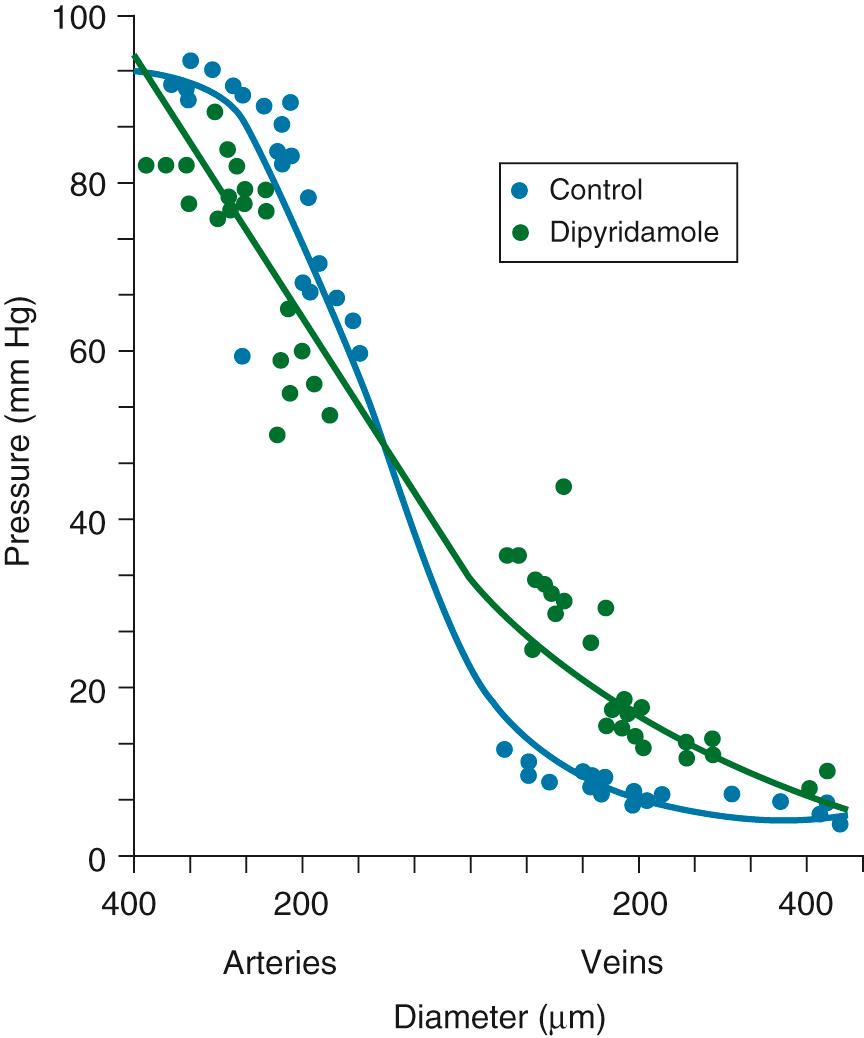
An understanding of vascular resistance is important, because these resistance vessels cause pressure losses and are responsible for regulation of perfusion. Initially, it was thought that the precapillary arterioles were responsible for vascular resistance, with little resistance involvement by the vessels larger than 25 to 50 µm in diameter. However, subsequent work revealed that over half of total vascular resistance is caused by vessels with diameters larger than 100 µm, even including vessels up to 300 µm. Contrary to previous belief, the venous circulation, under conditions of vasodilation, may account for up to 30% of vascular resistance. Figure 48-2 shows that after vasodilation with dipyridamole, larger arteries and veins assume a greater role in resistance. Similarly, ischemia results in a significant redistribution of vascular resistance ; this reveals that the distribution of vascular resistance is dynamic and is also largely dependent on vascular tone.
The redistribution of microvascular resistance can change the myogenic tone in each microvascular segment because the luminal pressure in a certain vascular segment is determined by the systemic pressure and the upstream distribution of vascular resistance. For example, when resistance is shifted upstream by the dilation of small arterioles, the luminal pressure in the upstream microvessels decreases, resulting in myogenic dilation. Changes in the venular pressure caused by the resistance redistribution can also affect the capacity for substance exchange and lead to edema formation.
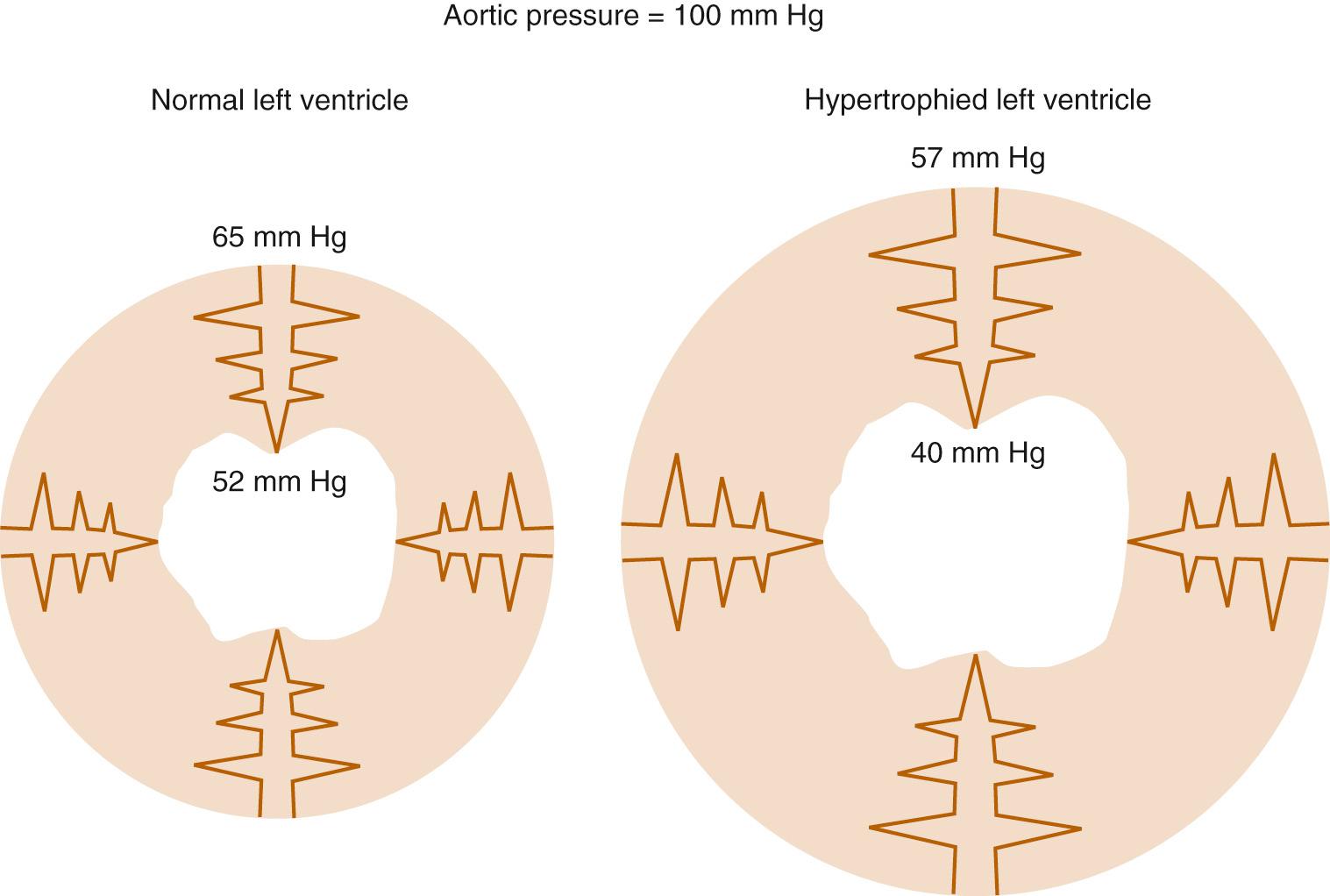
In the coronary circulation, pressure losses also occur as vessels course from the epicardium through the myocardium ; this is accentuated further in the setting of cardiac hypertrophy. Such a phenomenon is particularly relevant clinically, as it in part explains the propensity of the subendocardium to develop ischemia in hypertrophied hearts ( Fig. 48-3 ). The hypertrophied pathologic state causes a decrease in the perfusion pressure of the subendocardium, predisposing it to ischemia and infarction.
Vasomotor tone is influenced by the intrinsic properties of the vessel wall, by local innervation, and by substances from surrounding parenchymal tissue. This regulation of vasomotor tone is critically involved in organ perfusion. Vascular responses to endogenous substances are summarized in Figure 48-4 . All these factors have an especially significant role in the setting of microvascular tone.
Based on in vitro observations, Jones and colleagues found that larger arterioles are more sensitive to shear stress than myogenic factors, whereas small microvessels are more sensitive to metabolic factors. They organized arterial microvessels into three microdomains as governed by distinct forms of regulation based on vessel size: (1) small arterioles (<50 µm), most sensitive to metabolic mediators; (2) intermediate arterioles (50 to 80 µm), most sensitive to myogenic mechanisms; and (3) large arterioles (80 to 150 µm), most sensitive to flow-induced dilation. Undoubtedly, there is overlap among these three components; however, this model provides a framework for understanding the regulation of microvessels.
Jones and colleagues hypothesized that the longitudinal disposition of these three microdomains enables integrated adjustment of flow conductance in the face of various influences, such as increased metabolism or a reduction in perfusion pressure. For example, dilation of small arterioles by augmented metabolism produces a decrease in luminal pressure in upstream microvessels, leading to the dilation of intermediate arterioles by decreasing the myogenic tone. These microvascular dilations could also produce an increase in shear stress and result in enhanced flow-induced dilation in large arterioles. As a result, all sizes, or domains, of arterial microvessels dilate in response to the metabolic stimulation. The marked longitudinal heterogeneity of microvascular responses may be at least partly explained by this microdomain hypothesis.
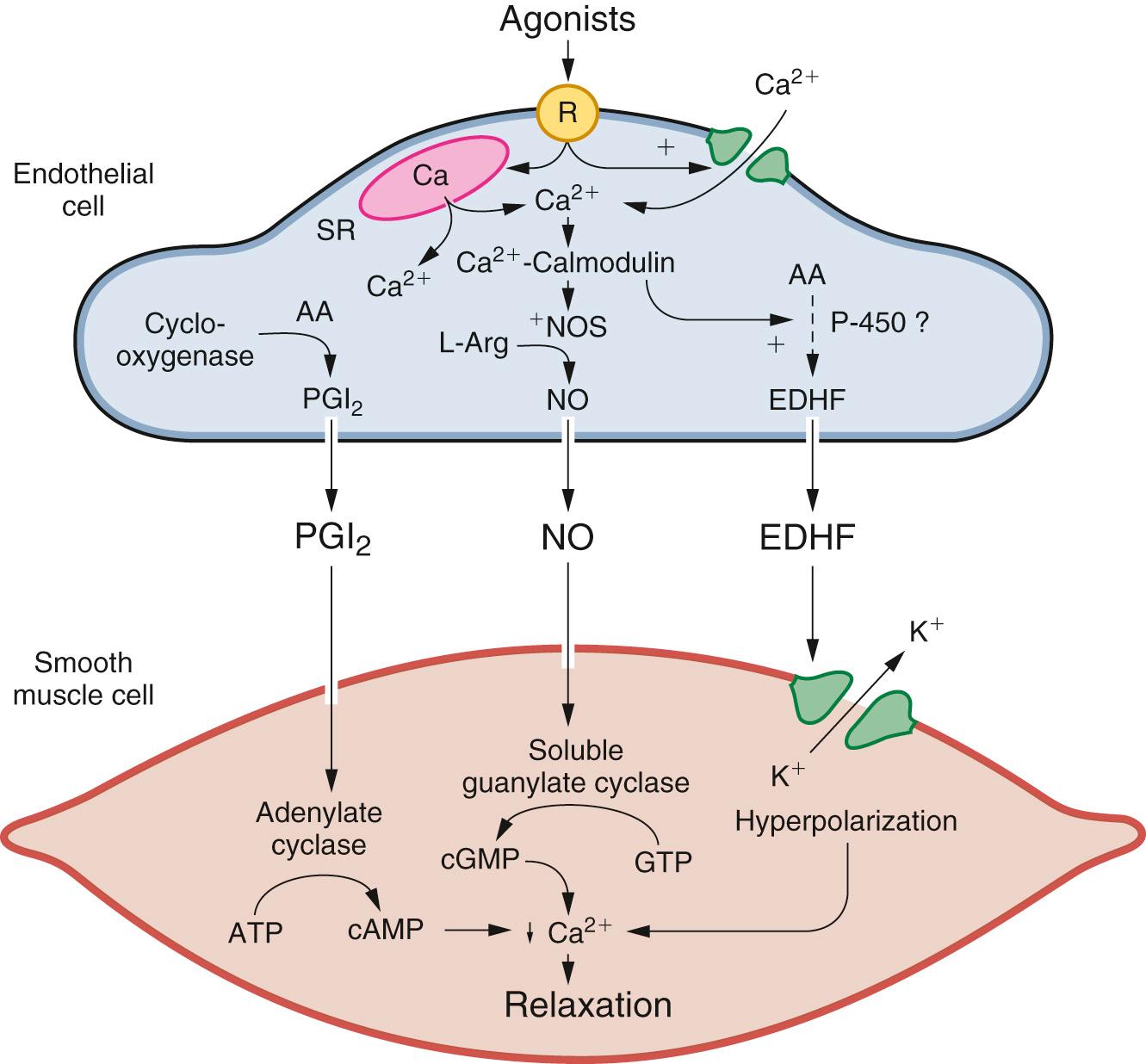
The endothelium plays a pivotal role in vasomotor tone regulation. Many substances affect tone via endothelium-mediated mechanisms. Endothelial cells also release several substances that affect coronary resistance, including vasodilators such as nitric oxide (NO•), prostaglandins, and vasoconstrictors including angiotensin converting enzyme endothelin, and reactive oxygen species (summarized in Fig. 48-5 ). As the major regulatory molecule, NO• is produced by a constitutively expressed enzyme known as endothelial nitric oxide synthase (eNOS or NOS-3). NO• is formed as a result of a series of electron transfers from reduced nicotinamide adenine dinucleotide phosphate (i.e., NADPH) to flavin adenine dinucleotide (FAD) and flavin mononucleotide (FMN) on the reductase domain, and electron transfer to a prosthetic heme group in the oxygenase domain. When heme reduction occurs, arginine is catalyzed to citrulline and NO•. The NO• formed diffuses to underlying vascular smooth muscle, where its actions include stimulation of soluble guanylate cyclase, increasing the level of cyclic guanosine monophosphate (cGMP) and prompting vasodilation via activation of cGMP-dependent protein kinase. Although binding of calcium and calmodulin is a prerequisite for activity of eNOS, other events, such as phosphorylation, membrane binding, binding of eNOS with heat-shock protein 90, and association with the integral membrane protein caveolin can also modulate NOS activity. In addition, NO• can undergo reactions with thiol-containing compounds to form biologically active nitroso molecules.
Although eNOS is expressed constitutively, it undergoes important gene expression regulation by factors such as shear stress, endothelial cell growth, hypoxia, exposure to oxidized low-density lipoprotein, and exposure to cytokines. In the coronary circulation, the release of NO• confers a state of basal vasodilation; therefore, administration of NO• synthase antagonists increases resting coronary resistance. However, when substances such as acetylcholine and bradykinin are administered, coronary microvessels of all sizes dilate, resulting in decreased coronary resistance. Endothelial NO• production is affected by a variety of mechanisms in many disease states. The signal transduction pathways through which NO• acts are summarized in Figure 48-6 . It is likely that the most important pathway involves activation of soluble guanylate cyclase, which catalyzes the formation of cGMP from guanidine triphosphate. The cGMP serves as an allosteric regulator of the enzyme cGMP-dependent protein kinase, which phosphorylates contractile proteins and ion channels, decreasing intracellular calcium and the sensitivity of contractile proteins to intracellular calcium. The binding of NO• to cytochrome oxidase in the mitochondria alters oxygen consumption and in turn can affect oxygen demand. Similarly, receptors for atrial natriuretic peptide and brain natriuretic peptide are also the particulate forms of guanylate cyclases, and these signal vasodilation via similar pathways. NO• is also released in response to sodium nitroprusside and organic nitrates.
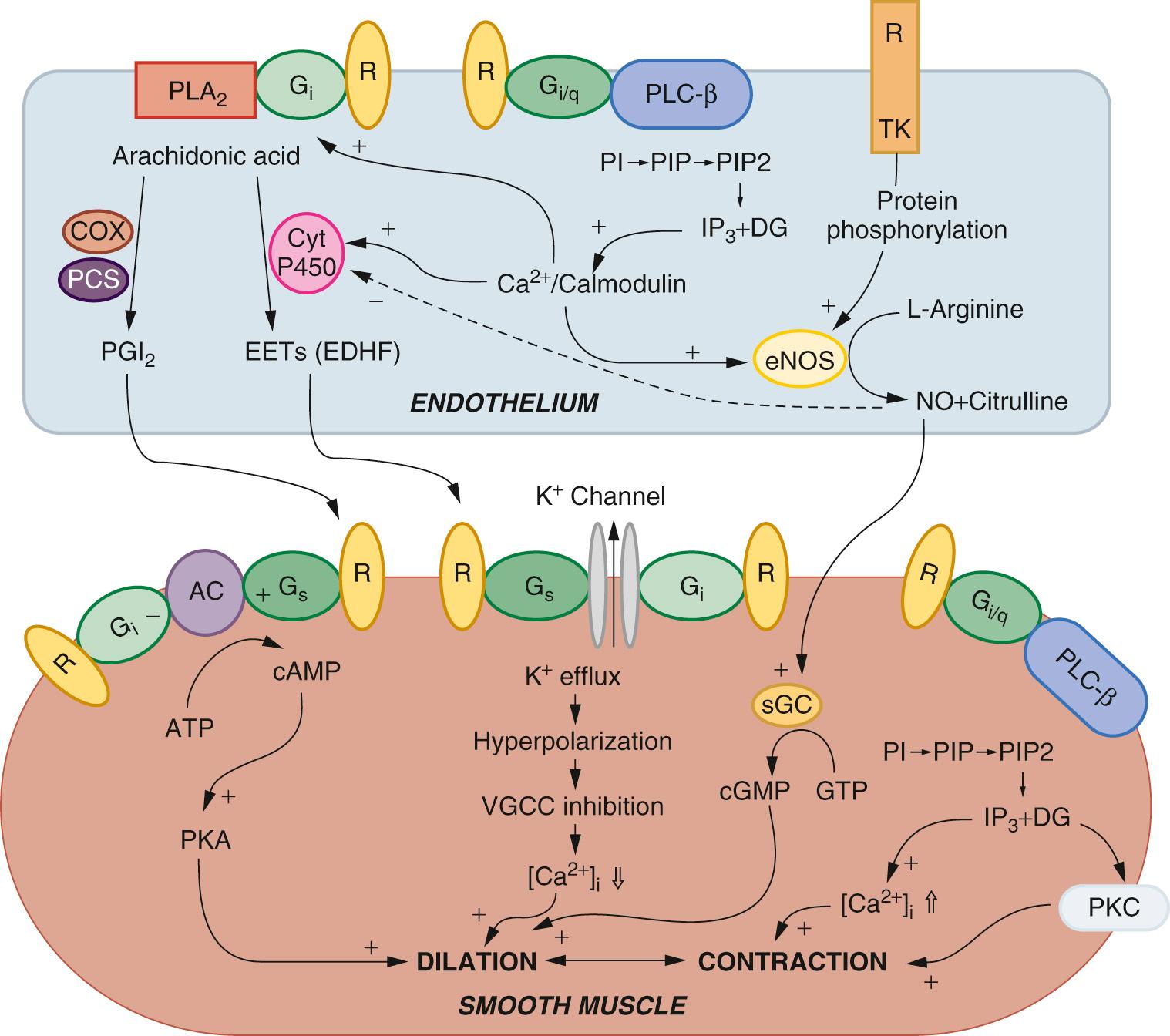
Although NO• is the major regulator of vascular tone, there are other factors that modulate endothelium-dependent vascular tone in coronary, pulmonary, and peripheral circulations. Endothelium-derived hyperpolarizing factor (EDHF) is an example. The endothelium-dependent hyperpolarization of vascular smooth muscle is mediated by the opening of a calcium-dependent potassium channel, leading to K+ exit from the cell. When the vascular smooth muscle is hyperpolarized, voltage-sensitive calcium channels are closed, leading to a reduction in intracellular calcium. The role of the various EDHFs probably varies depending on the vessel size, the species, and the vascular bed under consideration. It is likely that several EDHFs exist, but current evidence suggests that hydrogen peroxide and epoxyeicosatrienoic acid, a cytochrome p450 metabolite of arachidonic acid, play major roles. Hydrogen peroxide is formed by the mitochondria in response to shear stress and acetylcholine. The hydrogen peroxide not only opens large conductance potassium channels; it also activates protein kinase G, causing oxidation and dimerization. Prostaglandin synthesis by the endothelium also modulates tone in the microcirculation. The predominant prostaglandin produced by endothelial cells is prostacyclin. There is substantial interaction between NO•, EDHF, and prostacyclin. A major stimulus for release of these factors is shear stress, or the tangential force of fluid as it flows over the endothelium, resulting in flow-dependent vasodilation. Interestingly, the importance of NO• seems to decline and the role of the EDHF increases as blood vessels decrease in size. In addition, the production of EDHF may increase when NO• is low. The interaction of endothelial cells with vascular smooth muscle cells and the intermediates involved is outlined in Figure 48-7 .
The ability of a vascular bed to adjust its tone to maintain a constant flow during changes in perfusion pressure is termed autoregulation. This process is most effective in the coronary circulation when pressure is between 40 and 160 mm Hg. The subendocardium and subepicardium differ in the range of pressures over which autoregulation can be observed. In the subendocardium flow begins to decrease at pressures of less than 60 to 70 mm Hg, whereas in the subepicardium these decreases in flow occur at significantly lower pressures. Clinically, systemic arterial hypertension affects the range over which autoregulation occurs in the subendocardium, such that flow begins to decline at even higher pressures. Such a change in subendocardial perfusion pressure in the setting of hypertrophic myocardium increases the likelihood of subendocardial ischemia. Patients with systemic hypertension may have an increased lower limit of autoregulation and may be more likely to suffer brain ischemia during surgery, or other times, even at pressures sufficient to sustain adequate perfusion in patients with normal blood pressure.
The predominant changes in vasomotor tone, concerning both autoregulation and metabolic vascular regulation, occur in vessels smaller than 100 µm in diameter. The rate of oxygen consumption in the myocardium is closely related to myocardial perfusion via coronary microvascular tone. The ability of the myocardium to extract additional oxygen to meet increased demand is limited because myocardial oxygen extraction is already near its maximal threshold under resting conditions. To account for this limitation, coronary flow rises in response to increased myocardial oxygen requirements.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here