Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
While vaccine development, manufacturing, and delivery remain important components of a robust immunization system, vaccines only provide individual and societal benefits if eligible individuals can access and accept them. Therefore, it is important to understand and focus on the behavioral factors associated with vaccine uptake, in addition to addressing practical barriers. According to WHO Strategic Advisory Group of Experts working group on vaccine hesitancy, “Vaccine hesitancy refers to delay in acceptance or refusal of vaccination despite availability of vaccination services. Vaccine hesitancy is complex and context specific, varying across time, place and vaccines. It is influenced by factors such as complacency, convenience and confidence.” Increasingly, there is recognition that convenience or practical barriers to vaccination are important drivers of undervaccination that moderate vaccine behavior, separate from hesitancy or motivation, which is directly impacted by how people think and feel about vaccination and social processes.
In addition to vaccine hesitancy, there is a range of social and behavioral concepts associated with vaccine uptake. Vaccine confidence involves trust in the safety and efficacy of vaccines, the vaccine delivery system, including the reliability and competence of the health services and health professionals, as well as the motivations of the policymakers who decide on the needed vaccines. Other common vaccine-associated behavioral outcomes include vaccine uptake (percentage of a population having received a vaccine), vaccine demand (actions of individuals and communities to seek vaccines), vaccine acceptance (the degree to which individuals accept, question, or refuse vaccination), and vaccine refusal (unwillingness to allow oneself or a family member to be immunized). More formal definitions of these phenomena are described in Table 84.1 .
| Behavioral Concept | Definitions |
|---|---|
| Vaccine Hesitancy | Vaccine hesitancy refers to delay in acceptance or refusal of vaccination despite availability of vaccination services. It is complex and context specific, varying across time, place and vaccines. It is influenced by factors such as complacency, convenience and confidence. Concerns about the decision to vaccinate oneself or one’s children. Vaccine-hesitant individuals may accept all vaccines but remain concerned about them, they may refuse or delay some vaccines but accept others, or they may refuse all vaccines. Reluctance to receive recommended vaccination because of concerns and doubts about vaccines that may or may not lead to delayed vaccination or refusal of one, many, or all vaccines. The term “vaccine hesitancy” should be applied to those parents whose conscious deliberations demonstrate something akin to indecision. The inclusion of convenience is problematic, since much undervaccination arises from factors related to access or pragmatics that is not hesitancy. |
| Vaccine Confidence | Trust in (1) the effectiveness and safety of vaccines; (2) the system that delivers them, including the reliability and competence of the health services and health professionals; and (3) the motivations of the policymakers who decide on the needed vaccines. Vaccine confidence is the trust that parents, patients, or providers have in: recommended vaccines; providers who administer vaccines; and processes and policies that lead to vaccine development, licensure, manufacturing, and recommendations for use. Vaccine confidence concerns the belief that vaccination—and, by extension, the providers and range of private sector and political entities behind it—serves the best health interests of the public and its constituents. |
| Vaccine Demand | The actions of individuals and communities to seek, support, and/or advocate for vaccines and immunization services. |
| Vaccine Uptake | Vaccine coverage or uptake, which refer to the percentage of a population having received a vaccine, regardless of opportunity. Coverage/uptake is also often referred to as an immunization rate despite this measure representing prevalence and not a true rate. Vaccine uptake defined as the proportion of the eligible population who received a vaccine during a specific time period and “coverage” as the proportion of an eligible population that is vaccinated, regardless of when they received the vaccine. Vaccine uptake is used to refer to the proportion of a population that has received a specific vaccine. Vaccine uptake does not equal vaccine acceptance because it does not consider the opportunity to accept or refuse (i.e., in situations where access to vaccination services is problematic, low vaccine uptake does not equal low vaccine acceptance) or the fact that some may vaccinate despite having important doubts and concerns. |
| Vaccine Acceptance | The degree to which individuals accept, question, or refuse vaccination. , Vaccine acceptance is defined as the individual or group decision to accept or refuse, when presented with an opportunity to vaccinate. Vaccine acceptance represents a spectrum of behaviors and beliefs from rejection of all vaccines to active support of immunization recommendations. Accepters: those who agreed with or did not question vaccination. |
| Vaccine Refusal | Unwillingness to allow oneself or a family member to be immunized against a preventable contagious disease. It occurs most often in people who fear adverse effects from vaccination, in people who have religious or philosophical objections to vaccination, and in people who have had allergies, real or perceived, to a component of a vaccine. Vaccine refusal cannot be defined as a dichotomous behavior of acceptance versus refusal, but rather as a continuum between the two situations, with individuals who refuse all vaccines at one end, those who accept all vaccines at the other, and those who accept some but refuse others between the two groups. Rejecters: those who completely rejected vaccination. |
Reluctance to engage in immunity-related procedures has been a part of history even before Edward Jenner popularized vaccination. During the American revolutionary war, there was substantial transmission of smallpox in Boston. British soldiers were protected against the outbreak because most of them had been exposed to the virus in their childhoods. George Washington was concerned about the safety of inoculation—a procedure in which a small quantity of infectious material was transferred from a smallpox case to a noninfected individual to induce immunity in the latter. As a result of these concerns, George Washington initially relied on quarantine for containment of disease in his soldiers. However, after the military loss at Quebec in 1775–76, primarily attributed to smallpox, the revolutionary war general and Unites States’ first President decided to inoculate his Army. The rest, as they say, is history.
Jenner’s publication of his smallpox vaccination experiment occurred in a period of high smallpox rates and, hence, there was relatively broad early acceptance of the vaccine in England and many other countries, including the United States where the vaccine was introduced by a Harvard professor Dr. Benjamin Waterhouse at the turn of the 19th century.
However, in the 1850s, nonmainstream doctors and other practitioners led challenges to smallpox immunization. This opposition to vaccination came after a decrease in smallpox as a result of widespread vaccination between 1802 and 1840. Vaccination rates dropped in the context of the drop in the community risk of smallpox as well as opposition to the vaccine by vocal activists. Not surprisingly, there was a substantial smallpox resurgence the 1870s in the United States. In response to drops in vaccination rates and increasing smallpox cases, several states passed new vaccination laws while many other states started enforcing their existing laws.
These laws often had a backfire effect of increasing vaccine opposition and vaccine opponents were successful in repealing compulsory vaccination laws in states such as California, Illinois, Indiana, Minnesota, Utah, West Virginia, and Wisconsin. Overall, these 19th-century laws implemented compulsory vaccination rather than mandatory vaccination—a feature of most modern-day vaccine requirements. In mandatory vaccination, individuals are required to receive a vaccine or pay some sort of societal or financial price (e.g., loss of employment, restriction from on-site learning, loss of financial benefits etc.). In compulsory vaccination, individuals could be vaccinated against their will.
In the early part of the 20th century there was legislative focus on state and federal pure food laws resulting in an overlap in interests of the vaccine opponents and largely unregulated patent medicine manufacturers. Like modern vaccine opponents, the antivaccine movement in the United States at the turn of the 20th century was composed of those who saw vaccination—particularly compulsory vaccination—as an infringement on personal freedoms, as well as patent medicine manufacturers (analogous to many modern-day “natural” supplement manufacturers), parents of children with real or perceived vaccine adverse events, and some alternative medicine practitioners.
By the fourth decade of the 20th century, vaccine opposition had fizzled out. This decrease in intensity of vaccine opposition has been attributed to improvement in vaccination practices, an increase in the proportion of vaccinations delivered by trained medical practitioners, and more state and federal control over public health.
The modern antivaccination movement arose in the 1970s when groups in many western countries started voicing concerns about whole-cell pertussis vaccines. Another important vaccine safety related event was the so-called swine flu scare. The Swine Influenza Immunization Program was launched in January 1976 in response to an outbreak of swine influenza among military trainees at Fort Dix, New Jersey, , which led to panic due to concerns about an influenza pandemic. This program was discontinued within the same year after reports of cases of Guillain-Barré syndrome thought to be associated with the swine influenza vaccine.
A significant event in the antivaccine discourse in the United States was the airing of the documentary called “DPT: Vaccine Roulette” on Washington, DC area NBC affiliate in 1982. The documentary promoted misinformation regarding a purported link between the pertussis component of the DTP vaccine and brain damage. This documentary proved to be a nudge for a few well-connected Washington, DC area parents to come together to form Dissatisfied Parents Togethers (DPT), later renamed the National Vaccine Information Center. Throughout the last part of the 20th century several organizations were established by US antivaccine activists.
It was in this environment that Andrew Wakefield, a British surgeon who gave up clinical practice to focus on research, published a since retracted Lancet paper on 12 children with a false (and, as it turned out, fraudulent) nonexistent connection between autism and the MMR vaccine. The paper turned out to be a metaphorical shot in the arm for those who were skeptical about childhood vaccination. Many large studies and independent reviews have since found no causal association between MMR and autism.
In recent years, vaccine opposition in the United States has been characterized by use of social media for dissemination of messages opposing vaccines. Mapping of the views of 100 million Facebook users associated with the topic vaccine found that among the users with undecided, antivaccination, and pro-vaccination views grouped within clusters, the antivaccination clusters were smaller in size than pro-vaccination clusters but were central in the network, heavily entangled with undecided clusters, and showed the highest growth. Of most concern, the pro-vaccination clusters were peripheral, in the smaller network patches, and not engaging with the antivaccination or undecided groups, unable to influence the conversation. As such, social media platforms such as Facebook enable negative views online to become pervasive and exist in echo chambers, often with little interaction with pro-vaccination views. Vaccine skeptics have also been active in opposing COVID-19 vaccines.
While the antivaccine movement and vaccine hesitancy has been studied most closely in the United States, these are not uniquely U.S. phenomena. In fact, similar patterns of historical vaccine opposition re-emerging in the 1970s have been observed in countries such as the UK, Australia, France, and Italy, to name a few. While vaccine opposition is less well organized in low-income countries, vaccine hesitancy in significant minority of the population is a global phenomenon. In a large-scale analysis of 290 surveys conducted in 149 countries between 2015 and 2019, while there was heterogeneity in the level and determinants of hesitancy between countries, vaccine hesitancy was present in every region of the world. Similarly, a multi-country study of COVID-19 vaccine acceptance in low- and middle-income countries and Russia and the United States showed that while overall acceptance of vaccines was higher in low- and middle-income countries (compared to the United States and Russia), there were many low- and-middle income countries with high levels of hesitancy for COVID-19 vaccines.
While vocal vaccine deniers and active promoters of vaccine skepticism feature prominently in public discourse in many countries, they are a small minority in most countries.
Vaccine hesitancy and refusal have been associated with vaccine-preventable outbreaks and have hampered disease control and eradication programs such as the COVID-19 vaccination program and the polio eradication program. For example, in systematic reviews of measles cases after it was eliminated in the United States in 2000, among cases who were unvaccinated despite being vaccine eligible, more than 70% had nonmedical exemptions (e.g., exemptions for religious or philosophical reasons). , Moreover, while recent pertussis resurgences have been related to waning immunity and other factors, vaccine refusal was still associated with an increased risk for pertussis in some populations.
Globally, vaccine hesitancy and refusal have hampered polio eradication efforts. For example, in 2003, as the world was getting close to polio eradication, many clerics and other individuals boycotted the polio vaccine in Northern Nigeria due to multiple political, cultural, and socioeconomic factors. This boycott spread and led to increase in vaccine hesitancy in the region of Nigeria and beyond. It is hard to say if the world would have eradicated polio by now if the Nigeria boycott had not happened. However, it is indeed documented that cases arising following the boycott were linked to exportation of the virus to other countries, undermining eradication efforts for several years.
Vaccine hesitancy is not a binary phenomenon. It is a continuum ranging from pro-vaccination advocacy, to active demand, passive acceptance, hesitancy, outright refusal, and, in a few cases, vocal vaccine denial ( Fig. 84.1 ). , Underpinning these positions are people’s values and worldviews; trust in providers, medical establishment, government, and the pharmaceutical industry; perception of risk; and ability to access the vaccine.
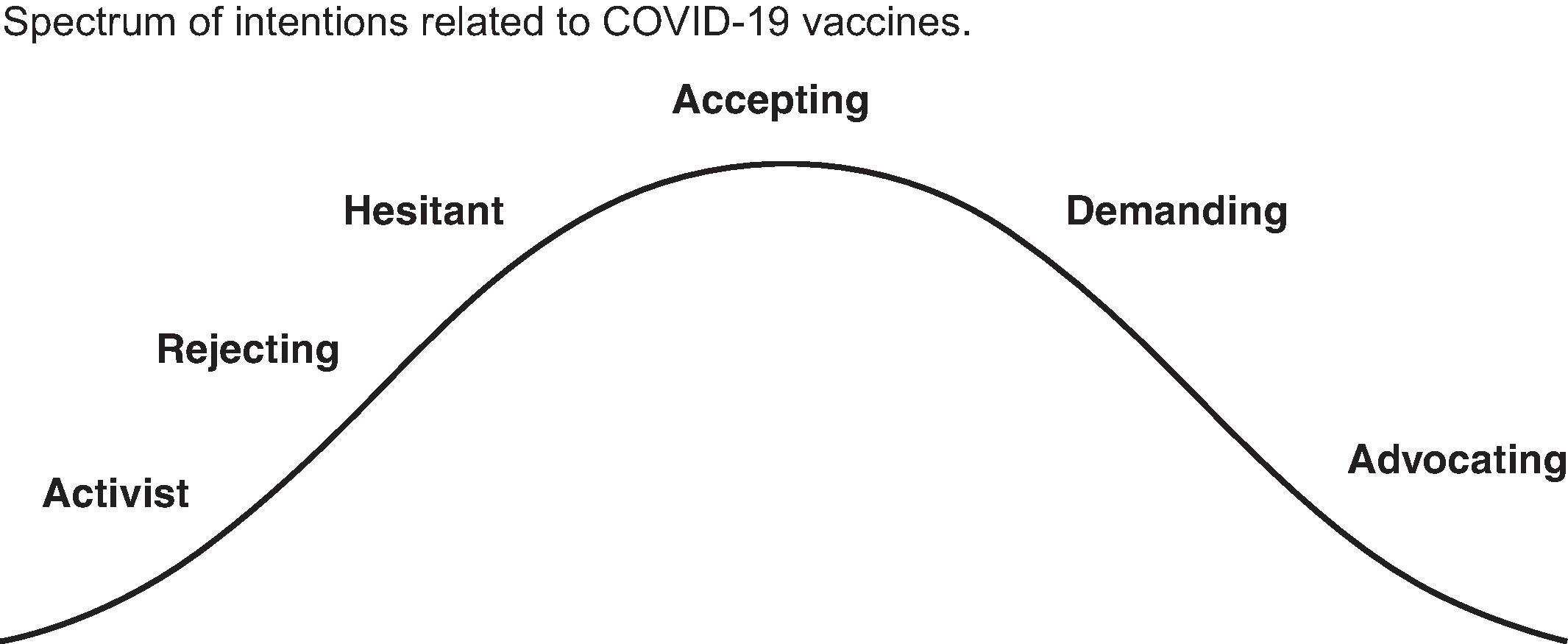
The goal of effective vaccine communication is to tailor the conversation or approach to where the individual is on the vaccine hesitancy-acceptance spectrum. Vaccine-hesitant individuals may already be vaccinating despite significant concerns, or they may be selectively vaccinating or delaying vaccination. Trust in the healthcare provider is key, and as such, time spent with these individuals addressing concerns may move them toward vaccine acceptance, whereas vaccine refusers are often the hardest to budge. Vaccine refusers often hold firmly entrenched religious, philosophical or alternative lifestyle beliefs, and may have had negative experiences with vaccination. Vaccine acceptors, although wanting to vaccinate, may still be influenced by disinformation or loss of trust in the health system and may subsequently slide back along the continuum.
While achieving high vaccine uptake is a primary public health goal, understanding and measuring the factors that drive uptake are critical. Such factors as risk perceptions, beliefs, attitudes, subjective norms, and knowledge are outlined in widely accepted theories of health behavior. Other factors such as confidence, trust, and values have been shown to be linked to vaccination. Most countries rely on vaccine coverage figures to monitor vaccination programs, which cannot distinguish between these behavioral determinants. Measuring behavioral factors (in addition to vaccine coverage) allows policymakers, immunization program managers, and funders to monitor vaccine confidence, identify target populations, provide consistent and comparable data over time, and inform and evaluate cost-effective strategies to optimize vaccine coverage across the life span. Several measurement instruments have been developed for different populations, settings, and vaccines.
The largest group of measures focuses on childhood vaccine confidence. They do not incorporate items to measure access factors or practical issues, such as vaccine supply, cost of vaccination, or barriers to travel and time to access services. More comprehensive measures of the barriers to childhood vaccination, including both acceptance and access factors, are under development. These include the WHO-led Measuring Behavioral and Social Drivers of vaccination (BeSD) tools and associated user guidance, and the Vaccine Barriers Assessment Tool (VBAT), being developed in Australia and New Zealand. The BeSD tools aim to measure the range of factors that influence children’s vaccination across low-, middle- and high-income contexts. In addition to an adaptable quantitative survey instrument, the BeSD tools also include guidance for applying qualitative methods to provide a more in-depth and contextualized understanding of how people perceive and experience vaccination for their children. The VBAT aims to develop a validated tool that is (1) brief, accurate, and predictive of uptake to inform targeted interventions and campaigns; and (2) able to both robustly measure and monitor vaccine acceptance and identify the practical barriers limiting access to vaccine.
At present, there are at least 14 general vaccine confidence measures for childhood vaccination (published between 2010 and 2019) that were all developed in high-income countries (HICs), except the Caregiver Vaccination Attitudes Scale, which was developed in Ghana. There are a number of commonly used measures, but The Parent Attitudes about Childhood Vaccines (PACV) is the most validated measure (n = 10 studies), with the other 13 measures having a mean of 1.4 studies per measure ( Table 84.2 ).
| Name of Measure/Authors | Year | Country | Conceptual Basis | Constructs | Number of Items | Number Validation Studies |
|---|---|---|---|---|---|---|
| 1. Parent Attitudes about Childhood Vaccines (PACV) survey Opel et al. |
2011 | USA HIC |
Health Belief Model | 1. Safety and efficacy (4 items) 2. General attitudes (9 items) 3. Behaviour (2 items) |
15 items in long form, 5 items in short form | 10 |
| 2. Vaccine Confidence Scale (VCS) Gilkey et al. |
2014 | USA HIC |
Health Belief Model | 1. Benefits of vaccination (4 items) 2. Harms of vaccination (2 items)3. Trust in healthcare providers (2 items) |
8 items in long form, 4 items in short form | 3 |
| 3. Vaccine Hesitancy Scale (VHS) The SAGE Working Group on Vaccine Hesitancy, WHO |
2015 | Switzerland HIC |
Health belief Model and Theory of Planned Behaviour; gaps in these models also identified | 1. Confidence (7 items) 2. Risks (2 items) |
10 items (9 in subsequent validation) | 1 |
| 4. 5C Antecedents of Vaccine Acceptance (5C) Betsch et al. |
2018 | Germany HIC |
Health Belief Model, Theory of Planned Behaviour, 3Cs, 5As | 1. Confidence (1 or 3 items) 2. Constraints (1 or 3 items)3. Complacency 1 or 3 items)4. Calculation (1 or 3 items)5. Collective Responsibility (1 or 3 items) |
15 items in long- form and 5 items in short form | 1 |
| 5. Caregiver Vaccination Attitudes Scale (CVAS) Wallace et al. |
2019 | Ghana LMIC |
Not reported | 1. Vaccine benefit (2 items) 2. Past vaccination behavior (2 items)3. Vaccine efficacy and safety (2 items) |
6 items | 1 |
Up to five constructs are included in each of the tools, including (1) beliefs in the benefits or importance of vaccination; (2) trust in vaccines, healthcare providers, the vaccine schedule, and the legitimacy of authorities to require vaccination; (3) perceived vaccination harms; (4) perceived risks of infectious disease; and (5) collective responsibility. Each construct is generally assessed using at least one or two items or questions. Psychometric validation and replication, which is important to ensure that these tools measure what they are designed to measure, have been limited for most measures. Of the 14 measures, most studies examined internal consistency (how well the items measure what they are meant to measure; n = 13), criterion-related validity (correlation with vaccination intentions or behavior; n = 12), and factor structure (n = 11), with fewer studies examining convergent and discriminant validity (the way constructs are related or dissimilar; n = 7). Very few studies have used cognitive interviewing to confirm the meaning that participants ascribe to survey items matches that intended by the researchers (n = 3) or assessed test-retest reliability (n = 3).
Several instruments have been developed to measure factors related to human papillomavirus (HPV) vaccination for adolescents, often drawing from the Health Belief Model (HBM). The Carolina HPV Immunization Attitudes and Beliefs Scale (CHIAS) measures parents’ attitudes and beliefs about HPV vaccines for their adolescent children. The original CHIAS and a modified version have been validated among parents, and it has also been adapted for use with adolescents themselves. Other measures based on the HBM include the Health Belief Model Scale for HPV and its Vaccination (HBMS-HPVV) —in Turkish—and the Parental Human Papillomavirus Survey (PHPVS). The Treatment Self-Regulation Questionnaire measures parental motivation for HPV vaccines in Spanish and English, while the HPV Adolescents Vaccination Intervention Questionnaire (HAVIQ) scale measures adolescents’ knowledge and experiences of HPV vaccination in school. At least one attempt to adapt and validate the PACV for use with adolescent vaccination was unsuccessful, highlighting the risks of adapting existing validated measures and the importance of conducting validation studies in a range of different populations.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here