Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The success and evolution of liver transplantation as a therapeutic treatment for patients with advanced liver disease led to a National Institutes of Health–sponsored Consensus Development Conference, which recommended that a “registry or clearinghouse be established for collection and evaluation of all available data on liver transplantation.” The National Institute of Diabetes and Digestive and Kidney Diseases–sponsored Liver Transplantation Database was subsequently established in 1985 for the purpose of developing a database to collect information on candidates for liver transplantation and information about recipients and their donors, the operation, and sequelae. The National Organ Transplant Act of 1984 mandated a national registry of all solid organ transplantations performed in the United States. In 1987 the United Network for Organ Sharing (UNOS), in collaboration with four existing solid organ transplantation registries (kidney, liver, heart, and pancreas) began operating the Scientific Registry of Transplant Recipients (SRTR). The registry exists to support the ongoing evaluation of the scientific and clinical status of solid organ transplantation, including kidney, heart, liver, lung, intestine, and pancreas. Data in the registry are collected by the Organ Procurement and Transplantation Network (OPTN) from hospitals and organ procurement organizations across the country. The SRTR contains current and past information about the full continuum of transplant activity, from organ donation and waiting list candidates to transplant recipients and survival statistics. Transplantation is a data-driven field. The establishment of a comprehensive registry with 25 years of data on candidates, donors, and recipients has allowed the field of transplantation to move forward with evidence-based medicine as the pillar of policy development and implementation.
This chapter will attempt to present an overview of trends in liver transplantation in the past 25 years with a focus on the past 10 years. One of the most notable developments in the field of liver transplantation in the past decade has been the development and implementation of the Model for End-Stage Liver Disease (MELD) score for adults and Pediatric End-Stage Liver Disease for children in 2002 in regard to allocation of cadaveric livers for these patient groups. This system ranks patients according to their risk for dying from their liver disease. The change to this allocation scheme resulted in a number of changes in the trends of liver transplantation, which had been consistent up until the implementation of MELD in February 2002. This chapter will highlight and focus on trends in the past 10 years and try to describe the impact of the MELD system on the waiting list, outcomes, and types of patients transplanted. This chapter will focus mainly on adult patients. Numerous other external forces have resulted in changes in the dynamics of liver transplantation over the past decade. Some of these forces will be addressed in an effort to give the reader a more comprehensive understanding of the shifting landscape of the field of liver transplantation. Much but not all of the data presented is a product of the annual report of the SRTR.
Effective February 27, 2002, adult liver transplant candidates are placed on the waiting list in descending order according to their MELD score. This score is derived from the candidate’s total bilirubin level, creatinine level, and the international normalized ratio for prothrombin time. The score starts at 6 and is capped at 40 and is a measure of 90-day mortality related to the candidate’s liver disease. Before this allocation system, candidates were listed according to more subjectively defined statuses that also incorporated waiting time as part of the allocation algorithm. The MELD system uses waiting time only when two or more patients have the same MELD score.
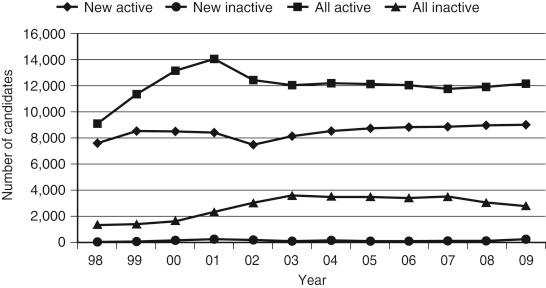
With the adoption of the MELD system there was a significant reduction in the number of waiting list registrations ( Fig. 99-1 ) because the need to accrue waiting time was abated. Subsequently the number of candidates on the waiting list has remained stable year after year. The age distribution of candidates on the waiting list for a liver transplant has changed over the past decade, with an increased proportion of the list being composed of patients in the 50- to 64-years age-group ( Fig. 99-2 ). This trend may be a consequence of the natural history and epidemiology of liver disease in the United States.
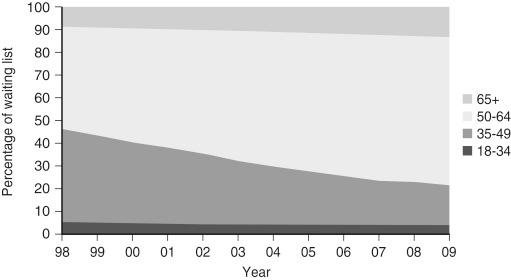
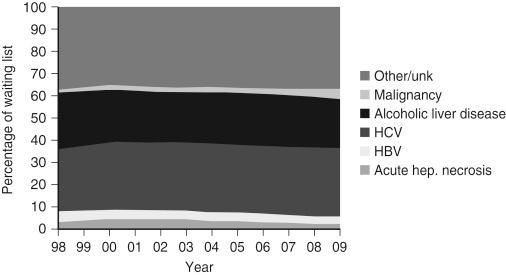
End-stage liver disease from chronic hepatitis C virus infection continues to be one of the most common causes for candidates on the waiting list ( Fig. 99-3 ). The long incubation time from infection to advanced cirrhotic liver disease is often decades and therefore becomes most manifest in patients in the 50- to 64-year-old group. The other large disease group of patients on the waiting list is other/unknown. This group likely includes a large group of patients with cryptogenic cirrhosis. The cause of liver disease in this group is more often related to fatty liver disease or nonalcoholic steatohepatitis.
The vast majority of patients on the waiting list for a liver transplant have relatively low MELD scores, which correspond with generally stable liver disease. Table 99-1 shows a snapshot of patients on the waiting list at the end of each year. It is worthwhile to note that there has actually been a decrease in the number of patients in the group with MELD scores of 6 to 10, which likely reflects the growing understanding that patients in this group with a low mortality risk generally do not derive a survival benefit from liver transplantation. The relatively small number of patients with higher MELD scores—21 to 30, and above 30—is a reflection of the consequence of the allocation scheme. This is a “sickest-first” algorithm, and thus most transplants occur in patients with MELD scores in these ranges.
| Patient Status | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 14 | 13 | 20 | 28 | 14 | |||||
| 1A | 11 | 3 | 6 | 1 | 5 | |||||
| 1B | 6 | 6 | 10 | 6 | 11 | |||||
| 2A | 62 | 127 | ||||||||
| 2B | 2,921 | 2,938 | ||||||||
| 3 | 10,918 | 11,810 | ||||||||
| MELD 6-10 | 5617 | 5085 | 4935 | 5095 | 4972 | 4799 | 4685 | 4412 | ||
| MELD 11-14 | 3711 | 3864 | 4002 | 4006 | 3958 | 3686 | 3649 | 3654 | ||
| MELD 15-20 | 2390 | 2366 | 2411 | 2385 | 2378 | 2361 | 2434 | 2589 | ||
| MELD 21-30 | 477 | 448 | 489 | 433 | 415 | 474 | 567 | 638 | ||
| MELD > 30 | 49 | 60 | 60 | 54 | 51 | 60 | 60 | 78 | ||
| HCC T1 | 72 | 58 | 8 | 5 | 5 | 4 | 4 | 3 | ||
| HCC T2 | 181 | 211 | 244 | 307 | 307 | 377 | 382 | 574 | ||
| Other Exceptions | 108 | 176 | 191 | 199 | 199 | 248 | 292 | 334 | ||
| Total | 13,915 | 14,888 | 12,635 | 12,296 | 12,354 | 12,501 | 12,294 | 12,025 | 12,080 | 12,298 |
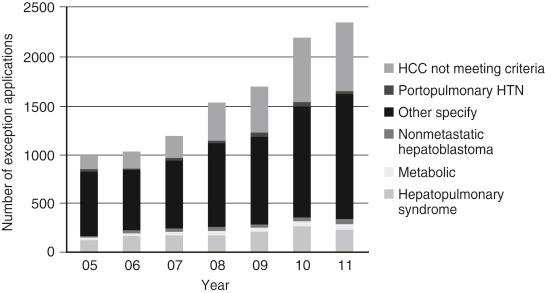
It is noteworthy that there has been an increasing number of patients with hepatocellular cancer (HCC) T2 lesions over the past decade. With adoption of the MELD system, patients with HCC that meet T2 or Milan criteria were granted additional MELD priority points. These “exception points” have been adjusted down over the first 3 years of the MELD system, and points for T1 lesions were abolished ( Fig. 99-4 ). If a patient is not transplanted in the first 3 months of being active on the waiting list, he or she is granted additional exception points as long as the patient meets the standard criteria. Over time there have been an increasing number of patients on the waiting list with the diagnosis of HCC.

With the adoption of MELD there was also a mechanism by which a physician could petition a group of peers, the regional review board (RRB), to grant additional MELD points to his or her patient if the physician felt that the patient’s risk for death was not represented by his or her calculated MELD score. Over time there has been an increase in the number of patients with exception scores, as shown in Table 99-1 . This trend is driven in part by an increasing number of HCC patients that do not meet the standard T2 criteria ( Fig. 99-5 ). This follows the recognition that carefully selected patients with larger tumor burden (T3) may benefit from transplantation with acceptable outcomes.
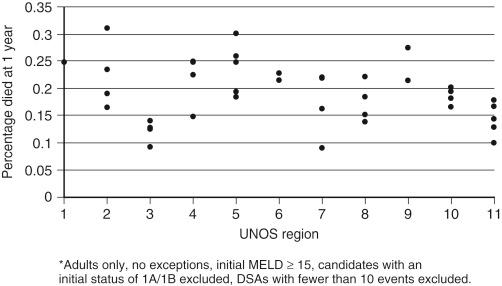
Patients often remain on the waiting list until transplanted or sometimes until death. Liver transplantation is intended to be a lifesaving procedure, and patients are ranked according to their risk for dying (MELD score). Death rate is a measure of mortality risk over time. Table 99-2 shows the death rate for various groups over the past decade. The adoption of MELD in 2002 lead to a more objective measure of mortality risk. However, the previous system with more subjectivity was not inaccurate, as can be seen by death rates in the status 2A, 2B, and 3 patients. Accordingly, with increasing MELD score there is an increased death rate that remains fairly constant over time. Of note, the death rates for patients on the waiting list with HCC are quite low because these patients do not frequently die from their liver disease. However, progression of their underlying malignancy beyond criteria may lead to removal from the waiting list. Also noteworthy is that patients with an exception score have very low death rates comparable to patients in the category of MELD scores of 11 to 14. The discrepancy between supply and demand of donated livers is one of the drivers of death rates. This discrepancy is variable across the country, and hence the death rates are variable. As seen in Figure 99-6 , there is disparity within and across regions in regard to rates of death.
| Patient Status | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 715 | 8482 | 6404 | 5494 | 3096 | 9484 | ||||
| 1A | 5397 | 3849 | 4849 | 2761 | 8021 | |||||
| 1B | ||||||||||
| 2A | 6159 | 4033 | 3701 | |||||||
| 2B | 203 | 199 | 444 | |||||||
| 3 | 60 | 63 | 190 | |||||||
| MELD 6-10 | 19 | 38 | 37 | 36 | 37 | 36 | 33 | 31 | ||
| MELD 11-14 | 28 | 71 | 69 | 73 | 67 | 72 | 57 | 59 | ||
| MELD 15-20 | 107 | 158 | 166 | 156 | 143 | 125 | 133 | 124 | ||
| MELD 21-30 | 666 | 805 | 747 | 733 | 733 | 605 | 668 | 550 | ||
| MELD >30 | 5945 | 4990 | 5074 | 4624 | 3924 | 3858 | 3780 | 4488 | ||
| HCC T1 | 71 | 30 | 72 | 213 | ||||||
| HCC T2 | 75 | 135 | 120 | 112 | 106 | 73 | 62 | 70 | ||
| Other Exceptions | 33 | 109 | 88 | 83 | 97 | 75 | 61 | 38 | ||
| Total | 136 | 137 | 130 | 129 | 131 | 130 | 122 | 114 | 114 | 113 |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here