Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Congenital heart diseases (CHDs) are the most common severe congenital malformations, affecting 0.8% to 1% of newborns. Approximately half of the CHDs are severe defects. The overall mortality of a CHD diagnosed prenatally ranges from 25% to 35%, and about 15% of children born with a CHD die before they reach adolescence.
Overall, the risk of associated chromosomal aneuploidy lies between 15% and 30%, with an additional risk of other genetic anomalies, including microdeletions and microduplications, between 5% and 7%. A fetal CHD increases the risk of other extracardiac malformations 10-fold, therefore 25% to 40% of fetuses with a CHD will have an extracardiac malformation.
Most CHDs (>90% of cases) occur in fetuses with no history or known risk factor. Prenatal ultrasound (US) screening programs are essential for the detection and diagnosis of CHDs, allowing a correct evaluation of prognosis, management of pregnancy, and a delivery plan. Prenatal diagnosis is particularly relevant in those CHD where postnatal clinical evolution is dependent on the patency of the ductus arteriosus.
The heart is an organ with three connections on each side. On the left side, the pulmonary veins reach the left atrium, which communicates with the left ventricle and the aorta. On the right side, the superior vena cava and inferior vena cava drain into the right atrium, which connects with the right ventricle and the pulmonary artery. A complete cardiac US examination should visualize all these connections (including the morphology, size, and function of the different components) and the ductal and aortic arches.
Several cardiac planes or views constitute the basic echocardiographic study at 19 to 22 weeks' gestation. The advanced echocardiographic study includes further sections and is reserved for high-risk patients. The planes or views of a basic cardiac scan can be performed from the first trimester of pregnancy and include ( Fig. 74.1 ):
examination of the upper abdomen
four-chamber view
five-chamber or left ventricular outflow tract view
short-axis or right ventricular outflow tract view
three-vessel and trachea view
The long-axis view of the right ventricle ( Fig. 74.2 ) and other sagittal views, which include the cavoatrial junction view ( Fig. 74.3 ) and the aortic arch view ( Fig. 74.4 ), can be considered part of the advanced echocardiographic study ( Table 74.1 ).


| MATERNAL INDICATIONS |
|
| FAMILIAL INDICATIONS |
|
| FETAL INDICATIONS |
|
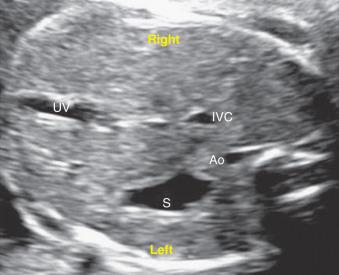
The upper abdomen view ( Fig. 74.5 ) detects situs abnormalities, which are frequently associated with heart malformations. As a starting point, the fetal position and the right and left sides of the fetus should be established. In a cross-sectional plane, the stomach and the descending aorta are located on the left side of the fetus and the liver and the inferior vena cava are on the right. The umbilical vein enters the liver and continues toward the right into the portal sinus. The transducer has to be moved slightly cranially to obtain the four-chamber view. During this movement, the connection of the inferior vena cava to the right atrium can be checked.
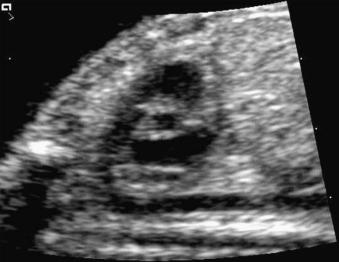
The four-chamber view ( Fig. 74.6 ) can be easily obtained as a transverse view of the thorax at the level of the fourth rib ( Fig. 74.6A ) and permits the widest range of detection of CHD (major CHDs affecting the atria, ventricles, atrioventricular valves, and interventricular and interatrial septa can be identified in this plane). The study of the four-chamber view includes:
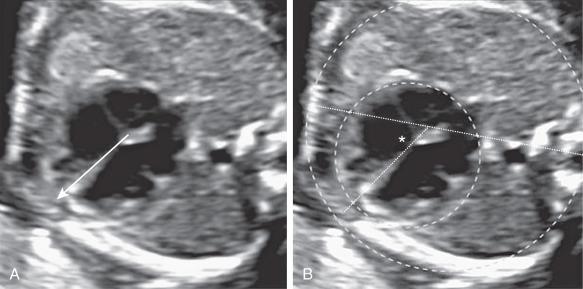
Position of the heart in the thorax: in normal levocardia, two-thirds of the heart is on the left, and the heart axis is pointing to the left (see Fig. 74.6 ).
Cardiac axis: compared with the sagittal axis, the cardiac axis is at 45 ± 20 degrees (see Fig. 74.6 ).
Size of the heart: the normal area of the heart is less than one-third of the thoracic area, and the transverse diameter of the heart at the level of the atrioventricular valves is less than one-half of the transverse diameter of the thorax (see Fig. 74.6 ).
Rhythm: a regular rate between 120 beats/min and 160 beats/min should be confirmed.
Contractility: the synchronous contraction of both atria and ventricles should be confirmed.
Evaluation of the presence of pericardial effusion: pericardial effusion is physiologic if less than 2 mm and the atrioventricular level is not exceeded.
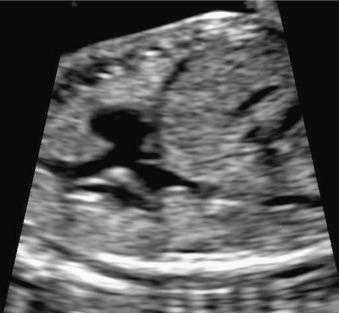
Confirmation of the existence of four chambers and evaluation of the symmetry between the atria and the ventricles: both atria are nearly equal in size. The lumen of the left ventricle is longer than the lumen of the right ventricle and reaches the apex of the heart. The right ventricle has a short lumen mainly because of the presence of the moderator band, a septomarginal trabeculum coursing from the interventricular septum to the lower free wall of the right ventricle ( Fig. 74.7 ).
Assessment of the position of the left and right sides of the heart: the right ventricle appears as the most anterior cardiac structure, and the left ventricle is posterior to the right ventricle and the most left-sided cardiac structure. The right ventricle is trabeculated, and its cavity is irregular, whereas the inner shape of the left ventricle is smooth. As mentioned, the right ventricle can be recognized by the presence of the moderator band. The left atrium is the most posterior cardiac chamber and is recognized by the connections of the pulmonary veins and the leaflet of foramen ovale, which bulges into it. The descending aorta is a circular pulsating structure positioned anterior-lateral to the spine and behind the left atrium (see Fig. 74.7 ).
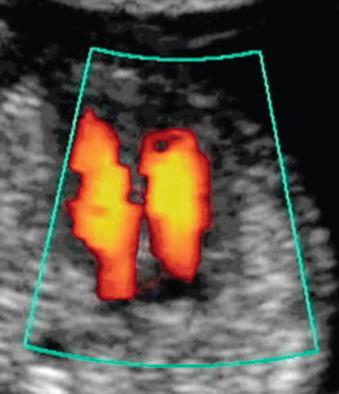
Confirmation of the pulmonary venous drainage to the left atrium: color Doppler can help identify the superior and inferior pulmonary veins ( ).
Assessment of the correct implantation of the two atrioventricular valves : it is another important feature to distinguish both ventricles ( Fig. 74.8 ). Both valves are implanted separately in the interventricular septum. The tricuspid valve is slightly more apical. This leaves a space between the insertions, the atrioventricular septum, which separates the right atrium from the left ventricle.

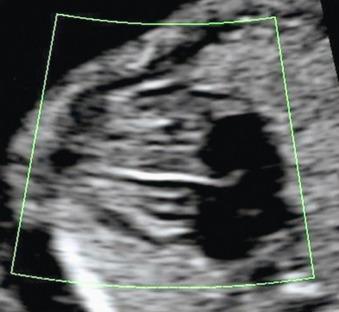
Assessment of function of the atrioventricular valves: it is important to confirm that both valves open freely during diastole (the cine-loop function can be useful for this) and close correctly during systole (absence of regurgitation evaluated by color Doppler) ( Fig. 74.9 ).
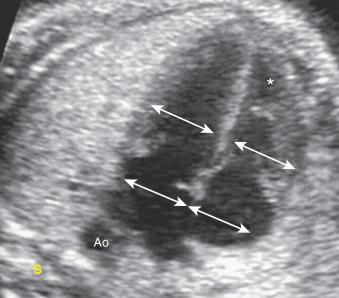
Evaluation of the interventricular septum: the long axis four-chamber view and the application of color Doppler allow a better evaluation of the septum ( Fig. 74.10 ).
Assessment of the interatrial septum: the septum primum and foramen ovale (with its flap that freely moves into the left atrium) should be identified ( Fig. 74.11 ).

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here