Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Primary degenerative arthritis of the elbow is discussed in detail in Chapter 76 . Over the years the etiology has been clarified, and the treatment trend is early intervention with arthroscopic débridement (see Chapter 21 ). Later stages may need to be managed with some form of prosthetic replacement (see Chapters 87 and 95 ).
The existence of primary degenerative arthritis of the elbow has been recognized since the early 1970s as a condition arising from “hard usage.” Kashiwagi et al. correctly considered this an overuse condition, clearly defined the radiographic characteristics, and suggested a means of treatment termed the Outerbridge-Kashiwagi (OK) arthroplasty. In fact, the condition is now well recognized as an overuse manifestation. However, other predisposing conditions may exist, such as osteochondritis dissecans. Unlike all other joints, primary osteoarthritis of the elbow is uncommon, accounting for only 1% to 2% of patients presenting with elbow arthritis. This is consistent with the observation that less than 5% of joint replacement is performed in patients with this diagnosis. Furthermore, recognition of the true nature of the entity is still sometimes overlooked or misinterpreted as a posttraumatic condition. With increased awareness, there is some evidence that the actual incidence of the disease may also be increasing.
Men are more commonly affected, at a ratio of about 4 to 1. The age at initial presentation is about 50 years, but this author and others have observed a surprising variation ranging from 20 to 65 years. Occupations or avocations involving repetitive use are identified in about 60% of patients. We have diagnosed this problem in persons with neuropathic conditions causing impaired ambulation and requiring continued use of crutches or a wheelchair. The dominant extremity is involved in about 80% to 90% of patients, and bilateral involvement is present in 25% to 60% of patients. The radiohumeral joint is involved in about 85%, but it may not be symptomatic. When involved, pain is localized laterally in flexion, extension, and rotation. Consensus does not exist regarding management of predominantly radiohumeral symptomatology. Stiffness may be a dominant feature. Loss of extension is the most common problem prompting medical attention. Posterior pain at terminal extension is present in virtually all patients and at terminal flexion in about 50% of patients. Less commonly, symptoms are present throughout the arc. The intensity of pain is mild to moderate, and only occasionally is the process described as severe.
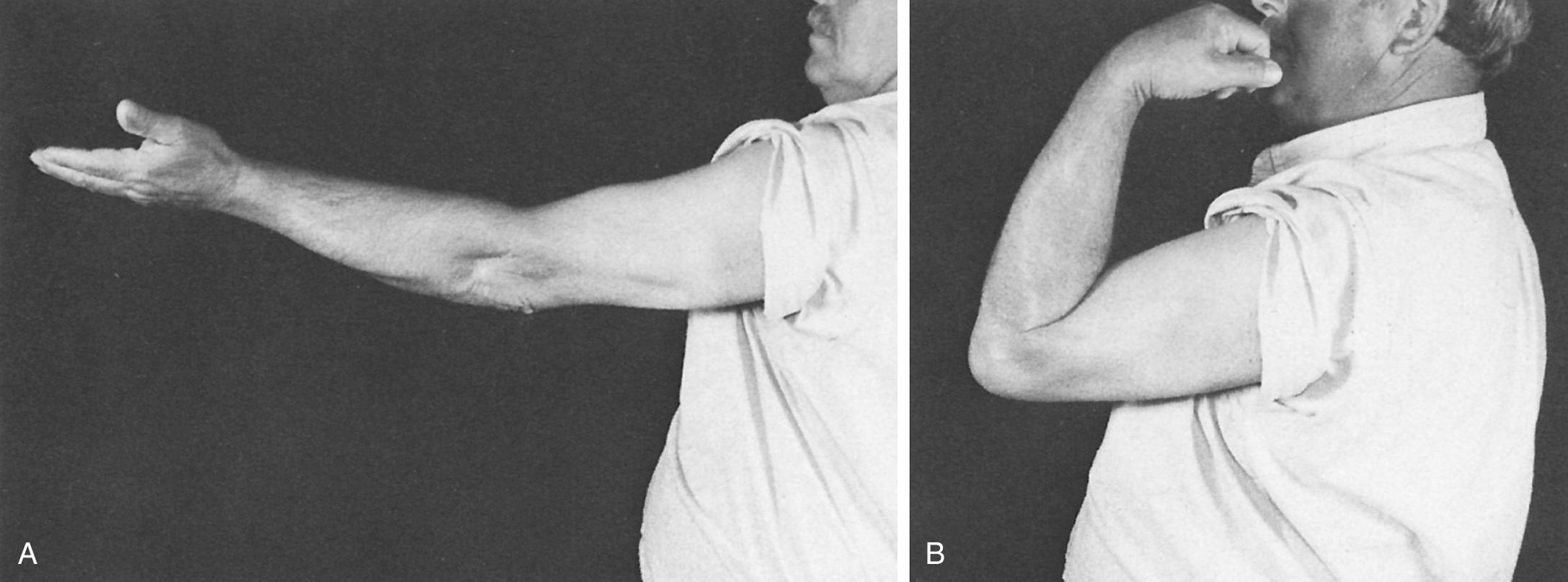
Examination reveals an arc of motion that averages about 30 to 120 degrees ( Fig. 111.1 ). Forearm rotation is not restricted or only minimally so because the radiohumeral joint is typically not severely involved. Ulnar nerve irritation has been reported in 10% but is probably underrecognized. Ulnar nerve involvement should be specifically assessed because ulnar nerve symptoms adversely affect the outcome of treatment.
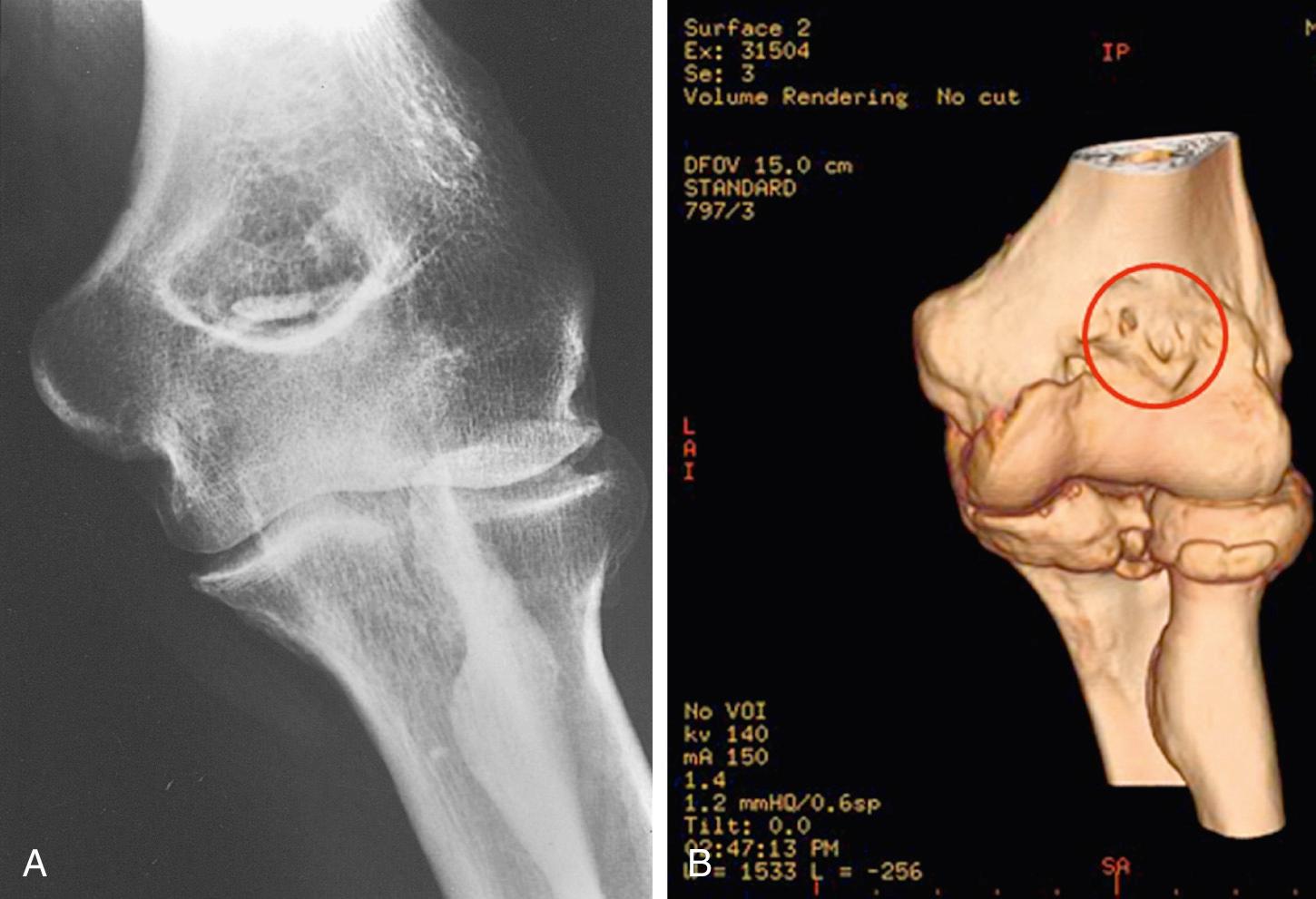
Because the diagnosis is obvious, special studies are unnecessary. The roentgenographic features of this condition are classic and maybe even monotonous. The characteristic of primary osteoarthritis of the elbow is “marginal osteophyte formation.” Hence, the anteroposterior and lateral roentgenograms consistently reveal an osteophyte of the coronoid and of the olecranon process ( Fig. 111.2 ). The anteroposterior view consistently shows osteophyte formation in the olecranon and/or coronoid fossae ( Fig. 111.3 ). Today a three-dimensional reconstruction clearly defines the osteophytic development at the margin of the articular surfaces of the humerus and ulna; hence the author refers to this as a “marginal disease” ( Fig. 111.4 ). Involvement of the radial head has been documented in about 85% of cases, and loose body formation is common, further justifying computed tomography (CT) imaging, which also makes a cubital tunnel view less relevant ( Fig. 111.5 ).



Symptomatic treatment is appropriate, especially in the early stages, and is discussed in Chapter 76 . In our experience, the mean time to surgery from symptom onset is about 5 years. The most important feature of the initial treatment is to explain to the patient the cause of the pain and the natural history of the process and to recommend activity modification. However, because this disorder is so often associated with one's occupation, this advice usually goes unheeded or cannot be acted on. Avoiding pressure to the cubital tunnel is recommended if there are ulnar nerve symptoms.
The surgical treatment is débridement. In the early stages, arthroscopic intervention is effective to simply remove loose bodies as well as osteophytes. An open ulnohumeral débridement is now reserved for more extensive involvement. In either instance, the ulnar nerve is decompressed when symptomatic ( Table 111.1 ).
| Dominant Symptom | Surgical Technique |
|---|---|
| Loose body | Arthroscopy |
| Motion loss | |
| Mild | Arthroscopy |
| Moderate | Arthroscopy/column |
| Impingement pain | |
| Mild hypertrophic changes | Arthroscopy |
| Moderate changes | Ulnohumeral arthroplasty |
| Ulnar nerve symptoms | Decompress: arthroscopy/UHA |
| Pain at radiohumeral joint | Hemiarthroplasty (capitellar replacement?) |
| Severe pain age >70 years | Total elbow replacement |
Arthroscopic débridement of the elbow is discussed in Chapter 21 . Several factors should be considered if choosing this treatment option:
The surgeon's expertise with elbow arthroscopy.
The surgeon's familiarity with elbow pathology, specifically the pathology of primary osteoarthritis.
The disease should not be too extensive; specifically, the joint should be readily entered and landmarks visualized.
The ulnar nerve should be asymptomatic; if it is not, a simple open decompression prior to the débridement is performed.
The ever-present potential for nerve injury. Both the radial and the ulnar nerve must be discussed with the patient and assiduously avoided during the procedure.
The contraindications for this procedure are prior ulnar nerve translocation and limited experience on the part of the surgeon.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here