Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Gestational trophoblastic disease (GTD) is defined as a spectrum of abnormal gestations and neoplasms arising from villous or extravillous trophoblast that are associated with pregnancy. As discussed in this chapter, GTD may take several forms, each with its own risk of mortality and responsiveness to chemotherapy. The gestational nature of these disorders justifies their discussion in the context of pregnancy evaluation as (1) most cases are directly related to a pregnancy, (2) the evaluation of each pregnancy requires the exclusion of trophoblastic neoplasia, and (3) a high percentage of hydatidiform moles are discovered in the first trimester. The most common types of trophoblastic lesions occur primarily in the first trimester of pregnancy and consist (in descending order of frequency) of partial hydatidiform mole (PHM), complete hydatidiform mole (CHM), placental site trophoblastic tumor (PSTT), and choriocarcinoma. The best studied are the CHMs, which are genetically abnormal gestations carrying a significant risk of subsequently developing gestational trophoblastic neoplasia, including choriocarcinoma. A pathologic diagnosis of a hydatidiform mole should prompt the clinician to serially monitor the patient's serum beta–human chorionic gonadotropin (β-hCG) for regression. The clinical features of these tumors, histopathology, and management are detailed in Tables 30.1 through 30.5 .
| Disorder | Clinico-Radiologic Features | Beta–Human Chorionic Gonadotropin | Endometrial Curettings/Hysterectomy (Gross) | Exclude |
|---|---|---|---|---|
| PHM |
|
Variable |
|
|
| CHM |
|
High (>100K mIU/mL) |
|
|
| Persistent GTD/invasive mole |
|
Plateau (<10% drop in 14 days) or rising (>10% increase × 3 weeks) |
|
|
| Choriocarcinoma |
|
|
Hemorrhagic tumor nodules in endomyometrium |
|
| PSTT |
|
Persistent, low (50 mU/mL) | Discrete or infiltrative, polypoid or endophytic, tan, fleshy mass in endomyometrium |
|
| ETT |
|
Persistent low (<150 mU/mL) |
Expansile mass, may be centered in cervix or lower uterine segment |
|
| Spontaneous pregnancy loss/SAB | Vaginal bleeding, first/second trimester | Declining | Minimal villous edema (not typically grossly evident; by dissecting microscope or histology usually) |
|
a With first trimester ultrasound screening and quantitative β-hCG, complete hydatidiform moles are most often diagnosed before clinical manifestations are evident.
| Disorder | Villi | Trophoblast | Exclusions | Ancillary Studies |
|---|---|---|---|---|
| PHM |
|
|
|
|
| CHM |
|
Diffuse triphasic trophoblast hyperplasia and atypia |
|
|
| Early CHM |
|
|
|
|
| ChorioCa | None present | Dimorphic/biphasic trophoblast atypia |
|
Immunostain: Strongly β-hCG and inhibin positive |
| PSTT | None present |
|
|
|
| ETT | None present |
|
|
|
| Hydropic abortus | Gradual differences in villous size with edema |
|
|
|
| Aneuploid gestation (e.g., trisomy 13) |
|
|
|
|
| Disorder | Therapy | Risk of Progression | Comments/Caveats |
|---|---|---|---|
| PHM |
|
|
Confusion with a twin complete and normal gestation (rare) |
| CHM |
|
|
If persistently elevated β-hCG: 75% have persistent GTD; 25% risk of ChorioCa |
| Persistent invasive mole |
|
“Persistent GTD” is a clinical diagnosis applied to persistently elevated serum β-hCG following molar pregnancy and often treated empirically without pathologic sampling to distinguish persistent/invasive mole versus ChorioCa | |
| Choriocarcinoma |
|
|
|
| PSTT and ETT |
|
|
Poor prognosis: >5 mitoses/10 HPFs (recurrence), pulmonary metastases, antecedent pregnancy >4 years prior |
| Feature | Sensitivity | Specificity |
|---|---|---|
| Absence of embryogenesis | 100 | 79 |
| Myxoid stroma | 92 | 100 |
| Implantation site atypia | 77 | 96 |
| Villous cavitation | 92 | 85 |
| Syncytiotrophoblastic “hyperplasia” and atypia | 54 | 99 |
| Cytotrophoblast hyperplasia and atypia | 77 | 100 |
| Syncytiotrophoblast “hyperplasia” and cavitation | 92 | 95 |
| Syncytiotrophoblast and cytotrophoblast hyperplasia and cavitation | 85 | 100 |
| Partial Mole | Complete Mole | |||
|---|---|---|---|---|
| Sensitivity | Specificity | Histologic Features | Sensitivity | Specificity |
| 79 | 77 | Inclusion | 18 | 51 |
| 100 | 22 | Syncytiotrophoblast hyperplasia | 80 | 17 |
| 100 | 35 | Contour complexity | 60 | 17 |
| 43 | 81 | Enlargement | 4 | 54 |
| 57 | 79 | Cavitation | 8 | 51 |
| 29 | 100 | Inclusion + syncytiotrophoblast hyperplasia | 0 | 86 |
| 79 | 83 | Inclusion + complexity + enlargement | 16 | 50 |
| 29 | 100 | Cavitation + inclusion + enlargement + syncytiotrophoblast hyperplasia | 0 | 93 |
Risk factors for GTD include a range of epidemiologic and genetic parameters ( Table 30.6 ) and are most strongly associated with subtypes of GTD at greatest risk for either persisting or evolving into malignancy. The principal risk factors are advanced maternal age, Asian ethnicity, lower socioeconomic status (in selected populations), and one or more prior molar pregnancies. Two types of molar gestations have been recognized, and their incidence varies widely worldwide: CHM (prevalence approximately 1 per 1000 pregnancies) and PHM (prevalence approximately 1 per 100 pregnancies).
| Factor | Qualifier | Relative Risk |
|---|---|---|
| Maternal age | <20 years | 1.5 |
| >40 | 5.2 | |
| Prior SAB | 1.9–3.3 | |
| Parity | >1 | 0.4 |
| Vitamin A | Median consumption | 0.6 |
| Incidence | ||
| Race | Indonesia | 1 : 85 |
| Japan | 1 : 522 | |
| Sweden | 1 : 1560 | |
| United States | 1 : 1724 | |
| Socioeconomic status | Philippines (wealthy) | 1 : 2000 |
| Philippines (poor) | 1 : 200 | |
| Prior molar pregnancy | 1 | 1 : 100 |
| >1 | 1 : 6 to 1 : 4 | |
| Trend | ||
| Smoking | >15 cigarettes/day | Increasing |
| Infertility | Increasing | |
| Theca-lutein cyst | >6 cm by ultrasound | Increasing (GTD subsequently develops in up to 50%) |
Molar gestations occur in women of all reproductive ages, but the highest incidence (per pregnancy) occurs in women over 40 years old, where the relative risk increases to more than 5. Women younger than 20 years old have a slightly increased risk as well (relative risk = 1.5).
Another major risk factor for molar pregnancy is maternal Asian race. In Indonesia, the rate is more than 1 molar gestation in 100 pregnancies. The socioeconomic status of women within this population is also an important factor in some studies; poor individuals show a tenfold greater risk of GTD than wealthy individuals from the same Asian population.
Nulliparity is associated with a slightly less than twofold increased risk of GTD. In one study, two or more spontaneous abortions conferred a 32-fold increase in risk of GTD.
Approximately 1% of pregnancies following a single hydatidiform mole will be a recurrent hydatidiform mole. If the patient has had two prior molar pregnancies, the risk is increased to 16% to 28%.
Complete and partial moles have different genetic, clinical, and pathologic features ( Fig. 30.1 ). A CHM develops when an empty (i.e., without female pronucleus) oocyte is fertilized by one or two spermatozoa, resulting in a diploid genome with two complete male-derived haploid chromosomal sets (diandry). In 90% of complete moles, a single 23,X spermatozoa duplicates its chromosome after fertilization, resulting in a 46,XX complete mole; in the remaining 10% of complete moles, two spermatozoa fertilize an empty egg, resulting in 46,XX or 46,XY molar karyotypes. PHMs result from two potential scenarios. In approximately three quarters of the partial mole cases, a normal egg is fertilized by two spermatozoa, resulting in diandric, monogynic triploidy (70% 69,XXY; 27% 69,XXX; 3% 69,XYY).
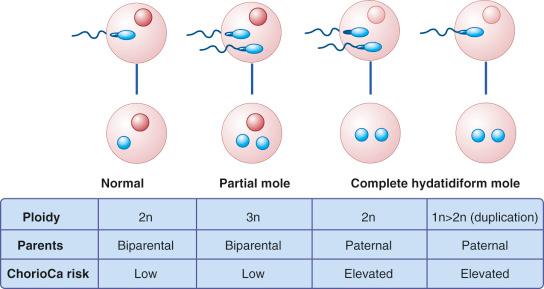
In the second scenario, nondisjunction in meiosis I or meiosis II of spermatogenesis results in an extra set of paternal chromosomes in one sperm (diandric), which fertilizes a haploid (monogynic) egg. It is important to realize that not all triploid gestations are partial moles; cases that have two haploid sets of maternal chromosomes resulting from nondisjunction in meiosis I or meiosis II of oogenesis and one haploid set of paternal chromosomes (monoandric and digynic) are abnormal but nonmolar (accounting for approximately 10% of all triploid gestations) (discussed later).
As will be discussed further in this chapter and as detailed in Table 30.7 , the diagnosis, classification, and differential diagnosis of GTD have undergone a major renaissance since the 1980s because of the genetic information obtained from these abnormal conceptuses combined with new biomarkers used for their diagnosis.
| Decade | Molar Categories | Parameters | Differential Diagnosis |
|---|---|---|---|
| 1970s | Hydatidiform mole grade 1-6 | Morphology | Hydropic abortus |
| 1980s | Partial and complete mole | Genetics | Hydropic abortus |
| 1990s | Partial and complete mole |
|
|
| 2000s | Partial and complete mole | p57 expression | Complete mole versus other biology genetics |
Trophoblast differentiation has been described in detail earlier (see Chapter 29 ). Both villous and extravillous trophoblasts are subject to neoplastic transformation; specifically, it is thought that the proliferative phenotypes (villous cytotrophoblast, early implantation/cell column, and transitional extravillous trophoblast) are the cells of origin of trophoblast neoplasia ( Fig. 30.2 ). The non-proliferative, mature trophoblasts (the villous syncytiotrophoblast and mature extravillous trophoblast) are perceived as terminally differentiated and presumably not susceptible to neoplastic transformation, although their phenotypes are seen in the maturation of the other trophoblast neoplasia. It should be pointed out, however, that ultimately, all of these phenotypes are derived from the villous cytotrophoblast, the presumed trophoblastic stem/progenitor cell.
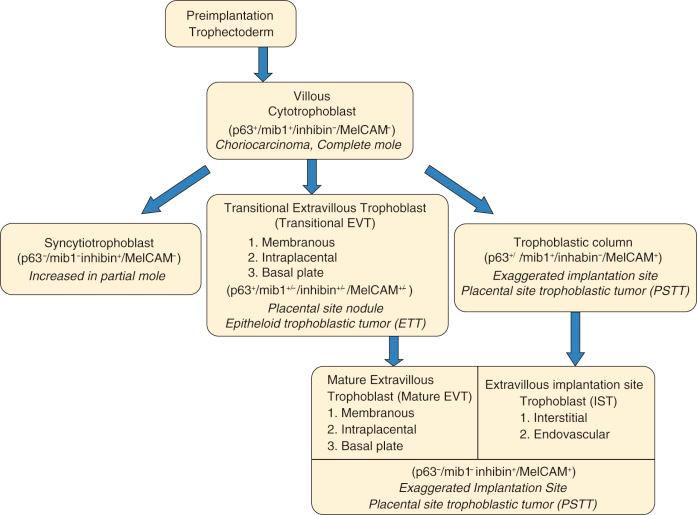
The villous cytotrophoblast is considered the cell of origin for both CHM and choriocarcinoma. The diagnosis of both is predicated on the identification of both cytotrophoblastic proliferation and atypia. Cytotrophoblasts are considered trophoblast stem/progenitor cells, staining strongly for both p63 and proliferative markers, as well as cytokeratins, but essentially nonreactive for hCG, inhibin, and human placental lactogen (hPL) (see Chapter 29 ).
Syncytiotrophoblast , typically multinucleated, form abruptly in the chorionic villi from cytotrophoblasts and exhibit considerable cytoplasmic differentiation and stain intensely for human chorionic gonadotropin (hCG) and inhibin, albeit only in the first trimester (see Chapter 29 ). The syncytiotrophoblast cytoplasm can become vacuolated; these vacuoles can coalesce to form “lacunae,” in which case the cell assumes an irregular, lacy appearance. Such appearance of the syncytiotrophoblast can be seen in both complete and partial moles. In the complete mole, this component is distinctly immature, producing a lushly festooned arrangement of concentric syncytiotrophoblast that appears to cascade from the involved villi. In contrast, in the partial mole, the syncytiotrophoblastic “atypia” is more subdued, limited to smaller aggregates but still concentrically arranged in some villi. The term syncytiotrophoblastic hyperplasia is often applied to the villi in this context; however, the appearance is more likely the result of an abnormal trophoblastic maturation process rather than a proliferation of these cells.
The extravillous trophoblast is considered the cell of origin for both PSTT and epithelioid trophoblastic tumor (ETT) lesions, which are significantly less common than tumors of the villous trophoblast. Extravillous trophoblasts are derived from cytotrophoblast in two scenarios.
In early gestation, extravillous trophoblasts evolve beneath the cytotrophoblastic columns of anchoring early in gestation and invade the decidua and superficial myometrium. These cells are strongly immunoreactive for inhibin and MelCAM (also known as MCAM, MUC18, and CD146), as are the cells in their malignant counterpart, the PSTT. In their benign form, they are encountered in the endomyometrial implantation site early in pregnancy in association with Nitabuch fibrin.
Later in gestation, extravillous trophoblast emerge from the villi as they encounter extracellular matrix, whether it is fibrinoid following degeneration of chorionic villi in fetal membranes, at the basal plate, or in perivillous fibrin, such as in the intraplacental trophoblast islands throughout the placental disc (see Chapter 29 ). These cells have a variable phenotype, depending on where they are in transition from cytotrophoblast. The least mature, or “transitional” (epithelioid) extravillous trophoblasts have a more vacuolated cytoplasm, retain p63 and cyclin E expression, and their transformed counterpart defines the ETT. The more mature extravillous trophoblasts have a more eosinophilic cytoplasm and have fully lost their expression of p63. These cells are quite similar in immunophenotype to those seen in early implantation site or PSTTs, being inhibin and MelCAM positive. Unlike the PSTT, where immunophenotypically similar extravillous trophoblast are capable of rarely undergoing neoplastic transformation, in mature placenta and in ETTs these more mature extravillous trophoblast are a product of maturing transitional (epithelioid) trophoblast. Predictably, the mature extravillous trophoblast will be more conspicuous in normal gestational tissues or in residual placental site nodules following pregnancy and less likely to be encountered in ETTs where the tumor is composed primarily of non-maturing malignant transitional (epithelioid) trophoblast. This explains the low percentage of cells staining for MelCAM in ETTs. Both PSTT and ETT are strongly immunoreactive for cytokeratins, hPL, and GATA3, and weakly reactive for hCG, with ETTs being more variable in this regard. The most distinctive marker of ETT is p63 (see later), again because the transitional (epithelioid) trophoblast retains p63 expression.
These pathways of trophoblastic differentiation and their neoplastic counterparts are integrated schematically in Fig. 30.2 . One important point to address here is the difference in terminology, used in reference to extravillous trophoblast lineage in particular. In much of the literature, these cells have been referred to as “intermediate” trophoblast, mostly because, morphologically, they have a phenotype “intermediate” between cyto- and syncytiotrophoblast. However, because we have come to recognize that these cells represent the product of differentiation pathways distinct from that which takes place in chorionic villi (differentiation of cytotrophoblast into syncytiotrophoblast), we strongly believe that the more appropriate, and perhaps intuitive, term for these “nonvillous” trophoblast is “extravillous” trophoblast. In addition, elsewhere in the literature, the extravillous trophoblast has often been distinguished based on location in the placenta, and the origin of ETT is often attributed to “chorionic” trophoblast, the extravillous trophoblast in fetal membranes. Although the extravillous trophoblasts in the fetal membranes are indeed often vacuolated and correspond to the chorionic or epithelioid type, we interpret them as a differentiation pattern that is more generic, signifying a “transition” from cytotrophoblast to mature extravillous trophoblast that can be encountered in intraplacental fibrin and maternal surface, as well as the extraplacental membranes (see Chapter 29 ). Therefore, in attributing the origin of ETT to such “transitional” extravillous trophoblast, we expect that the origin could be either membranes or maternal surface of the placenta, the latter a very logical source for many retained implantation site nodules often encountered after pregnancy—and a presumed source of occasional ETTs—in the corpus (see Fig. 30.2 ).
Recent studies imply these trophoblast subtypes can be distinguished in part by their expression of one particular transcription factor, p63. p63 is related to both p53 and p73 and encodes two different isoforms, a full-length form resembling p53 (TAp63) and a truncated isoform (ΔNp63) that is commonly expressed in squamous epithelium. Trophoblastic columns, adjacent to villous structures in the early placenta, and villous cytotrophoblast strongly express ΔNp63. Cells in transition from the cytotrophoblast to mature extravillous trophoblast (“transitional” or epithelioid extravillous trophoblast) also express ΔNp63 (see Chapter 29 ), but syncytiotrophoblasts and the more mature extravillous trophoblasts are p63 negative. TAp63, on the other hand, is known to be expressed in extravillous trophoblast in the fetal membranes, but its expression in similar cells in intraplacental islands and the basal plate is less clear. The expression pattern of p63 suggests that, like in other epithelia, it is governed by both maturation and proximity of the trophoblast to supporting mesenchyme.
Despite biological differences between various cell types of the trophoblastic spectrum, all trophoblast phenotypes share common expression of some proteins. Definition of such overlapping gene expression patterns may be exploited in routine diagnostic practice in general and in particular for classifying tumors of the female reproductive tract having prominent atypia. Previously, the most useful markers common to all trophoblastic cell lineages were keratins, but its low sensitivity (as it also is expressed by carcinomas relevant to the typical differential diagnosis) hinders its usefulness. More recently, the enhancer-binding protein GATA3 has been found to be expressed in the majority (80% or better) of all trophoblast proliferations, both benign and malignant. Thus, detection of nuclear GATA3 expression in a difficult-to-classify tumor may be very helpful in recognizing its trophoblastic origin and excluding competing diagnoses of various high-grade müllerian carcinomas and pelvic tumors of unknown origin. Of course, one must be mindful that carcinomas arising from outside the müllerian system (i.e., urothelial and breast) also express GATA3. GATA3 expression also may decline in the chorionic villi of term placentas, but this does not pose any problems for diagnostic use. Thus, inclusion of GATA3 in tumor immunophenotyping panels may be helpful when evaluating difficult tumors in the proper clinical and pathologic context.
The modified International Federation of Gynecology and Obstetrics (FIGO) staging system for GTD is based on anatomic location ( Table 30.8 ), whereas the World Health Organization (WHO) score is based on a variety of prognostic factors ( Table 30.9 ). A combination of these two systems is applied to separate patients into “low-risk” (FIGO stage I to III with a WHO score of 6 or less) and “high-risk” (FIGO stage I to III with a WHO score of 7 or more, or FIGO stage IV) categories. Generally speaking, management of the low-risk patient is with single agent chemotherapy (methotrexate), whereas high-risk patients are treated with combination chemotherapy.
| Stage I | Gestational trophoblastic tumors confined to uterine corpus |
| Stage II | Gestational trophoblastic tumors extending to the adnexae or vagina, but limited to the genital structures |
| Stage III | Gestational trophoblastic tumors extending to lungs, with or without genital tract involvement |
| Stage IV | Metastatic involvement of all other extrapulmonary sites (brain, liver, kidney, spleen, gastrointestinal tract) |
| FIGO Score | 0 | 1 | 2 | 4 |
|---|---|---|---|---|
| Age | <39 | >39 | — | — |
| Antecedent pregnancy | Mole | Abortion | Term | — |
| Interval from index pregnancy, months | <4 | 4-6 | 7-12 | >12 |
| Pretreatment hCG mIU/mL | <10 3 | >10 3 -10 4 | >10 4 -10 5 | >10 5 |
| Largest tumor size including uterus, cm | 3-4 | >5 | — | — |
| Site of metastases including uterus | Lung | Spleen, kidney | Gastrointestinal tract | Brain, liver |
| Number of metastases identified | — | 1-4 | 5-8 | >8 |
| Previous failed chemotherapy | — | — | Single drug | ≥2 drugs |
a After adding points assigned for each parameter, a low-risk score is defined as ≤6, whereas a high-risk score is ≥7.
CHM takes its name from its juxtaposition with PHM, the latter manifesting as sporadic and variable villous enlargement. In contrast the CHM is uniformly abnormal although, as will be detailed later, the abnormality is less conspicuous earlier than later (classic CHM) in gestation.
In the past, most CHMs were clinically recognized in the early second trimester because of heavy vaginal bleeding, anemia, marked uterine enlargement, a highly elevated β-hCG level, and a characteristic ultrasound in which the swollen villi give the appearance of Swiss cheese ( Fig. 30.3A ). Such “late” complete moles were evacuated at a mean gestational age of 14 weeks. Most complete moles are currently evacuated between 8 and 12 weeks of gestational age (“early” complete moles), because widespread use of ultrasonography now permits early recognition and evacuation of most abnormal gestations. However, early complete moles may not be clinically suspected, because frequently there has been minimal bleeding, uterine enlargement, and β-hCG elevation, and because the ultrasonographic features may be subtle. For this reason, the pathologist is often the first to suspect the diagnosis in many current “early” CHMs.
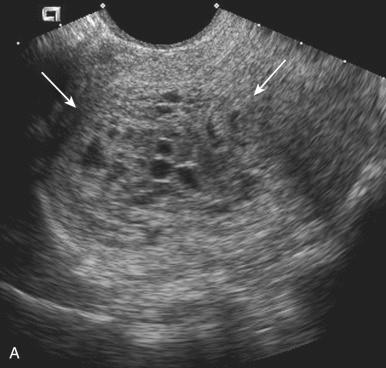
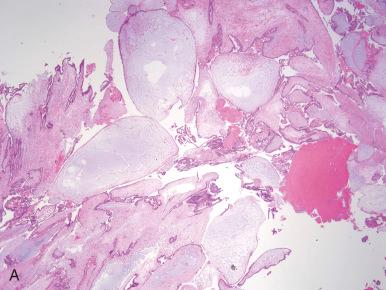
Macroscopically, the complete mole is distinguished by diffuse villous swelling, produced by the influx of fluid into the villi and the absence of any villous vasculature. The fluid distends the villi, producing the appearance of grapes (hence the term hydatidiform ). These transparent, swollen chorionic villi (vesicles) measure up to 2 cm in diameter and are distinguished from those in partial moles by their uniformity throughout the specimen (see Fig. 30.3B ). As will be discussed, the size of these villi and the ease with which the pathologist recognizes a complete mole is determined by the gestational age, with older moles being most conspicuous.
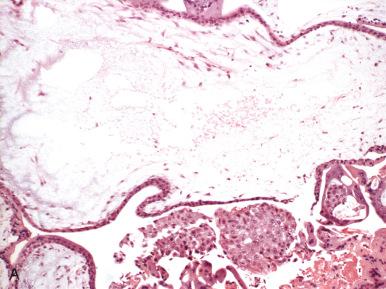
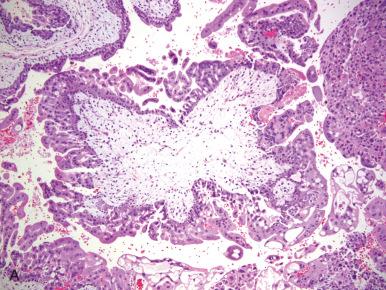
The pathologist can immediately appreciate a well-evolved complete mole on histologic examination. At low power, enlarged hydropic, frequently cavitated villi occupy a large geographic area. The conspicuous cavitations within villi are due to necrosis, forming spaces or cisterns. The other conspicuous finding is the presence of sheets of trophoblast both encircling the villi and bridging one or more villous structures. This villous trophoblastic proliferation is most notable for its concentric distribution on some villi and the participation of both the cytotrophoblast and the syncytiotrophoblast. Often, the syncytiotrophoblast may appear immature and form Medusa-like festoons emanating from the molar villi. The degree of cytologic atypia of the cytotrophoblast and syncytiotrophoblast exceeds that of nonmolar pregnancy but is not always conspicuous ( Fig. 30.4A-C ). Non-villous gestational tissues, including chorionic membrane, amnion, yolk sac, and nucleated fetal red blood cells (RBCs), are typically absent. Cases of complete mole with small numbers of nucleated RBCs are quite rare but well documented in our case files. All complete moles (early and late) typically show significant atypia of trophoblastic cells within the decidual implantation site (see Fig. 30.4D ). This latter feature is useful for confirming the diagnosis histologically, particularly in small samples or when the differential diagnosis includes partial mole or hydropic abortus.
The higher surveillance of early gestations has permitted clinicians and pathologists to recognize complete moles earlier in their natural history. These abnormal gestations can be appreciated on ultrasound, by careful gross inspection of the placental villi and attention to subtle but defined histologic parameters that herald the presence of early complete mole. Most early complete moles grossly resemble spontaneous abortion specimens; macroscopic villous edema is usually minimal but may be appreciated by the trained eye, particularly under the dissecting microscope. However, because many practices do not perform an exhaustive prehistologic examination of products of conception, most early complete moles are discovered by careful attention to several parameters:
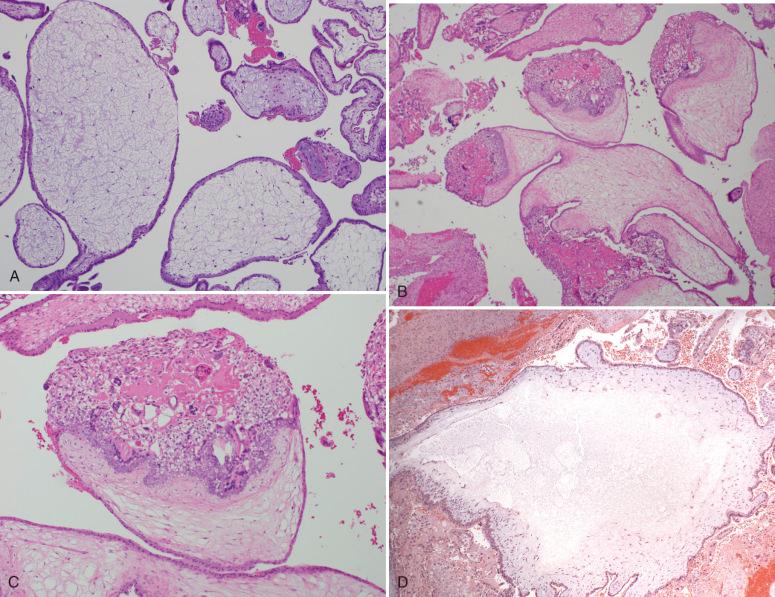
Histologically, these specimens typically display scattered cavitated villi (with slight enlargement) and focal to diffuse hyperplasia and atypia of the trophoblast ( Fig. 30.5A ).
Villous stromal features are highly characteristic, including a hypercellular population of tiny stellate mesenchymal cells in a blue myxoid matrix (resembling a fibroadenoma) (see Fig. 30.5B ).
Prominent karyorrhexis is seen in the villous mesenchymal cells (see Fig. 30.5B ).
Typical villous morphology includes many cauliflower-like villi, with toe- or knuckle-like bulbous protrusions separated by linear slits (see Fig. 30.5C ).
An important feature confirming the disease is marked implantation site atypia (see Fig. 30.5D ), reported in 66% in one study.
Because the pathologic features of an early complete mole may be subtle, pathologic recognition can be challenging, particularly with limited sampling. Adequate tissue sampling (a minimum of four to five paraffin blocks) is warranted whenever a molar gestation is clinically suspected or when the initial histologic evaluation raises the suspicion of a hydatidiform mole. One potential diagnostic pitfall when interpreting an early complete mole is the presence of degenerative changes with prominent villous edema and inconspicuous trophoblastic hyperplasia/atypia. Such cases require careful scrutiny of the trophoblast and cautious use of immunohistochemistry (see the next section) ( Fig. 30.6 ).
The differential diagnosis of a complete mole includes (1) early gestations with accentuated villous edema ( Fig. 30.7A ), (2) exuberant trophoblast cell column associated with early/aneuploid gestation (see Fig. 30.7B and C ), (3) partial mole (see later), and (4) an intact gestational sac mimicking a single cavitated villus (see Fig. 30.7D ). A rarely encountered androgenetic/biparental mosaic/chimeric conception can also generate some diagnostic confusion.
Early/hydropic abortus should be considered when the pathologist assesses a possible hydatidiform mole. The histopathology of a hydropic abortus is characterized by degenerated-appearing, edematous villi with balloon-like, rounded contours and an attenuated trophoblastic lining (see Fig. 30.7A ). Complete molar specimens typically display characteristic villous morphology (either diffuse hydrops in late complete moles or primitive stromal features in early complete moles; compare Fig. 30.4 with Fig. 30.5 ) and significant trophoblastic hyperplasia and atypia (involving cytotrophoblasts, syncytiotrophoblasts, and extravillous trophoblasts). In specimens that are difficult to pathologically classify, adequate sampling (at least five blocks of tissue), supplemented by p57 immunohistochemistry (discussed later), will disclose the correct diagnosis in most cases.
Occasionally, early products of conception, from either euploid or aneuploid gestations, show an exuberant trophoblast cell column, which can imitate the villous trophoblast hyperplasia associated with a complete mole (see Fig. 30.7B ). On closer inspection, however, these are quickly recognized as “eccentric” trophoblast hyperplasia, rather than the concentric hyperplasia characteristic of a complete mole (see Fig. 30.7C ). If needed, p57 immunostaining (see later) can also help confirm the diagnosis.
This should always be suspected in the presence of a single large villus-like structure (see Fig. 30.7D ). Gestational sacs can also show mild trophoblast proliferation and atypia, and have a p57 immunostaining pattern, which may be mistaken for a complete mole (see later). Nevertheless, the lack of additional villous tissue and careful evaluation of the p57 expression pattern should facilitate a correct interpretation. The gestational sac, being singular, also is more likely to be misclassified as a PHM (see later).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here