Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Operative treatment of scaphoid nonunion varies based on the timing of the injury, bone loss at the fracture site, location of the fracture, presence of humpback deformity or an increased intrascaphoid angle, and the vascularity of the proximal pole.
Humpback deformity results from collapse of the distal pole of the scaphoid. Normal intrascaphoid angle is 30 degrees plus or minus 5 degrees. Humpback deformity is present when the intrascaphoid angle measured on lateral x-ray or computed tomography (CT) scan is greater than 35 degrees ( Fig. 26.1 ).
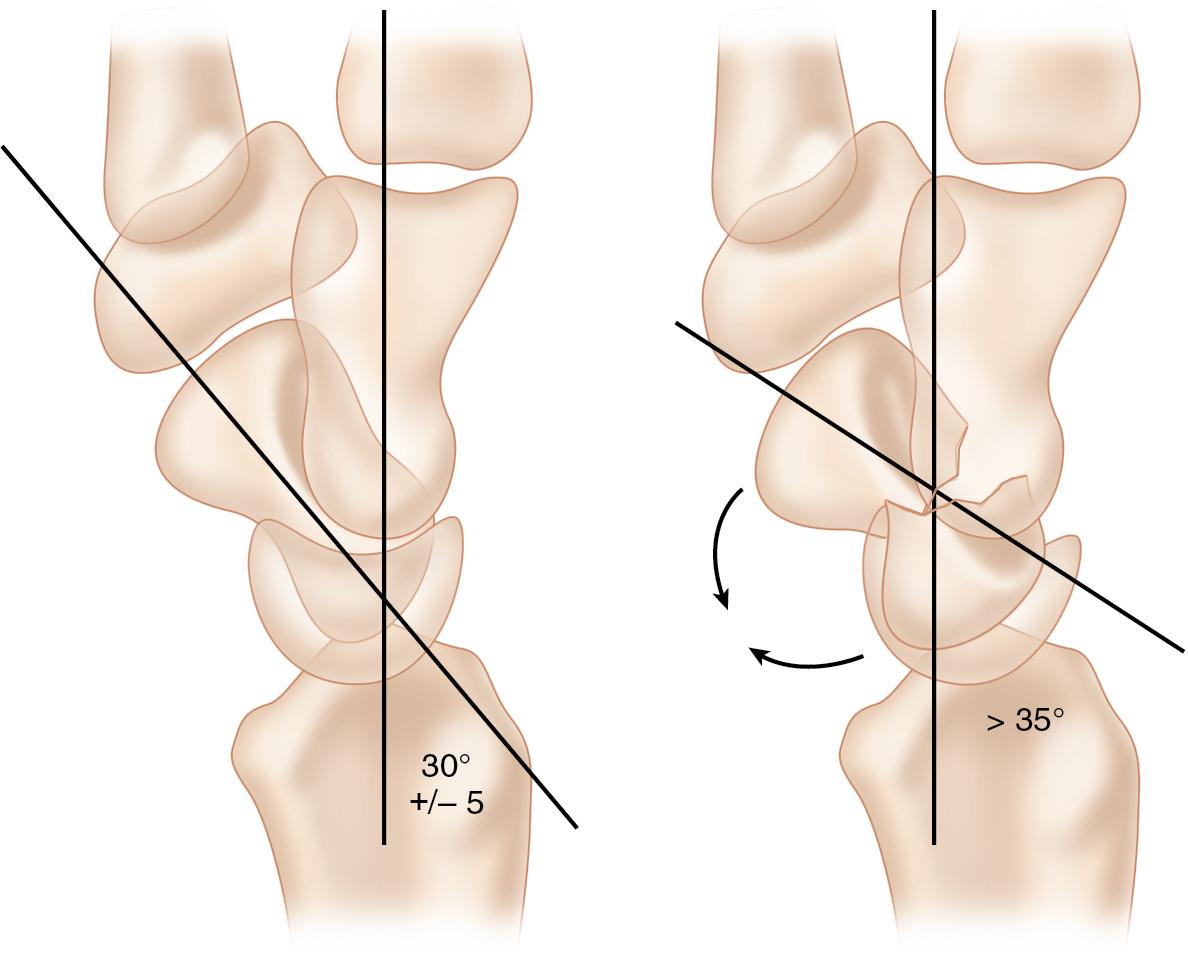
Table 26.1 highlights our treatment algorithm for scaphoid nonunion based on specific fracture characteristics.
| Type of Fracture | Treatment |
|---|---|
| Delayed union (< 6 months) | Open reduction and internal fixation with headless compression screw |
| Established nonunion without humpback deformity | Open reduction and internal fixation with headless compression screw + bone graft (distal radius, iliac crest cancellous bone graft) |
| Nonunion with humpback deformity but no evidence of avascular necrosis | Open reduction via volar approach, corticocancellous bone graft |
| Avascular nonunion without humpback deformity | Vascularized bone graft, dorsal or volar approach |
| Avascular nonunion with humpback deformity | Vascularized medial femoral condyle bone graft via volar approach |
Signs of radiocarpal or intercarpal arthritis, especially patterns indicative of scaphoid nonunion advanced collapse (SNAC; Fig. 26.2 and Table 26.2 ), often confirm that repair/reconstruction are no longer options and salvage should be considered.
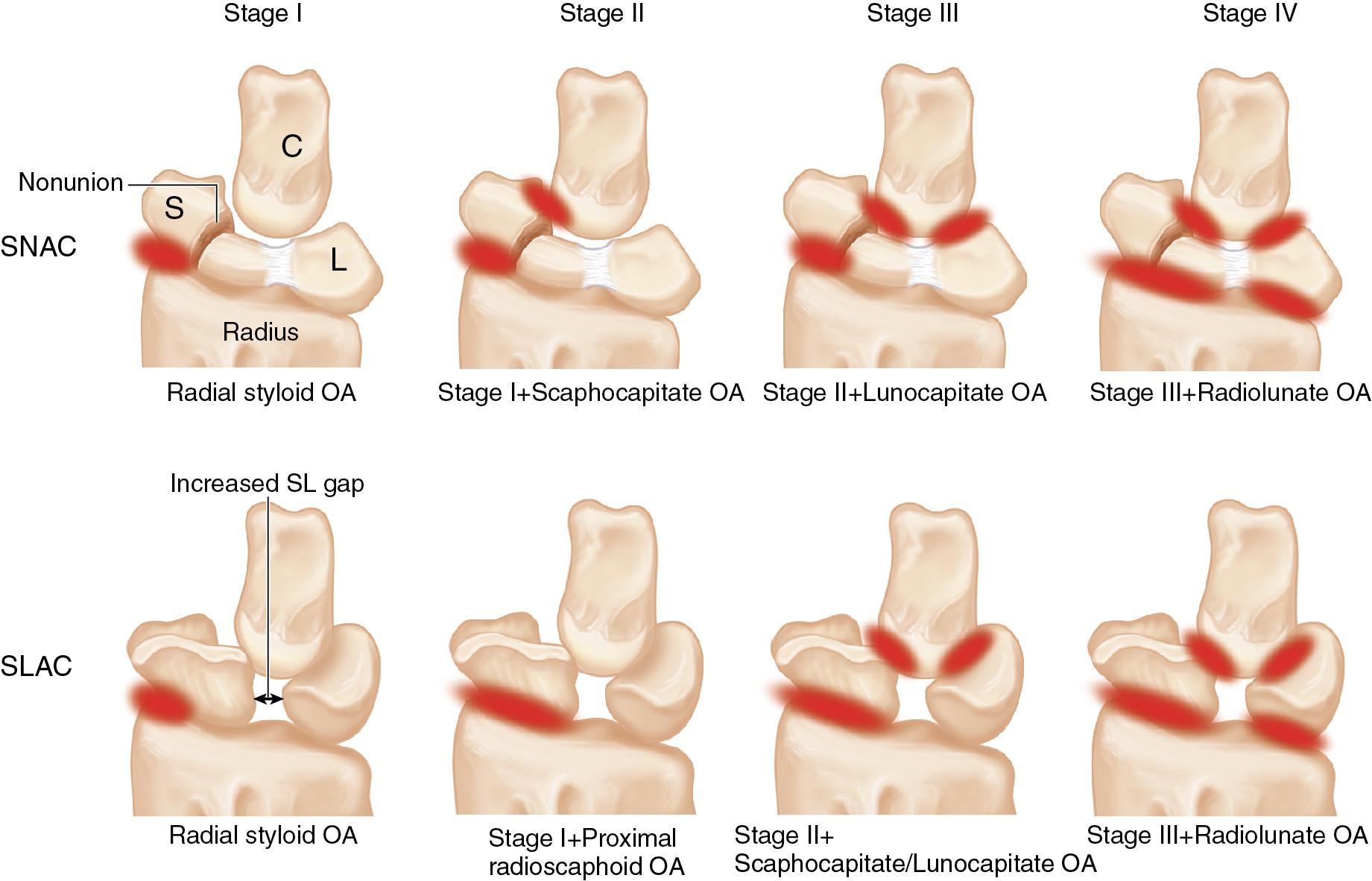
| Stage | Sites of Osteoarthritis |
|---|---|
| 1 | Radial styloid |
| 2 | Stage 1 & Scaphocapitate |
| 3 | Stage 2 & Lunocapitate |
| 4 | Stage 3 & Radiolunate |
The distal pole of the scaphoid may be tender to palpation, and axial compression of the thumb may reproduce the pain.
Nagging wrist pain or tenderness in the snuff box months after an injury may indicate a scaphoid fracture that has progressed to a nonunion.
Decreased wrist motion and grip strength are common findings in patients with a scaphoid nonunion.
If a patient continues to have radial-sided wrist pain with tenderness over the scaphoid in the anatomic snuff box despite prior treatment, this may reveal progression to nonunion.
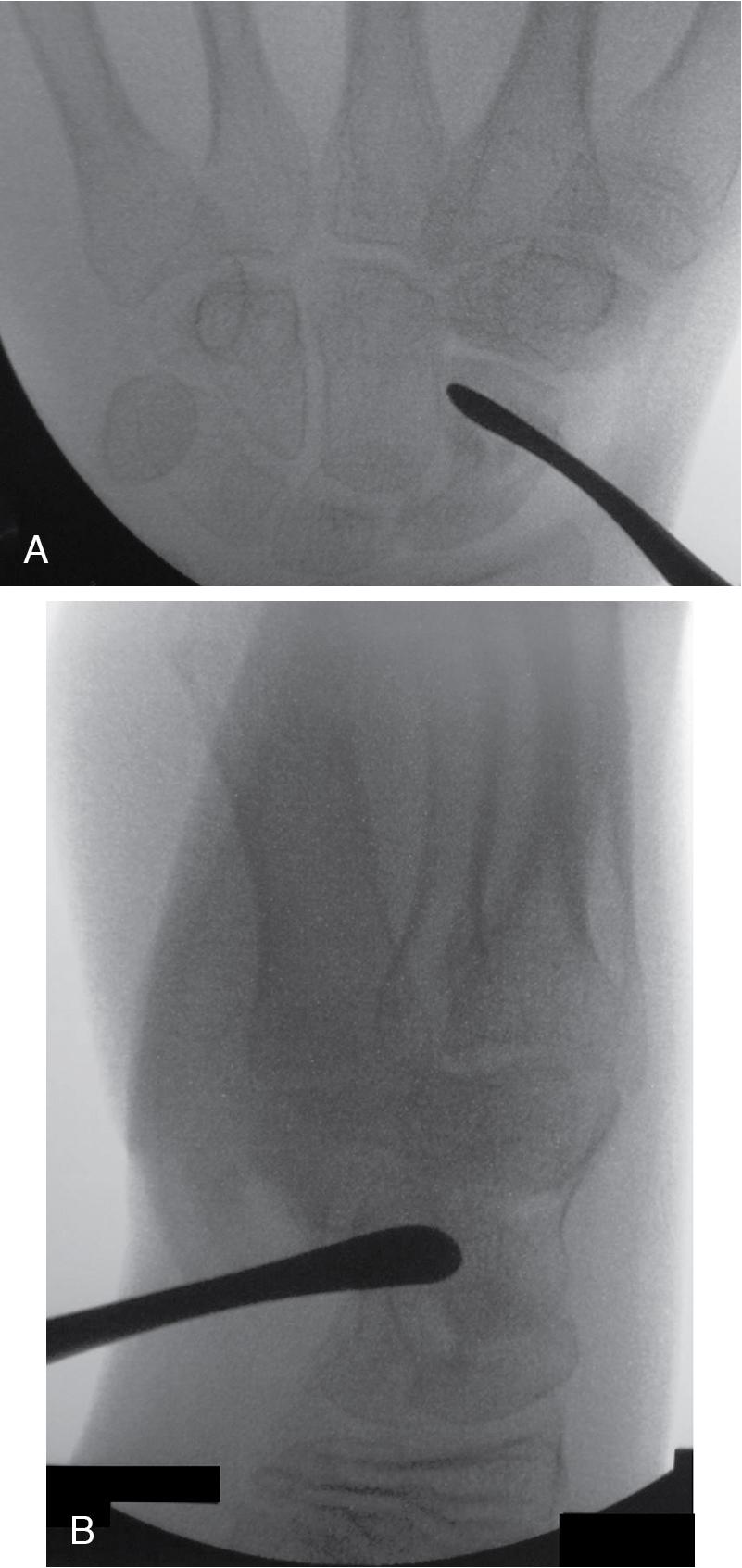
A standard three-view wrist x-ray should be obtained. If present, the nonunion is often apparent ( Fig. 26.3 ).

Bone loss, cyst formation, and degree of displacement should be noted.
Use the lateral view to approximate the lateral intrascaphoid angle to assess for collapse ( Fig. 26.4 ; see also Fig. 26.1 ).
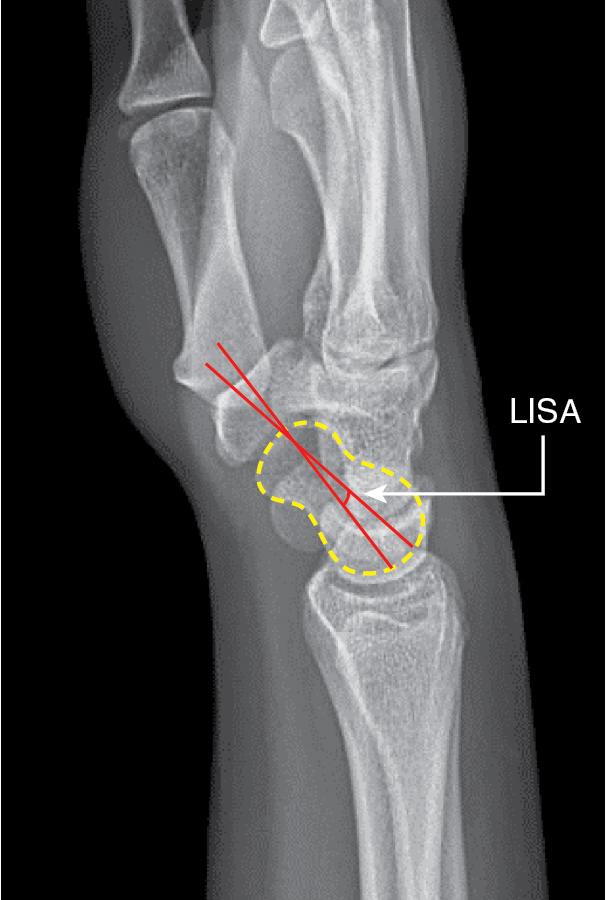
Evaluate for signs of SNAC wrist (posteroanterior [PA] view) and abnormal scapholunate angle (lateral view; see Table 26.2 ).
X-rays may show previously placed hardware.
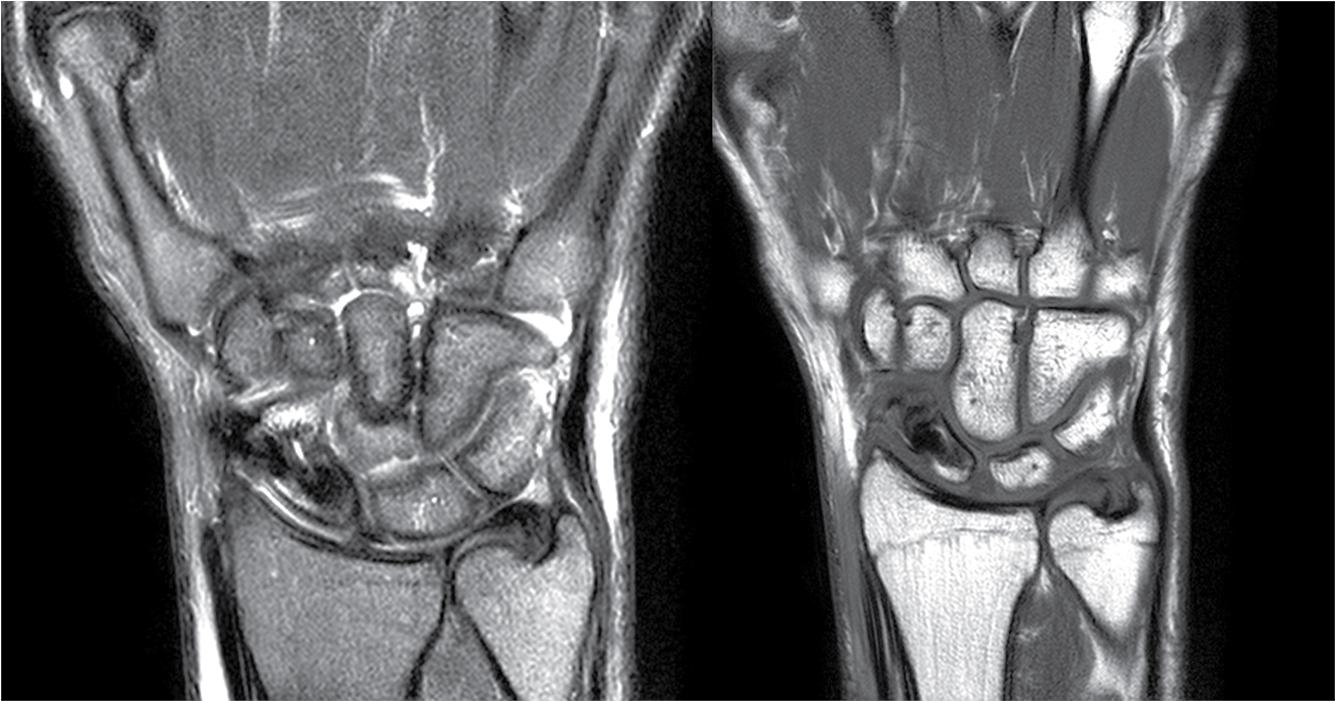
CT and magnetic resonance imaging (MRI) can be useful adjuncts to clinical examination and standard x-ray. Humpback deformity, joint incongruity, and structure of the proximal pole are best appreciated on CT scan. MRI may be used to assess the vascularity of the proximal pole, although there remains no diagnostic gold standard for avascular necrosis ( Fig. 26.5 ).
Indications for ulna bone grafting:
Established nonunion with or without humpback deformity
No evidence of avascular necrosis of the proximal scaphoid pole
Minimal cystic change, displacement, or carpal malalignment
Active smoking is a notable risk factor. We do not operate on patients who are current smokers because of the high risk for nonunion. Urine cotinine testing is obtained to clear a patient for surgery.
Both the ulna donor site and scaphoid recipient site are prepped and draped into the same operative field.
The decision to use a volar or dorsal approach to the scaphoid is guided by the location of the nonunion, the presence of humpback deformity, and the planned procedure.
A proximal nonunion is treated via a dorsal approach for better exposure and for the trailing screw head to purchase the proximal pole.
The volar approach improves visualization of more distal fracture/nonunion locations.
A notable humpback deformity is generally corrected via a volar approach.
Recipient site:
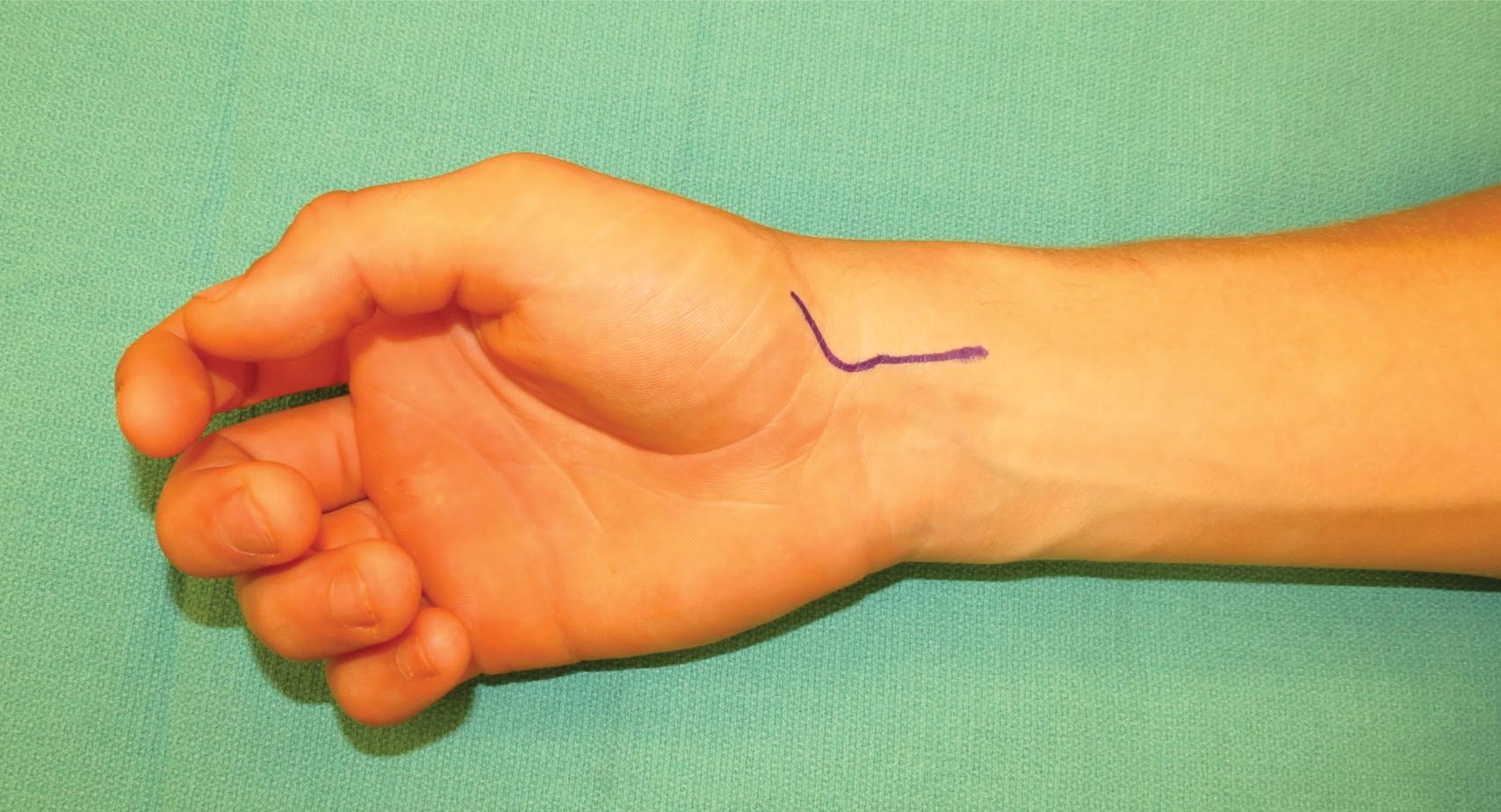
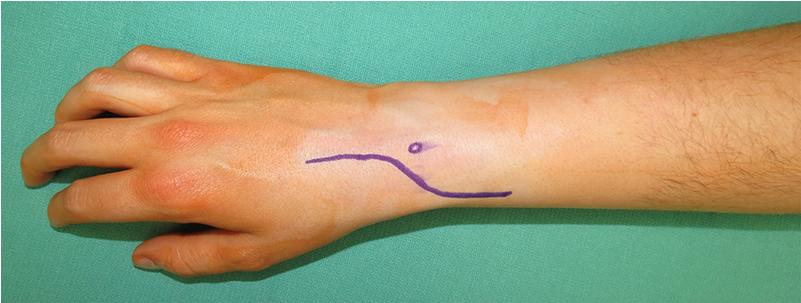
For the volar approach, the scaphoid is exposed via a curvilinear wrist incision. This incision extends from the radial aspect of the thenar eminence, across the wrist, parallel and radial to the flexor carpi radialis (FCR) tendon ( Fig. 26.6 ).
For a dorsal approach, a longitudinal or curved incision over the interval between the third and fourth extensor compartments (use Lister tubercle as a landmark) is used. Branches of the superficial radial nerve and the extensor pollicis longus tendon must be protected during this approach.
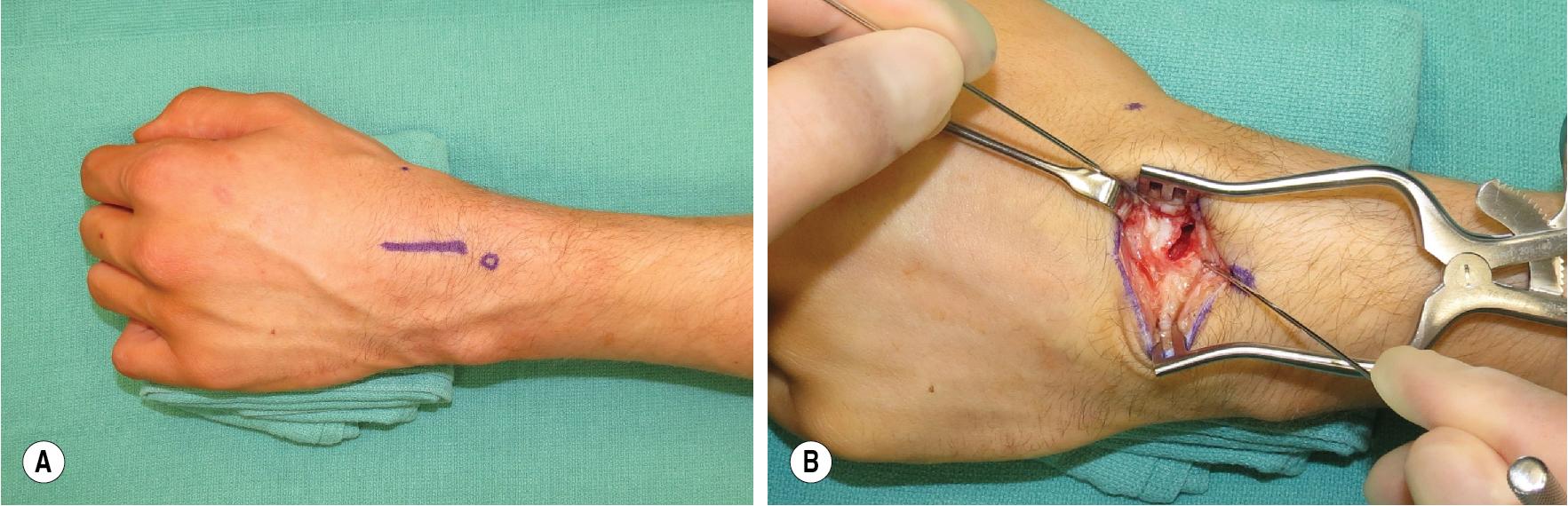
If using a corticocancellous graft, this incision can be somewhat limited ( Fig. 26.7A–B ).
If planning for vascularized bone options (see the section on “Pedicled Vascularized Bone Graft From Dorsal Distal Radius [1,2 Intercompartmental Supraretinacular Artery]”), a wider approach is used.
Donor site: A 5-cm longitudinal incision over the ulna, starting 1 cm distal to the olecranon, is used to expose the flat portion of the proximal ulna in preparation for bone graft harvest. The advantage of the proximal bone graft is that the exposure is relatively avascular and the bone is easily accessible.
Other graft sites (i.e., iliac crest) can also be used, but we prefer the ulna to keep the procedure to one surgical limb.
The dominant blood supply to the scaphoid is via a branch from the radial artery that enters through the dorsal ridge and supplies 70% to 80% of the intraosseous vascularity to the proximal pole. This vessel and its branches enter distally and dorsally and travel retrograde through the scaphoid ( Fig. 26.8 ).
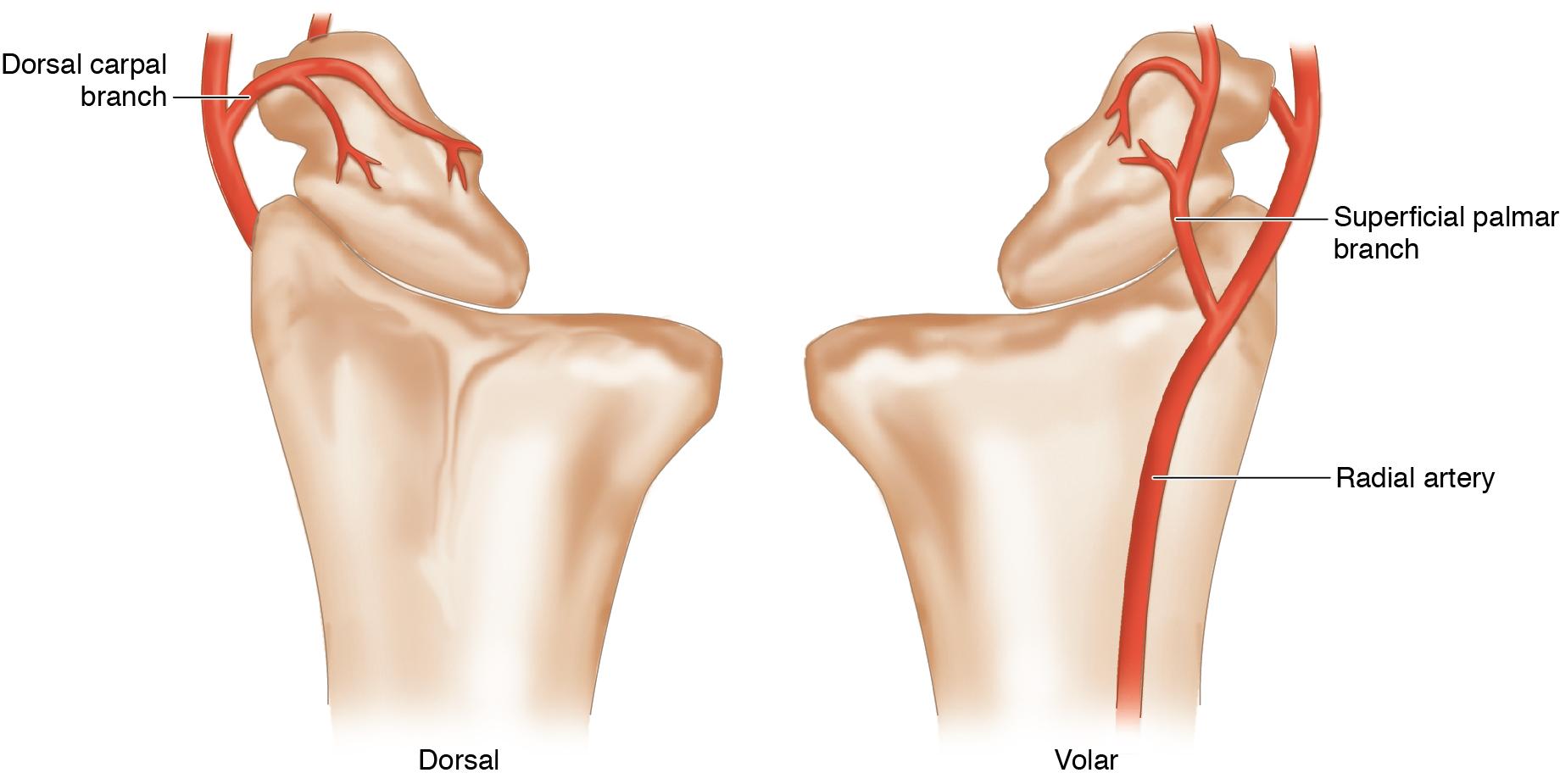
The scaphoid proximal pole is uniquely susceptible to avascular necrosis after fracture because of the high dependence on a dominant retrograde-traveling intraosseous vessel.
A volar branch of the radial artery supplies 20% to 30% of the scaphoid in the region of the distal tuberosity.
Corticocancellous bone is harvested from the ulna, just proximal to the tip of the olecranon. A 5-mm-wide by 10-mm-long by 5-mm-deep bone graft is usually all that is needed for the scaphoid, but up to 20 mm by 30 mm by 10 mm can be harvested as long as both cortices of the ulna are not violated.
The volar wrist incision is carried out through the skin and subcutaneous tissue. The FCR is identified and protected.
The FCR sheath is opened longitudinally and the FCR is retracted ulnarly.
The radioscaphocapitate (RSC) and long radiolunate (LRL) ligaments are incised, and the joint capsule is entered, exposing the scaphoid.
The nonunion site is identified by passing a periosteal elevator between the proximal and distal fragments ( Fig. 26.9 ). Fluoroscopy is used to confirm the nonunion site ( Fig. 26.10A–B ).
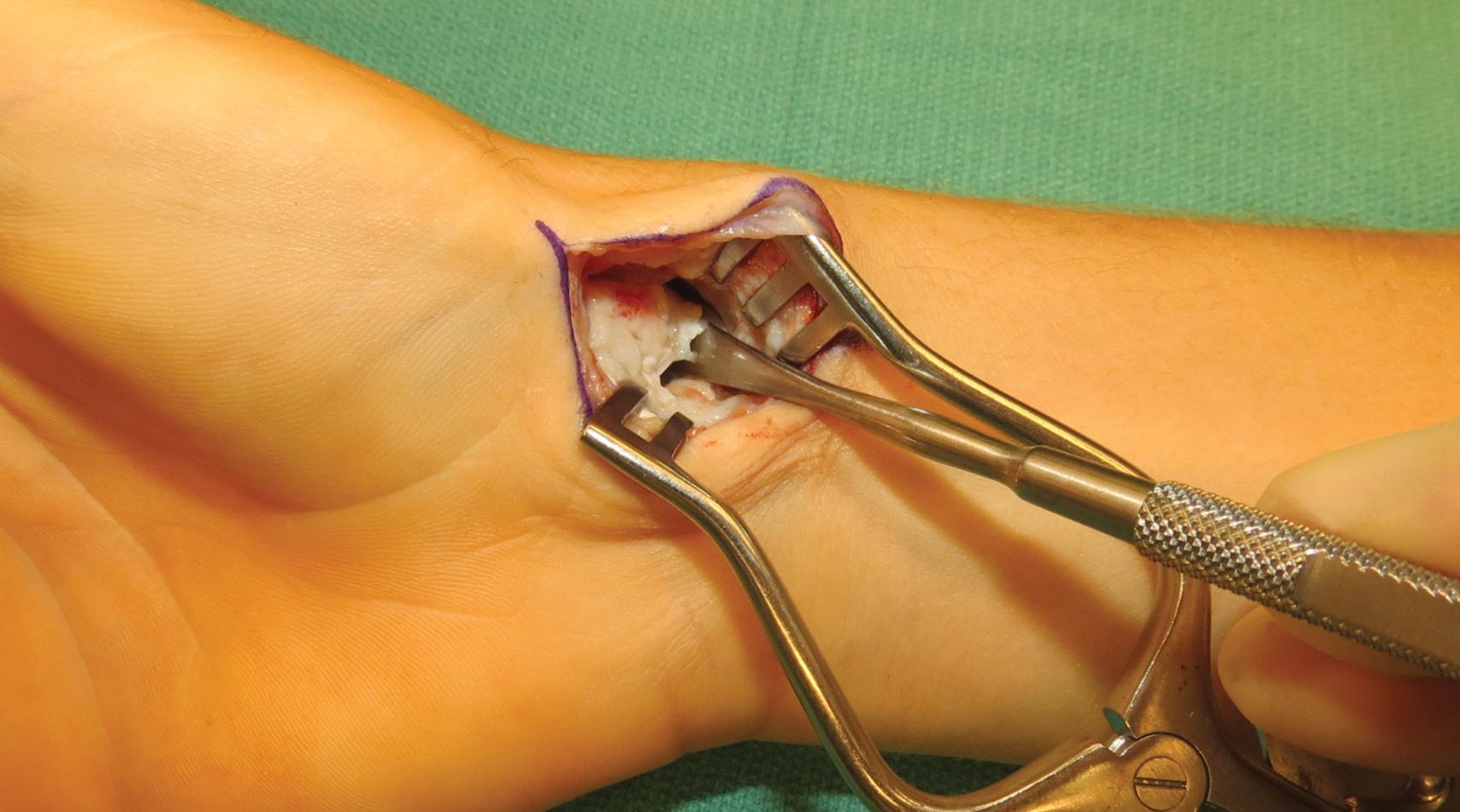
A curette or rongeur can be used to debride the scaphoid to healthy-appearing bone. Look for punctate bleeding as one potential indicator of healthy bone. Necrotic bone is typically whitish and hard, whereas the healthier bone has more of a porous, cancellous consistency.
The LRL and a portion of the RSC ligament should be preserved to stabilize the proximal pole of the scaphoid and maintain reduction.
A 5-cm longitudinal incision, centered over the proximal ulna, is performed 1 cm distal to the tip of the olecranon ( Fig. 26.11 ).

The incision is continued to the level of the periosteum.
The amount of bone necessary to bridge the gap in the scaphoid after debridement should be estimated. This often is approximately 5 mm wide by 10 mm long by 5 mm deep.
The flat portion of the ulna, near the tip of the olecranon, should be used for the bone graft harvest.
The template is measured and marked on the ulna ( Fig. 26.12 ). The periosteum overlying the graft is incised longitudinally and dissected carefully to facilitate reapproximation after graft removal.
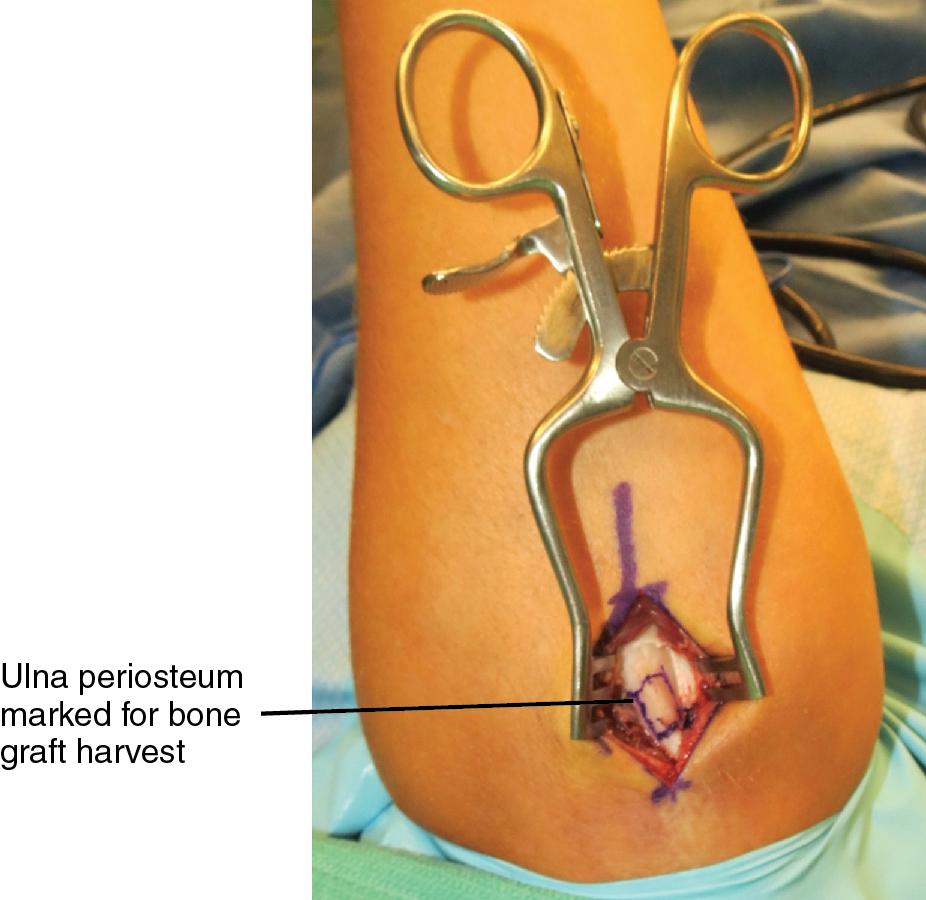
A 5-mm osteotome can be used to harvest the bone graft.
To extricate the graft, a 45-degree osteotomy is performed, approximately 1 cm distal to the distal end of the graft. This will permit an osteotome to be introduced at approximately 5 mm deep within the cancellous bone of the ulna. The graft can be separated from the remaining cancellous bone by using a straight or curved osteotome ( Fig. 26.13 ).

Preserving periosteal flaps during the approach to the bone graft harvest site will permit reapproximation during closure.
If necessary, the graft is trimmed to fit within the gap in the scaphoid.
The cortical portion of the graft is positioned along the volar cortex of the scaphoid to resist compression.
With the graft in position, two 0.045-in (1.14-mm) Kirschner wires (K-wires) are used to secure the graft.
The K-wire enters the scaphoid along its distal tubercle and is directed through the graft toward the proximal ulnar corner of the scaphoid ( Fig. 26.14A ).
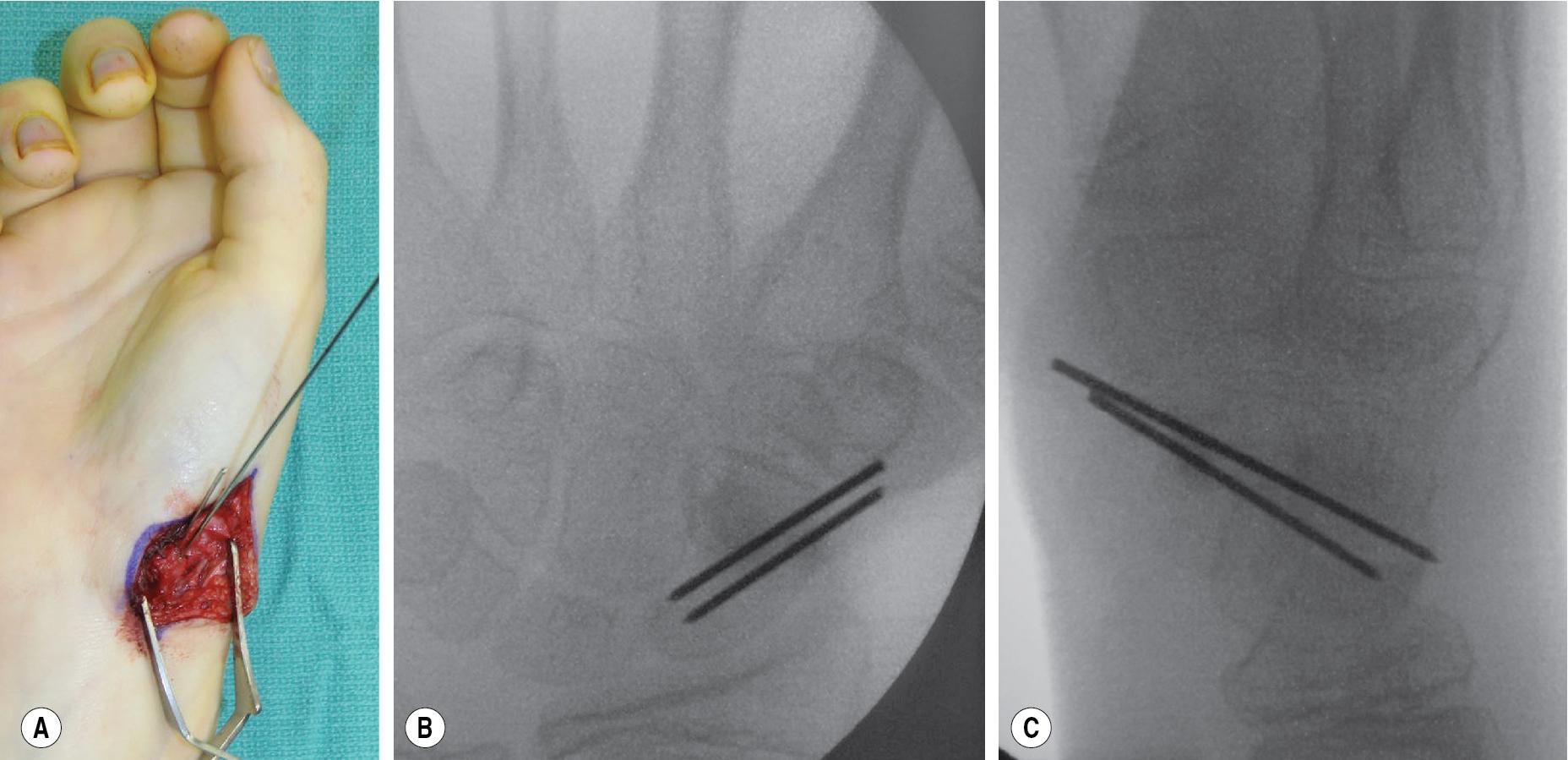
A second K-wire is directed collinearly to prevent rotation.
The position of the K-wires should be confirmed fluoroscopically (see Fig. 26.14B–C ).
The K-wires are cut and buried under the skin for later removal.
If a cannulated screw is available, the screw can also be used for fixation. The initial K-wire should be the guidewire for the screw, and the screw, rather than K-wires, can then be used for internal fixation ( Fig. 26.15 ).

The wrist should be taken through range of motion (ROM) after placement of the K-wires/screw to ensure that the graft is secure.
The wrist capsule is closed using 3-0 Ethibond sutures.
The periosteum of the elbow donor site is closed using 3-0 Vicryl suture.
The skin is closed with either 4-0 Monocryl or 4-0 polydioxanone (PDS).
Because the skin overlying the olecranon is thin, permanent suture material to close the periosteum should be avoided because the knots will be palpable.
Indications for pedicled vascularized bone graft:
Established nonunion without humpback deformity
If a humpback deformity is identified, a volar pedicled bone graft can be considered versus medial femoral condyle (MFC; see later section).
Evidence of avascular necrosis of the proximal scaphoid pole
Both the distal radius donor site and scaphoid recipient site are prepped and draped into the same operative field.
A 6-cm curvilinear incision is designed over the dorsoradial wrist in preparation for scaphoid debridement and bone graft harvest ( Fig. 26.16 ).
Branches of the superficial radial nerve should be identified and protected.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here