Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The pectoralis major (PM) muscle functions as a potent flexor, adductor, and internal rotator of the shoulder, as well as a dynamic stabilizer of the glenohumeral joint ( ).
Although the PM is not required for activities of daily living ( ), rupture of the tendon or muscle–tendinous junction leads to significant functional deficits and limitations of athletic performance or labor-intensive activities ( ).
Nonoperative treatment is reserved for partial tears, contusions, rupture at the muscle belly, and complete tears in older adult and low-demand patients ( ).
Although patients with low functional demand can recover reasonable function during activities of daily living ( ), athletes and laborers are unable to return to their preinjury levels of activity ( ).
For young active athletes, surgical treatment provides optimal strength, cosmesis, satisfaction, and return to sports ( ; ; ).
Advanced imaging is recommended to facilitate the timely diagnosis of acute injuries and is recommended when there is concern regarding injuries to the PM muscle or tendon ( ).
The chronicity of the injury should be taken into account, but it should not preclude surgical repair given that successful outcomes can still be achieved ( ).
When the history, physical examination, and appropriate PM specific imaging confirm the diagnosis, the athlete is indicated for surgery. The patient is positioned in the beach-chair position, and the repair is performed though either a deltopectoral or anterior axillary approach ( ). Meticulous dissection and retraction is required to avoid injury to the pectoralis nerves, especially inferior and medial to the coracoid ( ). The long head of the biceps sits medial to the PM insertion, and the surgeon should remain cognizant of this during surgical fixation.
Various repair techniques to reattach the tendon back to its footprint have been described in the literature ( ) ( Fig. 21.1 ). These techniques include tendon to tendon, bone trough ( Fig. 21.1, A ), suture anchors ( Fig. 21.1, B ) and cortical button repairs ( Fig. 21.1, C ). Although atypical, when enough healthy tissue remains attached to the insertion site, direct suturing of the tendon ends has been described for intratendinous tears ( ). For the majority of tears, sutures are passed through the ruptured tendon using either a modified Krakow or modified Mason Allen suture technique, which is then securely repaired to bone with either a transosseous method or more commonly with suture anchors or buttons.
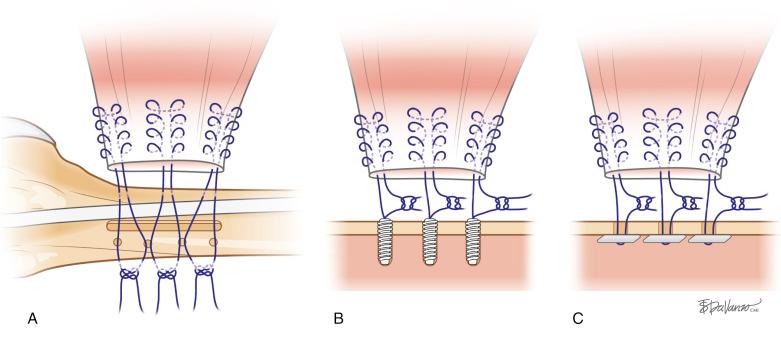
The bone trough technique has been described using a 5-cm vertical trough that is created at the footprint which is lateral to the bicipital groove. Four 2-mm drill holes are placed 1 cm lateral to the trough. Nonabsorbable sutures, fixed to the ruptured tendon, are then passed into the trough and into the drill holes, and are then tied over the bone bridge ( ). For both the suture anchor and the cortical button techniques, the footprint is cleared from soft tissue and lightly abraded to prepare for tendon to bone healing without structurally compromising the cortex. With the suture anchor technique, two or three anchors preloaded with high-strength suture are applied within the footprint. One of the suture limbs of each anchor is secured to the tendon and then is tied to the other limb ( ). For the cortical button technique, three 3.2-mm unicortical drill holes are made within the footprint with an adequate bone bridge between sites. The button is designed to flip in the intramedullary canal, which allows unicortical engagement on the near cortex. The titanium buttons are preloaded with one or two high-strength nonabsorbable sutures. One limb of each suture is secured to the tendon. Some buttons serve as suture anchors, and the limbs are simply tied to one another pushing the tendon to the footprint; other buttons are of the tensioning variety and may be used to pull the tendon to the footprint ( ).
Several biomechanical cadaver studies have been done to evaluate the different techniques of PM tendon repair. compared bone trough and suture anchor techniques and found no difference on ultimate load to failure. The mode of failure was fracture in 50% of the bone trough group and suture breakage in 100% of the suture anchor group. compared the three techniques (bone trough, suture anchor, and button techniques) and found a slightly higher load to failure on the bone trough group (596 N) compared with the suture anchor group (383 N). The modes of failure were suture breakage in nine specimens and fracture in one specimen for the bone trough, suture breakage in all cortical button specimens, and failure of the suture eyelet in five specimens and suture breakage in the other four specimens in the suture anchor group. compared the three repair techniques and found no differences in load to failure, elongation, linear stiffness, initial excursion, cyclic elongation, or footprint restoration. All three techniques failed at the suture tendon interface. They reported a significantly greater stiffness and maximal load (1455 N) in the intact tendon specimens.
There is general agreement that all three repair techniques described here are adequate to repair a PM tendon rupture. Although some investigators favor suture anchor and cortical button repairs, given that there is less dissection laterally on the humerus compared with the bone trough technique ( ).
There is a lack of general agreement on the definition of acute versus chronic in PM injuries. , in their systematic review, defined chronic injuries as those beyond 6 weeks. As with several other surgical interventions, chronicity of the injury may increase risk of surgical morbidity because it requires greater surgical exposure and dissection of scar tissue to mobilize the retracted muscle ( ). Moreover, in some chronic injuries, the tendon length is insufficient to allow for primary repair with minimal tension and requires reconstruction or augmentation with either autograft or allograft. Extended chronicity of the injury should not preclude surgical intervention given that good outcomes can still be achieved ( ).
After surgical repair, patients are instructed to remain in a sling for 4 to 6 weeks, with the arm in internal rotation and adducted ( ). By week 6, passive motion in all planes is allowed with the assistance of the physical therapist. At the 8-week postoperative phase, periscapular and isometric strengthening exercises are added. After week 12, the patient should have near full range of motion and light resistance, and strengthening exercises are started ( ). Additional strengthening and sport-specific rehabilitation progress for the next 12 weeks with a goal of unrestricted activity by 6 months postoperatively, when full range of motion and strengthening are achieved ( ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here