Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Percutaneous placement of inferior vena cava (IVC) filters and treatment of superior vena cava obstruction (SVCO) ( Ch. 44 ) are the cornerstones of venous intervention. Venous angioplasty, stenting and thrombolysis are sometimes performed but remain controversial techniques, except in the management of haemodialysis access ( Ch. 50 ). The principles of negotiating and treating venous stenoses and occlusions are exactly the same as in the arterial system. This chapter covers some established indications for venous intervention and details aspects of intervention specific to the venous system.
IVC filters are placed to prevent pulmonary embolism from sources in the lower limbs, pelvis and IVC. Contemporary devices are readily placed percutaneously via the right internal jugular vein (IJV) or femoral veins. Several permanent and retrievable filters are commercially available. Most retrievable filters can be left permanently in place.
There is little evidence to support the use of IVC filters, and patients should be considered on a case-by-case basis ( Table 51.1 ). Thrombosis rates vary between devices; overall, about 10% of permanent IVC filters will thrombose within 5 years. Therefore, permanent filters should be avoided whenever possible in those patients with a long life-expectancy.
| Indication | Filter type |
|---|---|
| Unequivocal | |
| Recurrent PE despite adequate anticoagulation | P |
| Patients with PE and severely limited cardiorespiratory reserve | P |
| PE with contraindication to anticoagulation | P |
| Relative | |
| Free-floating iliofemoral/IVC thrombus with a high risk of embolization | P/R |
| Spinal cord injury with paraplegia | P |
| Severe trauma | P/R |
| Prophylactic – before surgery on patients at high risk of DVT or PE, e.g. before hip surgery in the presence of ipsilateral femoral DVT | R |
Introducer sheaths for IVC filters start at 7F; insertion of large catheters into the femoral vein is itself a cause of deep vein thrombosis (DVT), hence the jugular approach has a distinct advantage!
Ultrasound for right IJV puncture
Basic angiography set
Cobra catheter
Three-mm J guidewire
An appropriate IVC filter set (see below).
IVC filters are supplied with delivery systems designed for use from either the jugular or the femoral approach. These systems are not interchangeable, so make sure that you have the correct device! Check also that you have an appropriately sized device for the IVC.
The right IJV is the ‘universal gateway’ and can be used for access even in the presence of iliofemoral DVT. Make sure that there is a contemporary ultrasound to document the site and extent of thrombus. Placing a catheter through a thrombosed vein is likely to result in iatrogenic pulmonary embolism (PE)!
From the jugular route, use a Cobra catheter and 3-mm J-guidewire to carefully negotiate through the right atrium to the IVC.
Assessment is required for three reasons:
To demonstrate the patency of the IVC, assess its size and any angulation
To confirm conventional anatomy, i.e. single IVC
To document the position of the renal veins.
In practice most patients will have had a contrast-enhanced computed tomography (CECT), which demonstrates the anatomy and IVC size, leaving you only needing to establish the position of the renal veins.
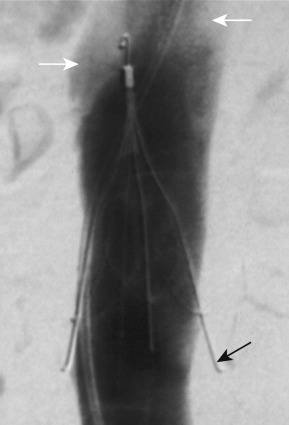
If digital subtraction angiography (DSA) is required it is usually sufficient to perform a simple IVC injection through a pigtail catheter placed just above the confluence of the iliac veins. An initial gentle hand injection will ensure that there is no thrombus adjacent to the catheter; perform a more vigorous injection to demonstrate the entire IVC. The position of the renal veins is usually apparent because of streaming of unopacified blood ( Fig. 51.1 ). If the renal veins cannot be identified, use a Cobra catheter to engage them and perform selective hand injections to demonstrate their position.
Use the patient's spine as a reference for the position of the renal veins.
Once the position of the renal veins has been established, do not move the table or the image intensifier.
If you did not measure it on the CT scan, do not forget to measure the diameter of the infra-renal IVC. Most IVC filters can only be used within a specified range of IVC diameters; if the filter is too small, the first place it will lodge is the tricuspid valve!
There are two sites to place an IVC filter, and the position is determined from the cavogram.
Infrarenal: this is the optimal site; if the filter causes IVC thrombosis, the renal veins will be spared. Conical filters should be placed with the filter apex at the level of the renal veins; the high flow promotes dissolution of thrombus trapped or formed within the filter.
Suprarenal: in the presence of infrarenal thrombus, a filter can be sited between the renal and hepatic veins. In this position, filter thrombosis can lead to renal vein thrombosis and renal infarction.
Each type of filter is deployed differently and there may even be differences for a single type of filter, depending on whether the jugular or femoral route is used. Read the instructions carefully before use; if you do not understand them, seek help! It is traditional, but unnecessary, to perform a completion venogram to demonstrate the position of the filter; a single-shot image will suffice. If you must do this, consider injecting through the sheath and take great care if you pass a pigtail catheter or J-wire through the filter as they might become entangled!
If there is no contraindication, the patient should be anticoagulated while the filter is in situ, to minimize the chance of filter thrombosis.
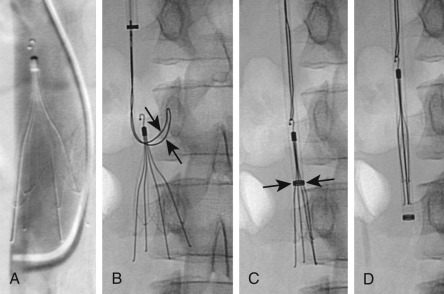
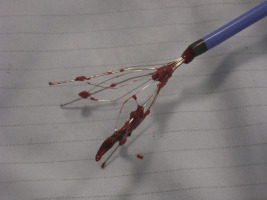
There is no absolute consensus on the length of time a filter can be left in place before removal is attempted. Longer dwell times are associated with greater complications and the filter should be removed as soon as it is no longer clinically required. Always perform a cavogram ( Fig. 51.2 ) to see if there is any residual thrombus either in the filter or which would threaten significant PE. If there is <1 cm 3 of thrombus in the filter, it can be removed. Most removable filters have a hook at their apex, this is snared from the jugular vein. The snare must be placed at the top of the hook; the snare is held in place and the sheath advanced over it to close the filter ( Fig. 51.2 ). There is almost always thrombus/tissue on the filter struts ( Fig. 51.3 ).
If there is difficulty STOP! DO NOT USE FORCE. Accept that it may not be possible to remove the filter. It is better to leave a permanent filter than cause an IVC laceration.
If filter retrieval is difficult it is often worth stopping and obtaining a CT of the abdomen.
Significant procedure-related complications are rare and include:
Femoral vein thrombosis was particularly common with early devices but is only seen in 2–3% of patients with smaller contemporary devices.
Filter struts may perforate the caval wall ( Fig. 51.1 ); this is rarely clinically significant but may make the filter irretrievable. Caval strut perforation is common and is best assessed on CT.
There are four forms of incorrect deployment:
Malposition in relation to the renal veins
Incorrect filter sizing. At worst, this will result in fatal embolization of the filter. More commonly, it results in tilting or incorrect opening
Conical filters can be tilted; this may reduce filter effectiveness
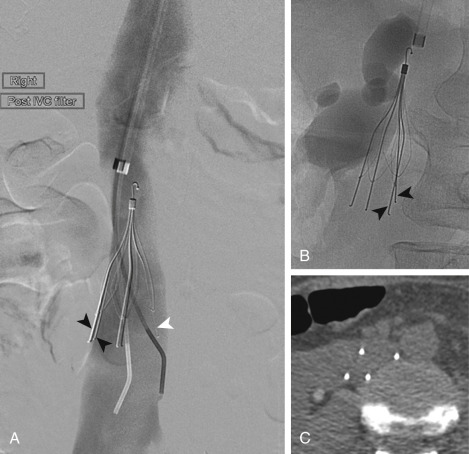
The filter may open incorrectly so that the struts are not evenly distributed or appear not to reach the IVC wall. This may impair filter function. If you have any doubt, perform a limited CT to clarify the situation ( Fig. 51.4 ).
If you have placed a permanent filter, you are stuck, whereas a removable filter can be repositioned. If there is severe misalignment, a second filter may have to be placed above the first.
Try to deploy the filter in a straight portion of the IVC; it is more likely to be effective and much easier to remove.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here