Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Trauma describes injuries caused by physical forces. These may be blunt, penetrating, thermal, or any combination of the three. As the leading cause of death in patients under 45 years of age, it is imperative that the on-call surgeon be able to appropriately recognize, respond to, and triage the traumatically injured patient.
What is the estimated time and mechanism of arrival of the patient?
You can triage your response time based on the time and the method of arrival (patient dropped off, arrived by ambulance, or airplane/helicopter). Be prepared before the arrival of the patient.
What is the triage classification of the patient?
Trauma occurs within a range of severity including the severely injured (i.e., a hypotensive patient with large traumatic injuries) to the minor injury (i.e., skateboard crash leading to superficial wounds). Patients typically arrive and are triaged through local emergency medical services (EMS), which may be further modified by the institution based on injury characteristics. Knowing the patient’s activation level (minor vs. major) will help you prepare for what may come through the doors.
What is the mechanism of injury?
It is important to classify in your mind whether the patient is traumatically injured from a blunt or penetrating trauma. Additionally, ascertain if multiple patients are in route (e.g., as in a transportation-related crash). Mechanisms of trauma (e.g., a pedestrian hit by car) can have predictable patterns of injury.
What are the patient’s vital signs en route or at the scene of injury?
Tachycardia is the first sign of hemorrhagic shock. Being prepared for an unstable, hypotensive patient is crucial. Note that on occasion there will be discrepancy between the reported vitals signs and patient’s condition in the field compared with what is observed when the patient arrives in the trauma bay/resuscitation area.
What is the patient’s Glasgow Coma Scale (GCS)? Has this changed since paramedics arrived on scene?
It is important to be prepared for intubation and an urgent computed tomography (CT).
What is the patient’s current intravenous (IV) access?
A hypotensive trauma patient is in hemorrhagic shock until proven otherwise. It is imperative to have adequate IV access for resuscitation and possible transfusion.
What medical problems does the patient have?
Diabetes (hypoglycemia), Cardiac disease (e.g., dysrhythmias, myocardial infarction [MI], valvular disease), and neurologic conditions can all be important with possible syncope leading to vehicular crashes. Presence of blood thinners is crucial for evaluating and monitoring a possible traumatic brain-injured patient. A list of potential anticoagulation reversal agents for use in intracranial hemorrhage is in included in Table 30.1 . Consultation with neurosurgical specialists and hospital pharmacists are advised before administration of these agents in the setting of blood thinners and intracranial hemorrhage.
| Anticoagulant | Reversal Agent | Management Steps |
|---|---|---|
| Vitamin K+ antagonist reversal (warfarin) | Vit K (10 mg IV) 3- or 4-factor PCC (if INR ≥1.4) Weight-based dosing FFP if PCC unavailable 10–15 mL/kg IV |
Discontinue medication. 4-factor preferred over 3-factor PCC Serial INR testing, goal <1.4 |
| Direct thrombin inhibitor (Dabigatran, etc.) | Administer activated charcoal (50 g) Intubate if risk for aspiration If within 2 h last of dose Idarucizumab (5 g IV, 2 divided doses) Activated PCC (50 u/kg) OR 4-factor PCC (50 u/kg) Consider hemodialysis for dabigatran-related major hemorrhage |
Discontinue medication Obtain time/dose of last dosage Base reversal off of presence of major/intracranial bleeding (not laboratory findings) Consider renal insufficiency, discuss with pharmacist. Use a PCC if idarucizumab unavailable or direct thrombin inhibitor other than dabigatran used. Factor Xa inhibitors cannot be dialyzed off. Current consensus favors against use of FFP or recombinant factor VIIa in direct thrombin inhibitor related intracranial hemorrhage. |
| Unfractionated heparin | IV protamine (1 mg/100 u given in last 2–3 h; maximum single dose 50 mg) | Discontinue medication. Reversal advised for full-dose heparin. Do not routinely need to reverse prophylactic-dose heparin. Administer protamine slowly, monitor for hypotension and anaphylaxis |
| Low-molecular weight heparin (LMWH) | Consider IV protamine. Consider recombinant factor VIIa if protamine contraindicated. |
Discontinue medication. Protamine may not work. Consult pharmacist. Recommend against reversal of prophylactic-dose LMWH. Recommend against reversal with FFP or PCCs. |
| Polysaccharides (fondaparinux, etc.) | Activated PCC (20 IU/kg) Recombinant factor VIIa if aPCC contraindicated or unavailable (90 mcg/kg) |
Discontinue medication. Recommend against protamine for reversal. Consider against reversal in prophylactic-dosage without evidence of bioaccumulation or impaired clearance. |
| Antiplatelet medications | Platelet transfusion (1 apheresis unit) Consider DDAVP; if aspirin/COX-1 inhibitors or ADP receptor inhibitor Consider DDAVP in uremia-related platelet dysfunction |
Reversal recommended only if patient requires neurosurgical intervention. Consider platelet function testing before transfusion of platelets. Consult neurosurgery if reversal related to intracranial bleeding. |
Typically, the trauma or resuscitation bays should be set up in advance. If not, make sure the support staff has the following equipment is ready:
Airway cart
Including bag-mask ventilator, oxygen with tubing, and medications for possible intubation. Medications for rapid sequence induction: etomidate 0.3mg/kg IV push OR thiopentone 3 to 7 mg/kg IV bolus at induction, succinylcholine 1.5 mg/kg IV push once asleep (See Table 30.2 ). Wait for fasciculation to stop before direct laryngoscopy
| Drug | Dosage | Notes |
|---|---|---|
| Sedation/Induction | ||
| Etomidate | 0.2–0.3 mg/kg IV (15–20 mg in a 70-kg adult). Onset 30–60 sec, duration 10 min |
|
| Ketamine | 1–2 mg/kg IV (70–140 mg in 70-kg adult) Onset 30–60 sec, duration 5–10 min |
|
| Fentanyl | 2–5 mcg/kg IV (150–350 mg in 70-kg adult) |
|
| Propofol | 1–2 mg/kg IV (70–140 mg in 70-kg adult) |
|
| Thiopental | 3–5 mg/kg IV (210–350 mg in 70-kg adult) |
|
| Neuromuscular Blocking Agents | ||
| Succinylcholine | 1–2 mg/kg IV (70–140 mg in 70 kg adult). Onset 1 min, duration 5–7 min |
|
| Vecuronium | 0.08–0.10 mg/kg IV (5–7 mg in 70-kg adult). Onset 2–3 min, duration 30–35 min | |
| Rocuronium | 0.6–1.2 mg/kg IV (45–85 mg in 70-kg adult). Onset 60–90 sec, duration 20–30 min |
|
Ventilator for possible intubation
Cricothyroidotomy tray if available
Thoracotomy tray if available
Tube thoracostomy tray if available
Adequate IV access
Ideally, they should have enough 16-gauge IVs to be able to properly resuscitate. If the patient is in shock, sometimes an intraosseous or central venous catheter will need to be placed. The appropriate kits should be present (see Chapter 19 for central venous catheter placement).
IV fluid, at least 2 liters of crystalloid should be present. Warm fluids are preferred if available.
Lactated Ringer’s (LR) or 0.9% normal saline (NS) are appropriate resuscitative fluids. Avoid LR in head-injured patients or those with known renal disease.
Appropriate notification to the blood bank.
Should a severely traumatically injured patient be arriving, the blood bank should be aware for massive transfusion of blood products.
Alert radiology to the potential patient in need of rapid radiographic interpretation.
What are the major causes of trauma?
Blunt trauma
High speed
Motor vehicle collision
Motorbike/Motorcycle collision
Manpowered vehicle (e.g., bicycle) collision
Other rare causes, including aircraft, etc.
Fall from height
Explosion
Low speed
Ground-level fall
Crush injuries
Penetrating trauma
High velocity
Rifle
Low velocity
Handgun
Shotgun
Stab wounds
A hypotensive trauma patient is in hemorrhagic shock until proven otherwise. There are 5 potential spaces for the bleeding to occur:
Chest
A patient can bleed a one-third of his or her blood volume into each hemithorax.
Abdomen
Solid organs, especially the liver, kidney and spleen, are potential sources for ongoing hemorrhage requiring varied management, from close observation to urgent surgical intervention. Radiographic grading of these solid organ injuries can be found in Tables 30.3 to 30.5 .
| Grade a | Injury Type | Description of Injury |
|---|---|---|
| I | Hematoma | Subcapsular, <10% surface area |
| Laceration | Capsular tear, <1 cm parenchymal depth | |
| II | Hematoma | Subcapsular, 10%–50% surface area intraparenchymal, <5 cm in diameter |
| Laceration | Capsular tear, 1–3 cm parenchymal depth that does not involve a trabecular vessel | |
| III | Hematoma | Subcapsular, >50% surface area or expanding; ruptured subcapsular or parenchymal hematoma; intraparenchymal hematoma ≥5 cm or expanding |
| Laceration | >3 cm parenchymal depth or involving trabecular vessels | |
| IV | Laceration | Laceration involving segmental or hilar vessels producing major devascularization (>25% of spleen) |
| V | Laceration | Completely shattered spleen |
| Vascular | Hilar vascular injury with devascularized spleen |
| Grade a | Injury Type | Description of Injury |
|---|---|---|
| I | Hematoma | Subcapsular, <10% surface area |
| Laceration | Capsular tear, <1 cm parenchymal depth | |
| II | Hematoma | Subcapsular, 10%–50% surface area intraparenchymal, <10 cm in diameter |
| Laceration | Capsular tear, 1–3 cm parenchymal depth, <10 cm in length | |
| III | Hematoma | Subcapsular, >50% surface area of ruptured subcapsular or parenchymal hematoma; intraparenchymal hematoma >10 cm or expanding |
| Laceration | >3 cm parenchymal depth | |
| IV | Laceration | Parenchymal disruption involving 25%–75% hepatic lobe or 1–3 Couinaud’s segments |
| V | Laceration | Parenchymal disruption involving >75% of hepatic lobe or >3 Couinaud’s segments within a single lobe |
| Vascular | Juxtahepatic venous injuries (i.e., retrohepatic vena cava/central major hepatic veins) | |
| VI | Vascular | Hepatic avulsion |
| Grade a | Injury Type | Description of Injury |
|---|---|---|
| I | Contusion | Microscopic or gross hematuria, urologic studies normal |
| Hematoma | Subcapsular, nonexpanding without parenchymal laceration | |
| II | Hematoma | Nonexpanding perirenal hematoma confined to renal retroperitoneum |
| Laceration | <1 cm parenchymal depth of renal cortex without urinary extravasation | |
| III | Laceration | >1 cm parenchymal depth of renal cortex without collection system rupture or urinary extravasation |
| IV | Laceration | Parenchymal laceration extending through renal cortex, medulla, and collection system |
| Vascular | Main renal artery or vein injury with contained hemorrhage | |
| V | Laceration | Completely shattered kidney |
| Vascular | Avulsion of renal hilum which devascularizes kidney |
Pelvis
Pelvic bone fractures can result in tearing of the pelvic veins, which can lead to severe blood loss. Closing the potential space of the pelvis with a pelvic binder can help tamponade the bleeding. A simple folded bed sheet tightly wrapped around the patient over the greater trochanters and fastened tightly with a clamp can be life saving
Long bones
A patient can lose 1 to 2 liters of blood from a long bone fracture (i.e., a femur fracture). Placing the long bone in traction to reduce the fracture can help slow the bleeding and reduce further vascular injury from bony edges.
Floor/Scene of injury
Although the blood is not sequestered into a cavity, large scalp lacerations can bleed significantly, often leaving blood at the scene. Estimates of blood loss at the scene are generally regarded as inaccurate, but can give a sense of what stage of shock to anticipate. A scalp laceration can produce severe blood loss; clips or suture ligature can be used to quickly control a scalp laceration.
Airway Obstruction
Every proper trauma assessment begins with the airway to evaluate for obstruction. The patient could have significant maxillofacial trauma and soft-tissue edema that prevents against adequate ventilation.
Tension Pneumothorax
This should be a prompt clinical diagnosis. As a hemithorax fills up with air from a one-way ball valve mechanism, the ipsilateral lung collapses and the mediastinum shifts opposite to the injured side. Venous return to the right ventricle is impaired because of the increased intrathoracic pressure resulting in decreased cardiac output. The patient will be in extremis with hypotension and decreased breath sounds on the side of the pneumothorax. The trachea may be deviated away from the pneumothorax and distended neck veins can be observed. Promptly place a large IV (angiocatheter) in the second intercostal space in the midaxillary line to relieve the pressure. The patient will require a tube thoracostomy to follow (see Chapter 28 ).
Cardiac Tamponade
As blood fills the pericardial space, the increasing pressure decreases the filling capacity of the heart. Preload to the heart precipitously decreases. The patient will present with hypotension and an elevated jugular venous distention (JVD). Muffled heart sound may be difficult to illicit in the often chaotic and noisy trauma/resuscitation room. A pericardiocentesis can be performed for short-term management, although the patient will need a definitive drainage procedure for the pericardium (e.g., pericardial window; see Chapter 28 ).
Open Pneumothorax
A patient with a large thoracic injury with missing overlying thoracic wall can have a pleural cavity in continuity with the air. This can cause a large open pneumothorax. Treatment involves an occlusive dressing and tube thoracostomy until definitive management can be performed.
Massive Hemothorax
Blunt thoracic injury can cause significant rib fractures with laceration and injury to the associated intercostal arteries. A patient can bleed up to one-third of their overall blood volume into each hemithorax. The patient will present with hypotension, decreased breath sounds, and likely signs of chest wall trauma. A tube thoracostomy that evacuates more than 1000 mL on initial placement defines a massive hemothorax.
Flail Chest
A flail chest occurs when there are multiple consecutive ribs, each with multiple fractures causing areas with “floating ribs.” The injury results in paradoxical movement of the chest wall such that the flail segment shifts in with inspiration because of the negative inspiratory force and no bracing from other ribs and likewise shifting out with exhalation. The flail segment can impair breathing dynamics and is usually associated with significant pulmonary contusions.
A patient who arrives hypotensive and bradycardic could be in neurogenic shock. An injury to the spinal cord can damage the sympathetic response to the vasculature causing systemic vasodilation from lack of vascular tone and an inappropriate parasympathetic response to the myocardium, causing bradycardia. Hemorrhagic shock must first be ruled out, but neurogenic shock can be common in spinal cord injury patients. Mild doses of peripherally acting vasopressors ( phenylephrine 50–200 μg IV every 1–5 minutes ) can help with the vascular tone and prevent hypotension
Traumatic patients arriving after a motor vehicle accident could have had a myocardial event leading to the loss of control. A 12-lead electrocardiogram (ECG) is an important adjunct test for any traumatically injured patient.
First, do not panic . A coordinated team effort is required in the evaluation and management of a traumatically injured patient. Before the patient’s arrival it is important to establish good communication between the members of the trauma resuscitation effort. Every hospital system is different, but defining preassigned roles before patient arrival can help facilitate an expedient and well-run resuscitation. One method is shown in Fig. 30.1 .
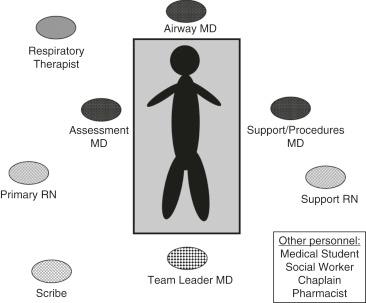
As the on-call physician, you are likely to be at the patient’s bedside as the assessment physician performing a full head-to-toe physical examination, termed a primary and secondary survey. Your chief resident or attending will likely be the team leader.
The primary survey is designed to identify immediate, potentially reversible threats to life. Be systematic. Do not move on if an issue arises in “A,” “B,” or “C.” If there is a change in a status of a patient, return to “A” and reevaluate systematically.
A = Airway
Assess: Always assess airway with cervical spine control. Ask the patient their name and evaluate for their ability to phonate.
If there is significant maxillofacial trauma, intubation may be necessary to control the airway
A GCS <8 requires placement of a definitive airway as the patient may not protect their airway
You can chin lift or jaw thrust to help with airway before definitive management. Remember to always keep spinal precautions in mind.
B = Breathing and Ventilation
Assess: Listen for bilateral air entry with a stethoscope. If breath sounds are not identifiable on one side, consider pneumothorax and evaluate for signs of tension physiology (hypotension, tracheal deviation, distended neck veins).
Make sure continuous pulse oximetry is on the patient. Optimize oxygenation with high-flow O 2
Tube thoracostomy may be required for tension pneumothorax or hemothorax. For hemothorax, consider having an auto-transfusion pneumovac available.
C = Circulation and Hemorrhage Control
Assess: Assess consciousness level and skin color. Look for active blood loss from laceration. Feel central pulses (femoral/carotid) and confirm equal laterality. Stop obvious, active, life-threatening bleeding. Ensure adequate vascular access.
Have at least two large bore (16-gauge) IVs in the antecubital fossa. If there is a need for massive transfusion, a large-bore central venous catheter can be placed. Typically in the trauma situation, femoral or subclavian access is preferred (refer to Chapter 19 on IV access).
Have 2 liters of crystalloid ready; warm fluids are preferred.
Type and cross
Have blood available; consider whether your hospital’s massive transfusion protocol must be initiated.
D = Disability
Assess:
Pupil reaction and symmetry. Symmetrically dilated pupils can be a sign of sign of high sympathetic tone or use of stimulants. Likewise, symmetrically constricted pupils can be a sign of opiate use. Unequal pupils can be a sign of herniation and warrant a prompt CT head without contrast. Unreactive pupils may also indicate intracranial injury.
GCS (See Table 21.1 )
Rectal tone
E = Exposure
Evaluate the entire body for injuries. It may be helpful to remove clothing; however, judgment should be used for minor injuries. In a severely injured patient, recommend fully exposing for complete assessment.
Cover with warm blankets to maintain euthermia.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here