Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Metastatic lesions account for over 50% of intracranial lesions in adults.
The most common primary locations of these metastases are lung, breast, skin and large intestine.
The majority of intracranial metastases occur at the grey–white matter junction in the supratentorial space.
Multiple metastases (>3 distinct lesions) are not uncommon.
The goals of treating brain metastases are to relieve mass effect, improve neurologic symptoms, establish a diagnosis and provide local disease control in the brain.
In general we aim to achieve en bloc resection of intracranial metastases, but this can be challenging, especially with large tumors that require significant retraction.
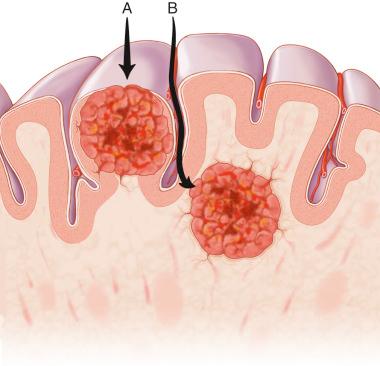
Because these tumors typically reside in the gray–white matter junction below the cortical surface, these tumors can be approached and resected either via a trans-sulcal or transcortical route ( Figure 3.1 ).
The decision to surgically resect supratentorial, intracranial metastases requires consideration of various factors, including the patient's age, functional status, control of primary tumor and presence of extracranial spread. These factors are all used to calculate a patient's recursive partitioning analysis (RPA) class.
Patients with good RPA class (class I–II), radiation-resistant tumors and lesions causing symptoms or mass effect (including seizures, motor deficit, headaches, hydrocephalus) are typically candidates for surgery. Historically, the number of intracranial metastases was used to determine whether a patient was a surgical candidate, but there remains conflicting evidence regarding resection of symptomatic lesions only.
Patients with poor prognoses are generally considered for radiation therapy, including whole brain radiation therapy (WBRT) and/or stereotactic radiosurgery (SRS).
The choice of approach is usually dictated by preoperative neuroimaging and tumor location. In the trans-sulcal approach the sulcus to enter is planned preoperatively, taking into account the anatomy of the vessels running within it and the areas of eloquence.
Intra-axial lesions in the subcortical space underlying an evident sulcus.
This approach is preferred for tumors underlying eloquent cortex, including somatosensory, language and visual cortex.
For tumors deep in the subcortical space (>1 cm), the trans-sulcal approach may allow easiest access for resection while minimizing disruption of the overlying cortical tissue, which is especially critical in eloquent areas.
Deep intra-axial lesions that require wider exposure to localize and resect the lesion.
Subcortical tumors that do not underlie an obvious sulcus and do not involve eloquent cortical regions.
This may provide a more direct access for operative resection than the trans-sulcal approach.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here