Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
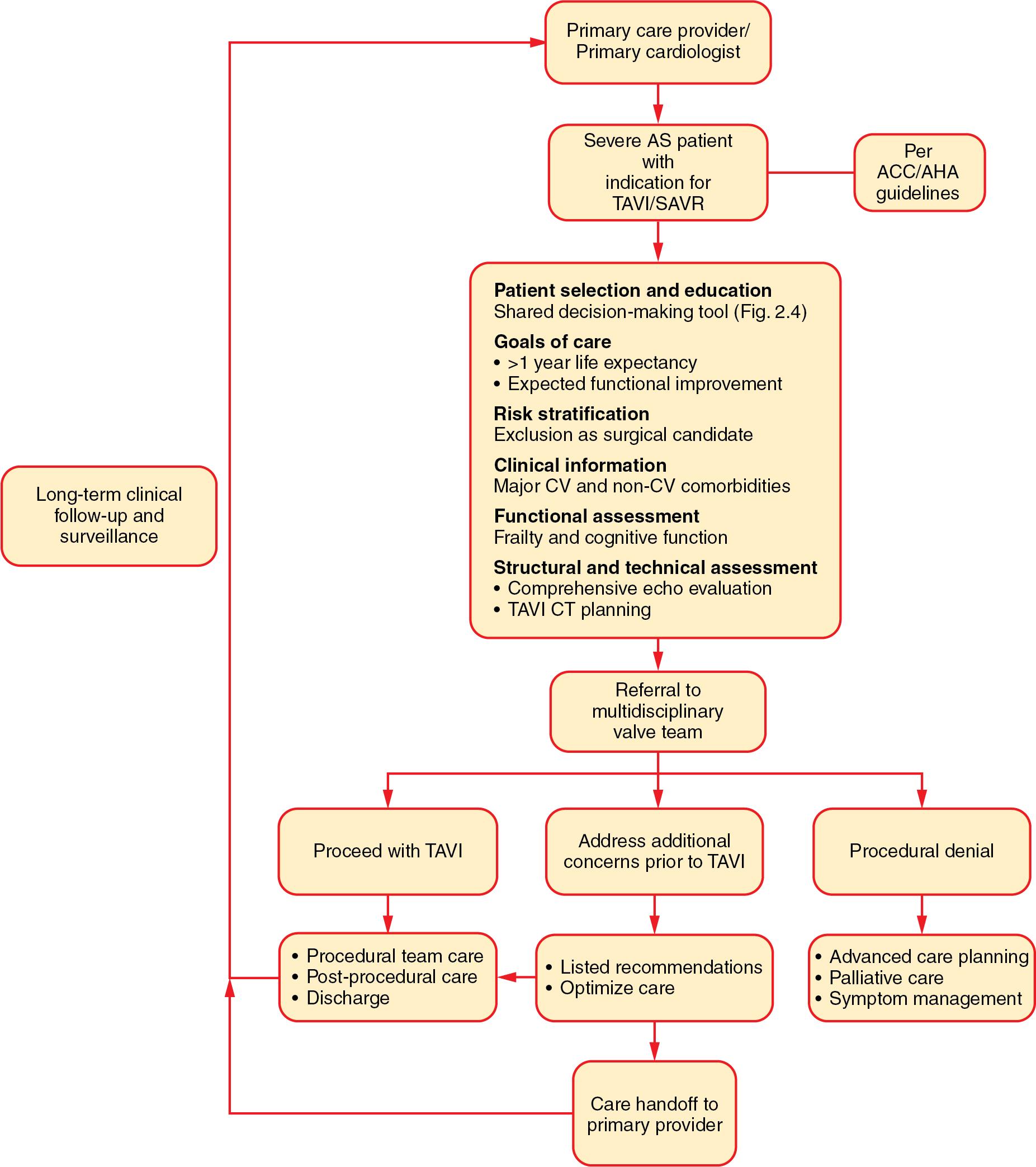
An effective system for the evaluation and management of patients with severe aortic stenosis (AS) requires a multilevel, graduated approach to identify patients with disease and refer them for therapy in a timely and efficient manner. The key guiding principle for a transcatheter aortic valve implantation (TAVI) center is to adopt a multidisciplinary and patient-centered approach that integrates the care of patients with AS, using guidelines published by large subspecialty groups as the framework for program development and individualized patient management. Ideally, care of adults with AS is integrated across health care systems, with patients moving seamlessly and efficiently between different tiers of care, while coordinating with the diverse primary care and subspecialty providers needed in management of AS patients, who often are older and have multiple comorbid cardiac and noncardiac conditions.
The clinical goals of an integrated system are simple:
Ensure efficient and cost-effective patient care.
Enhance the patient care experience.
Expand and promote equity of access to care.
Minimize time to diagnosis and to treatment.
Streamline and coordinate the pathway for assessment referral to a treatment center.
Optimize both procedural and long-term outcomes.
Promote a seamless transition of care back to the referring provider from the aortic valve intervention center.
At a systems and health policy level, the pursuit of an integrated care model for the treatment of AS supports the shift from “procedure-based” health planning to a more comprehensive “disease-focused” approach that supports continuity of care, multidisciplinary practice, and patient-centered best practices, including the use of shared decision-making along patients’ journey of care with valvular heart disease. A disease-focused approach is particularly salient to address the multiple challenges associated with the needs of the primarily older and medically complex AS population. The ideal integrated system of care provides coordination of care from the referring provider to primary and secondary valve centers, either with transfer of the patient for diagnostic or therapeutic procedures, or with communication, conventional or telemedicine, across the system. Similarly, there is a coordinated transfer of care back from the valve intervention center to the referring provider to ensure continuity of care ( Fig. 2.1 ).
A timely and accurate diagnosis of AS is primarily based on echocardiographic imaging requested once patients experience symptoms that might be due to AS, with the finding of a murmur on routine examination, or for unrelated reasons. Symptoms alone are not a reliable trigger for diagnosis of AS because symptoms develop gradually over many years and are not specific—exertional intolerance, shortness of breath, dizziness, and chest pain are common in older adults and most often are due to other causes. In fact, the presence of severe symptoms at the time of the initial diagnosis of AS is a harbinger of poor outcomes and requires immediate intervention.
The questions for an integrated health care system then are as follows: How can we diagnose AS in the absence of symptoms? Who is best suited to make the diagnosis of AS? What is the best diagnostic approach? Is there a role for more widespread screening for AS?
In the community, a patient’s care typically is managed by a general practitioner or other primary care provider (PCP), sometimes with intermittent visits to a general cardiologist. For many cardiovascular conditions, the patient first presents to a PCP with new symptoms, which then prompts evaluation and referral to subspecialty care. However, this referral pattern is unusual for patients with AS. Although some patients may be diagnosed when the PCP has a high index of suspicion for AS in an elderly adult with unexplained dyspnea, chest discomfort, or syncope, the more common first symptom of AS in older adults is a subtle decrement in exertional tolerance. This often is not mentioned by the patient to the PCP and may be difficult to elicit on a standard clinical review of symptoms.
More important, the goal is to diagnose AS before the onset of even subtle symptoms, which is problematic. Unfortunately, cardiac auscultation is not reliable for diagnosis of the presence or severity of AS, regardless of the level of training or experience of the health care provider. The sensitivity of auscultation for diagnosis of mild valvular heart disease is approximately 32%, which increases to only 44% with significant disease. Instead, early AS typically is identified incidentally on an echocardiogram performed for an unrelated indication. On the other hand, the specificity of a murmur is high (98% ), with current guidelines recommending echocardiography in asymptomatic patients with a significant systolic murmur (grade 3/6 or louder) or any diastolic murmur. It is also prudent to obtain an echocardiogram in a patient with symptoms that might be due to AS even if the murmur is soft or absent.
Given the prevalence of AS in older adults, the poor prognosis of untreated, severe disease, and the accessibility and utility of routine transthoracic echocardiography in the diagnosis of AS, there is increasing interest in and scrutiny of the role of broad echocardiographic screening. Although current guidelines do not recommend screening in asymptomatic adults without suggestive physical examination findings, studies suggest that population-level screening commonly detects valvular abnormalities. Further, point-of-care ultrasound (POCUS) is an ever-expanding field; small studies of POCUS by providers with limited training demonstrate a reasonable sensitivity and cost-effectiveness in screening elderly adults for AS. ,
On recognition, moderate to severe AS should prompt referral to a cardiologist with expertise in valve disease. In the absence of severe disease, medical management and periodic surveillance imaging are continued until progressive disease reaches a point that prompts referral to a valve expert.
The PCP continues to have a central role in patient care when referral to a primary or comprehensive valve center is needed. As the provider with often the most longitudinal relationship with each individual patient, the PCP or referring cardiologist’s role is vital in discussing the patient’s goals of care and facilitating an informed discussion of the net benefit from evaluation and treatment in the context of the patient’s other cardiac and noncardiac conditions. A system that promotes bidirectional communication between the referral center and the referring provider also promotes seamless transitions of care from the diagnosing provider, to the evaluating valve expert, to the interventionalist or surgeon correcting the lesion, and back to the referring provider for ongoing, longitudinal care.
The American College of Cardiology/American Heart Association (ACC/AHA) recommends a systematic approach to management of patients with AS based on the concept of levels of subspecialty care stratified by disease state and patient complexity. Although the specific terms used to define these valve centers will vary from country to country, the basic concepts are widely applicable. Briefly, a comprehensive valve center (CVC) is defined as an organization with the resources, facilities, and training to provide high-quality, advanced care for more complex patients with AS—for example, patients requiring nonfemoral access routes for TAVI, valve-in-valve procedures, surgical aortic root procedures, and so on. CVCs benefit from an expert multidisciplinary team (MDT) that provides access to all percutaneous and surgical approaches currently available, supported by advanced imaging specialists who participate in treatment decision, procedure planning, and periprocedure guidance. By comparison, a primary valve center has expertise in the management of less complex patients and more routine treatment modalities—typically transfemoral TAVI or surgical aortic valve replacement (SAVR) without associated aortopathy. To that end, dedicated imaging specialists with expertise in echocardiography and preprocedural computed tomography (CT) are important members of the MDT, though they may not offer advanced, multimodality, or procedural imaging. The MDT team at both types of valve centers also includes specialists in cardiac anesthesia, vascular surgery, neurology, and palliative care.
A valve program coordinator is essential to manage each patients’ assessment pathway, lead communication with the patient and family, conduct early discharge planning, and help meet the goals of comprehensive programmatic care in all TAVI programs. Registered nurses with expertise in cardiovascular care and program leadership are ideally suited to fulfill this role. The primary responsibilities of the coordinator include (1) triage and coordination (e.g., primary point of contact, clinical triage, coordination of diagnostic assessment), (2) clinical assessment (e.g., assessment of functional status and frailty), (3) patient and family education (e.g., initiation of shared decision-making, tailored approach to individual needs, discharge planning), and (4) program leadership (development of standardized protocols, collaboration with MDT, communication across areas of care). The coordinator plays a pivotal role in facilitating and supporting effective MDT meetings to determine treatment decision and conduct early procedure planning.
Table 2.1 illustrates the similarities and differences between a primary and comprehensive valve center. In summary, each is defined by three key elements: types of procedures performed, MDT team members, and the institutional needs and infrastructure required to maintain the center.
| Comprehensive (Level I) Valve Center | Primary (Level II) Valve Center |
|---|---|
| Interventional Procedures a | |
| TAVI–transfemoral | TAVI–transfemoral |
| Percutaneous aortic valve balloon dilation | Percutaneous aortic valve balloon dilation |
| TAVI–alternative access, including transthoracic (transaortic, transapical) and extrathoracic (e.g., subclavian, carotid, caval) approaches | |
| Valve-in-valve procedures | |
| Transcatheter edge-to-edge mitral valve repair | |
| Paravalvular leak closure | |
| Percutaneous mitral balloon commissurotomy | |
| Surgical Procedures a | |
| SAVR | SAVR |
| Valve-sparing aortic root procedures | |
| Aortic root procedures for aneurysmal disease | |
| Concomitant septal myectomy with AVR | |
| Root enlargement with AVR | |
| Mitral repair for primary MR | Mitral repair for posterior leaflet primary MR b |
| Mitral valve replacement c | Mitral valve replacement c |
| Multivalve operations | |
| Reoperative valve surgery | |
| Isolated or concomitant tricuspid valve repair or replacement | Concomitant tricuspid valve repair or replacement with mitral surgery |
| Imaging Personnel | |
| Echocardiographer with expertise in valve disease and transcatheter and surgical interventions | Echocardiographer with expertise in valve disease and transcatheter and surgical interventions |
| Expertise in CT with application to valve assessment and procedural planning | Expertise in CT with application to valve assessment and procedural planning |
| Interventional echocardiographer to provide imaging guidance for transcatheter and intraoperative procedures (52) | |
| Expertise in cardiac MRI with application to assessment of VHD | |
| Criteria for Imaging Personnel | |
| A formalized role/position for a “valve echocardiographer” who performs both the pre- and postprocedural assessment of valve disease | A formalized role/position for a “valve echocardiographer” who performs both the pre- and postprocedural assessment of valve disease |
| A formalized role/position for the expert in CT who oversees the preprocedural assessment of patients with valve disease | A formalized role/position for the expert in CT who oversees the preprocedural assessment of patients with valve disease |
| A formalized role/position for an interventional echocardiographer | |
| Institutional Facilities and Infrastructure | |
| Multidisciplinary team | Multidisciplinary team |
| A formalized role/position for a dedicated valve coordinator who organizes care across the continuum and system of care | A formalized role/position for a dedicated valve coordinator who organizes care across the continuum and system of care |
| Cardiac anesthesia support | Cardiac anesthesia support |
| Palliative care team | Palliative care team |
| Vascular surgery support | Vascular surgery support |
| Neurology stroke team | Neurology stroke team |
| Consultative services with other cardiovascular subspecialties (see Section 5.2.4 Personnel, Institutional Facilities, and Infrastructure) | |
| Consultative services with other medical and surgical subspecialties (see Section 5.2.4 Personnel, Institutional Facilities, and Infrastructure) | |
| Echocardiography–3D TEE; comprehensive TTE for assessment of valve disease | Echocardiography–comprehensive TTE for assessment of valve disease |
| Cardiac CT | Cardiac CT |
| ICU | ICU |
| Temporary mechanical support (including percutaneous support devices such as intra-aortic balloon counterpulsation, temporary percutaneous ventricular assist device, or ECMO) | Temporary mechanical support (including percutaneous support devices such as intra-aortic balloon counterpulsation, temporary percutaneous ventricular assist device, or ECMO) |
| Left/right ventricular assist device capabilities (on-site or at an affiliated institution) | |
| Cardiac catheterization laboratory, hybrid catheterization laboratory, or hybrid OR laboratory d | Cardiac catheterization laboratory |
| PPM and ICD implantation | PPM and ICD implantation |
| Criteria for Institutional Facilities and Infrastructure | |
| IAC echocardiography laboratory accreditation | IAC echocardiography laboratory accreditation |
| 24/7 intensivist coverage for ICU |
a A Primary (Level II) Center may provide additional procedures traditionally offered at a Comprehensive (Level I) Center as long as the criteria for competence and outcomes are met.
b If intraoperative imaging and surgical expertise exist.
c If mitral valve anatomy is not suitable for valve repair.
d Equipped with a fixed radiographic imaging system and flat-panel fluoroscopy, offering catheterization laboratory-quality imaging and hemodynamic capability.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here