Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Strabismus related to ocular torsion.
A- and V-pattern deviations.
Oblique muscle overactions and underactions.
Torsion of the globe.
“Oblique muscle overaction” and A- or V-pattern strabismus are defined based on clinical exam findings. Oblique overaction and pattern strabismus usually are intimately related in well-defined ways. It helps to clarify what these terms mean.
Every ophthalmology resident learns the function of the extraocular muscles based on their direction of “primary field of action” in the six cardinal positions of gaze. The medial rectus moves the eye into adduction when it contracts; the lateral rectus abducts the eye. In turn, the oblique muscles are said to have their greatest or most pure action when the eye is adducted, so the inferior oblique elevates the eye in adduction, whereas the superior oblique depresses the eye in adduction. Thus it seems natural that an excessive elevation of the eye in adduction is called inferior oblique overaction (IO OA), whereas an excessive depression of the eye in adduction is called superior oblique overaction (SO OA). But these labels are deceptive.
The term oblique overaction implies hypertonicity or excess neural stimulation; however, this appearance does not necessarily mean the oblique muscles are truly overacting. Instead, the term oblique overaction is used because the oblique muscles have their greatest vertical action when the eye is adducted, where the hypertropia is seen clinically.
A or V patterns can be defined by the measured difference in horizontal deviation in up gaze compared with down gaze, where the patient is fixing on an accommodative distance target and the vertical gaze angle is about 30° from primary:
A pattern—at least 10 prism diopter (PD) lesser exodeviation or greater esodeviation in up gaze than down gaze ( Fig. 11.8.1 )
V pattern—at least 15 PD greater exodeviation or lesser esodeviation in up gaze than down gaze ( Fig. 11.8.2 )
Precise head positioning when measuring deviation in side gaze or up or down gaze is difficult, especially in children. Thus the incomitant deviation in up and down gaze may vary inadvertently, depending on the variable direction of gaze. Because of this, many clinicians simply label A and V patterns as mild, moderate, or large.
A common system for grading “oblique overaction” is 0 (normal) to 4+ (extreme). In rare cases when the misalignment appears to exceed even 4+ as a result of aberrant orbital anatomy (some types of syndromic torsion), 5+ has been used as well. In turn, restriction of elevation (as can be seen in a patient with Brown syndrome) can vary from 1– to 4–. In addition, and in concert with the dysinnervation of Duane syndrome, the terms upshoot and downshoot reflect hyperelevation or hyperdepression in adduction not typically resulting from oblique muscle function.
Common childhood strabismus occurs when fusion is lost or is overcome by the imbalance between agonists and antagonists (e.g., intermittent exotropia). Much childhood strabismus can best be understood by considering the five elements that determine the typically progressive misalignments that occur: the three axes of strabismus, the inherent bias between agonist and antagonist pairs, muscle-length adaptation, motor fusion, and the restraint put on the path of extraocular muscles by orbital tissues.
Strabismus occurs when fusion is absent, is lost, or is overcome by the imbalance between agonists and antagonists mechanically, with or without neurological origin. Regardless of the etiology, torsional misalignment may play a major role, often giving a clue to the etiology and directing the best intervention. In a patient with the potential for binocular fusion, addressing the torsional component of strabismus may be critical for maintaining fusion over time.
In addition, strabismus occurs in many forms, including types with distinctive genetic fingerprints, such as congenital cranial dysinnervation disorders like Duane syndrome, Moebius syndrome, congenital fibrosis of the extraocular muscles (CFEOM), and Brown syndrome. Other causes of misalignment include trauma; inflammation from Graves’ or orbital pseudotumor; and neurological conditions, including myasthenia gravis and cranial nerve palsies.
To understand torsional strabismus, it is important to understand the three axes of ocular motion. Each globe has three rotational degrees of freedom, and thus the rotations of the eye fall into three orthogonal (perpendicular to each other) axes: horizontal, vertical, and torsional. These axes also have been described in analogy with the motions of an airplane, as yaw (horizontal), pitch (vertical), and roll (torsional), as emphasized by Dr. Michael Brodsky. Horizontal misalignment is seen as esotropia (ET) or exotropia (XT), whereas vertical misalignment is seen as hypertropia, with one eye being higher than the other in the primary position. However, torsional misalignment is invisible to the clinician when the eyes are in the primary position: detection of torsional misalignment depends on observing the relatively skewed ocular deviations in various gaze directions (e.g., hypertropia of the adducting eye in the presence of excyclotorsion) or on fundoscopy by noting the incyclo- or excyclorotated fundus appearance. Because the muscle insertions are torted along with the rest of the globe, the direction of motion of the eye in attempted versions induces the appearance of oblique overaction. Thus incyclotorsional misalignment is often attributed to SO OA, whereas excyclotorsion is often attributed to IO OA. These are so named because these vertical deviations in adduction correspond to the “primary fields of action” of the respective oblique muscles. How this occurs will be described in detail later in this chapter.
The actions of the extraocular muscles (EOMs) are not all cleanly separated along the three orthogonal axes. The horizontal recti are pure in their direction of action: even in eccentric gaze their muscle paths are constrained by the tissues of the orbit. However, the vertical recti pull on the globe at a small angle. Because the vertical recti originate on the nasally displaced orbital apex, the superior rectus is responsible for modest intorsional effect and the inferior rectus is responsible for a modest extorsional effect. As a result, a tight vertical rectus muscle sometimes can result in symptomatic torsional diplopia; for example, this can be seen after vertical rectus resections, or it may be secondary to local toxicity from bupivacaine injection or inflammatory hypertrophy from thyroid eye disease.
In turn, the oblique muscles’ main action in the primary position is torsion. However, because they insert on the globe at an angle approximately 39 degrees from that required to be purely torsional in their effect, they have small secondary and tertiary actions of vertical pull and adduction. As a result of its particularly wide insertion, which extends from the anterior toward the posterior surface of the globe, superior oblique function is particularly dependent on ocular position. In addition, the passive actions of orbital tissue (including the elasticity of the extraocular muscles themselves or of the optic nerve) have significant effects on the ocular position in eccentric gaze, limiting how far the globe can rotate.
The orbital path of each of the muscles is constrained by several tissues of the orbit. As the rectus muscles go anteriorly from the annulus of Zinn to their insertion, they pass through orbital fat and connective tissue septae. Because the origin of the recti is fixed to bone posteriorly, there is more laxity in this constraint from the anterior connective tissue than from the posterior tissue. Just posterior to the equator of the globe, and as described in 1805 by Jacques Tenon, the rectus muscles pass through inelastic but somewhat lax pulleys of connective tissue at the point where they enter the slick bursa of Tenon’s capsule. These pulleys are adherent to the muscle but allow the muscle to extend and contract within limits; the pulleys are, in this manner, unlike the pulley of the superior oblique tendon. Whether the bellies of the muscles are constrained by orbital fat and septae or by the pulleys themselves, this passage through the pulleys marks an effective point of origin for the action of each muscle. The line from the effective point of origin to the insertion on the globe determines the direction of force on the globe. The pulleys are connected in an array that encircles the globe and is actively shifted by the orbital layers of the EOMs and by smooth muscle. This connective tissue sling, including the pulleys, also is connected to the orbital wall. It has been demonstrated that rectus muscle transposition procedures have little impact on rectus trajectory behind the globe because of the stabilizing effect of the orbital connective tissues. Thus the very presence of this orbital and pulley connective tissue modulates the impact of transposition procedures and likely explains why such procedures leave the original primary function of the transposed muscles reasonably intact.
For most patients with the appearance of IO OA, SO OA, or A- or V- patterns, torsion is a key to understanding clinical observations. However, pathology in any of these components, including neural control, the muscles, the soft tissues, and the pulley arrays—and in some cases, even the bony orbital anatomy—can produce strabismus, including pattern strabismus and oblique overaction. Recent work may have identified neurally separate compartments of some of the extraocular muscles, which may play a role in some patients.
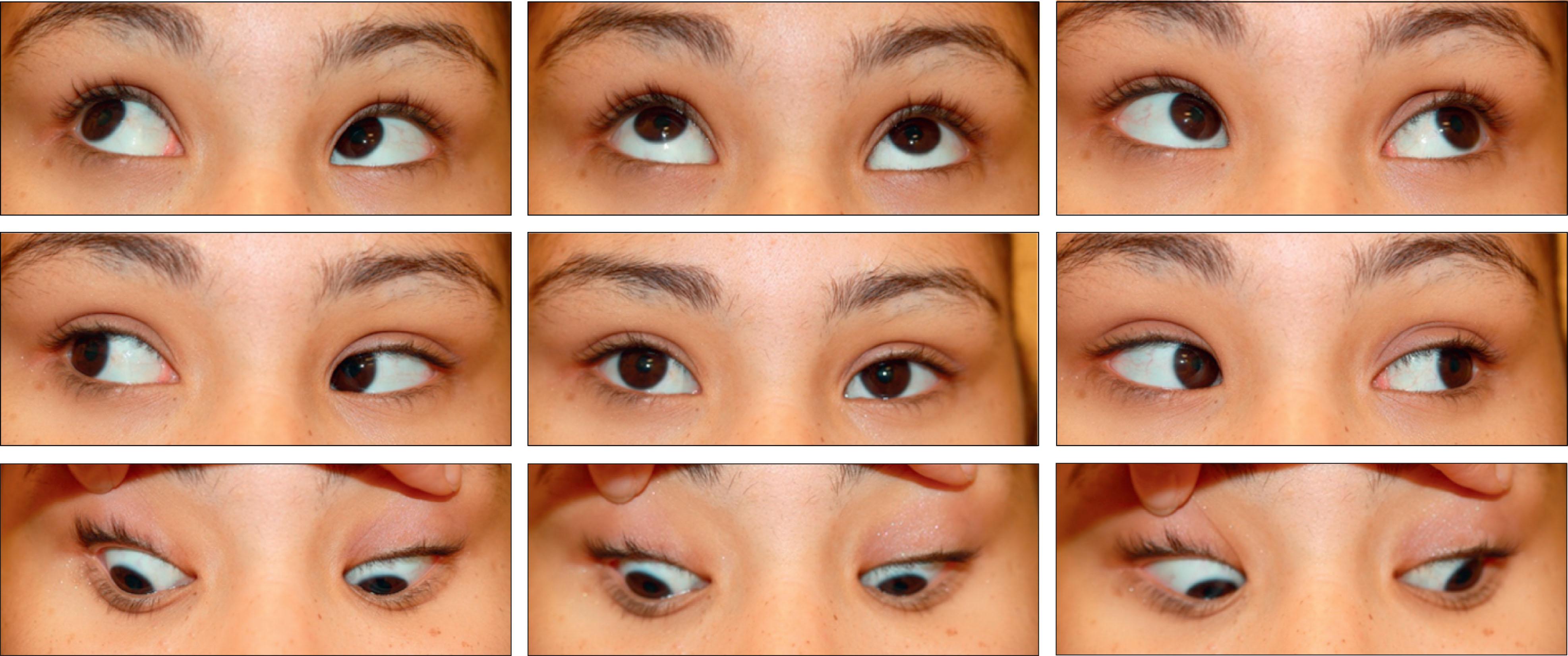
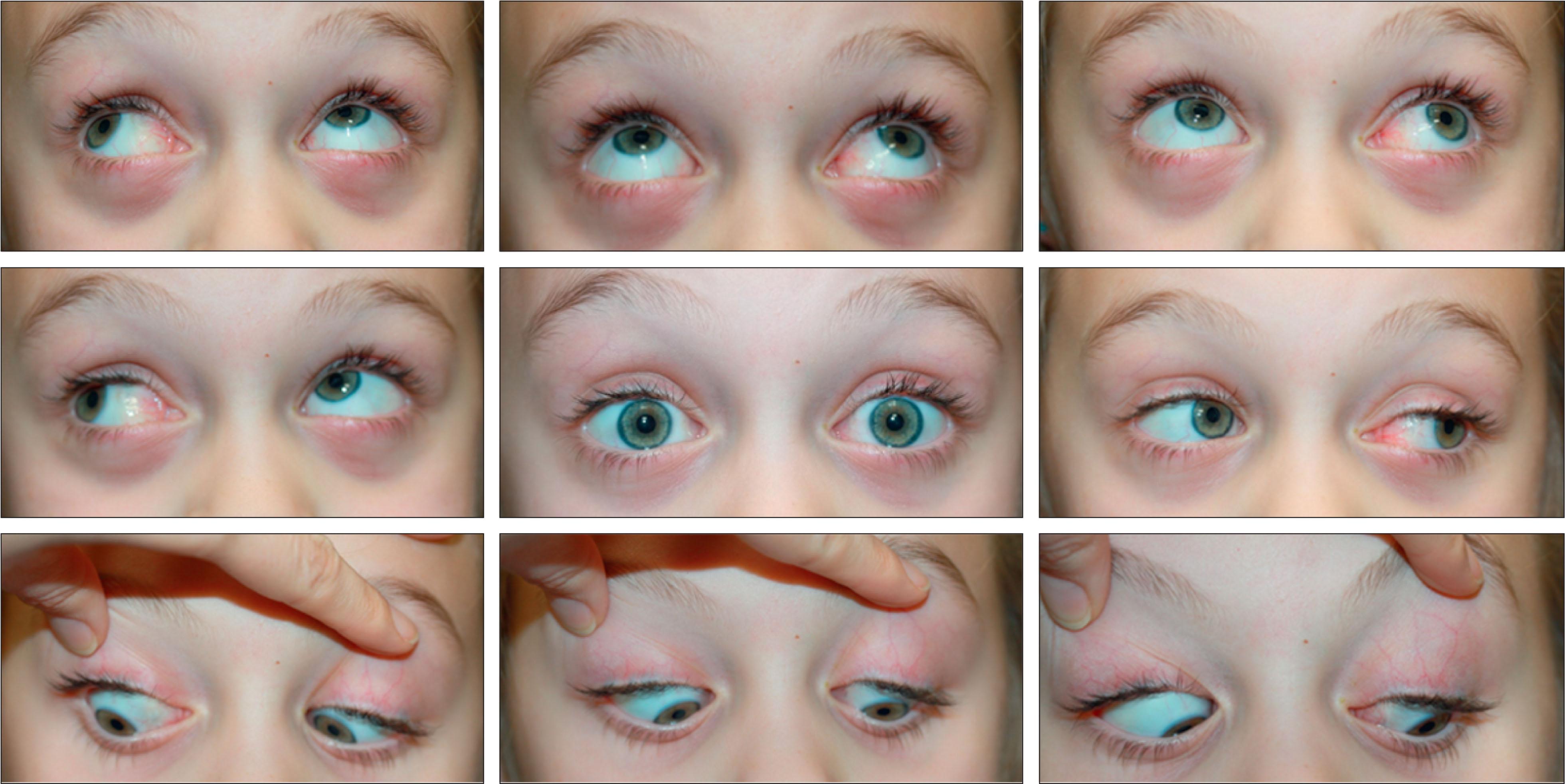
As an example of “primary overaction of the inferior obliques,” let us consider the common story of a 2-year-old child with a cycloplegic refractive error of +4.5 D OU, who presents with accommodative esotropia. The initial examination shows no oblique overaction, pattern strabismus, or fundus torsion, and when given a prescription for +4.5 D lenses, the spectacles fully correct his deviation. The child then is lost to follow-up, and over 2 years, he fails to wear the glasses. He presents again at age 4 with partially accommodative esotropia: when given glasses to correct his full cycloplegic refraction, his esotropia (ET) cc = 25 prism diopters (PD). He also has 3+ IO OU, a moderate V pattern, and approximately 15 degrees of excyclotorsion in both eyes ( Fig. 11.8.3 ). Because no apparent cause exists for the IO OA, such as cranial nerve IV palsy or craniosynostosis, his strabismus is called V-pattern esotropia with “primary inferior oblique overaction.” Surgery is performed: a recession of the medial rectus (MR) 5.0 mm OU and a recession of the IO 14 mm OU. At his 2-month postoperative exam, he is straight in all positions of gaze, with no IO OA, no V pattern, and no torsion on fundus exam.
Why did this patient develop a V pattern with apparent IO OA, and how did recession of the IO correct both conditions?
Many causes occur for “oblique overactions” and pattern strabismus. In this chapter, we show how ocular torsion and torsional displacement (also called heterotopy ) of the muscles and orbital tissues are the keys to understanding many patients with oblique muscle dysfunctions and V- and A- pattern strabismus. We discuss clinical observations, the place of torsion within the three axes of strabismus, how torsion of the rectus pathways results in pattern strabismus, and the appearance of oblique overaction. We will discuss how lack of fusion can lead to torsional strabismus, as well as other causes of oblique dysfunction.
Oblique overactions and A and V patterns rarely are observed clinically in infants with esotropia, perhaps because of their limited effort or cooperation. It is difficult to get a young child to follow an object into far side gaze or to precisely measure alignment in chin-up or chin-down posture. Many patients either develop or are found to have these signs of torsional strabismus when they are 3–6 years of age rather than in the first year of life, even when torsion is observed objectively on fundus exam.
In a study by Wilson and Parks, IO OA was observed to develop in about 72% of patients with congenital esotropia, 34% of those with accommodative esotropia, and 32% of those with intermittent exotropia who were followed up for longer than 5 years. The incidence of IO OA in patients with congenital esotropia was not related to age at strabismus onset, time from onset to surgery for the esotropia, age at first surgery, or decompensation of horizontal alignment; it was, however, related to the number of surgeries necessary to align the eyes horizontally. The mean age of onset or detection was 3.6 years, with many demonstrating pattern deviation much before.
Eustis and Nussdorf studied infants undergoing bilateral medial rectus muscle recession for esotropia and found that of the eyes with excyclotorsion observed at surgery, all demonstrated IO OA at follow-up. Of those with no torsion at the time of surgery, only 9 of 21 demonstrated IO OA at follow-up.
In children with SO OA, there is a higher rate of concurrent neurological disease, up to 40% in one series.
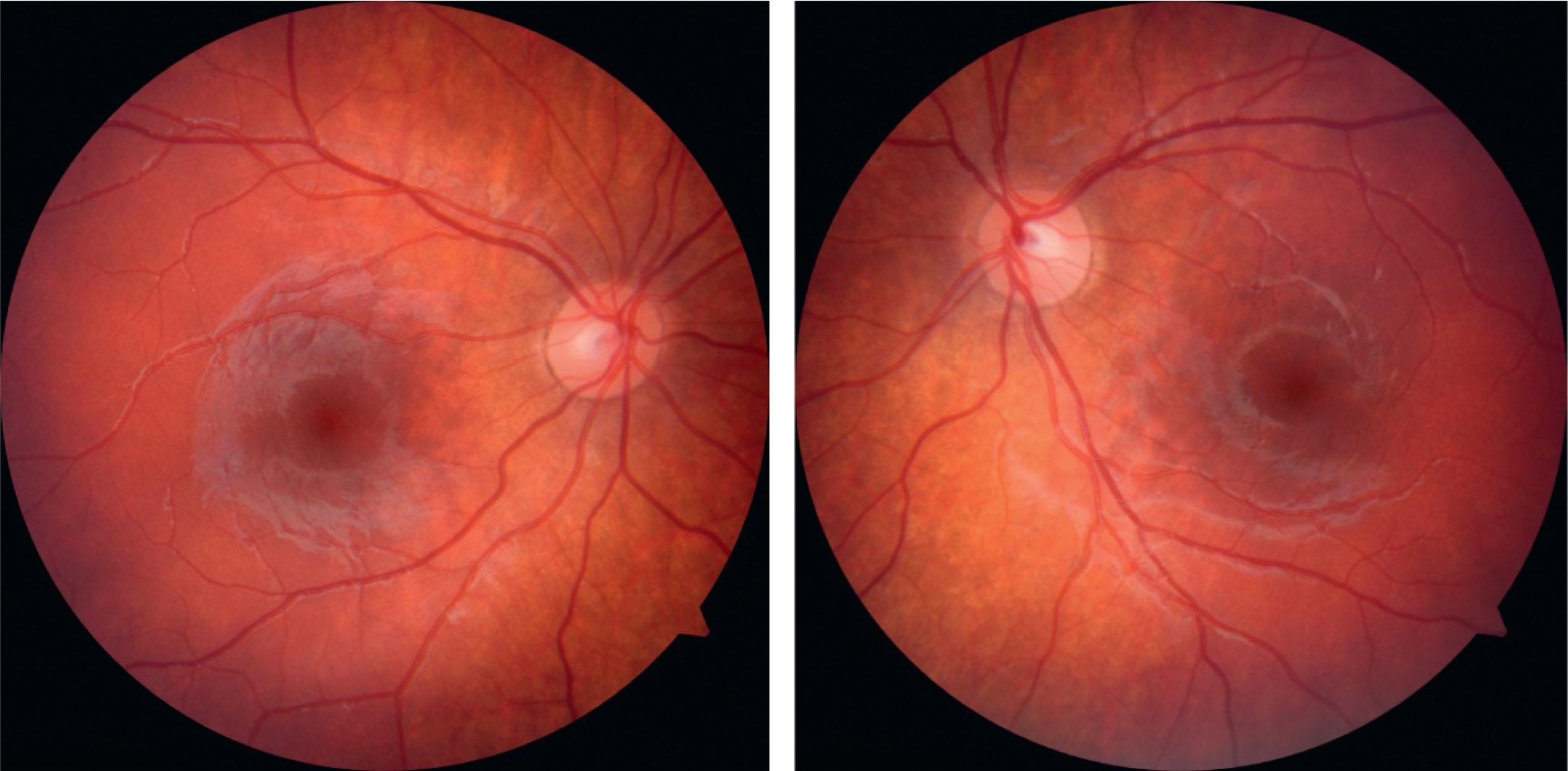
Clinical fundoscopy can be used to estimate the degree of fundus torsion, based on a 1+ to 4+ scale, a protractor, or estimation of the angle, as is done for free-lens retinoscopy refractions. Torsion also can be documented by fundus photography in cooperative patients ( Fig. 11.8.4 ) or during surgery.
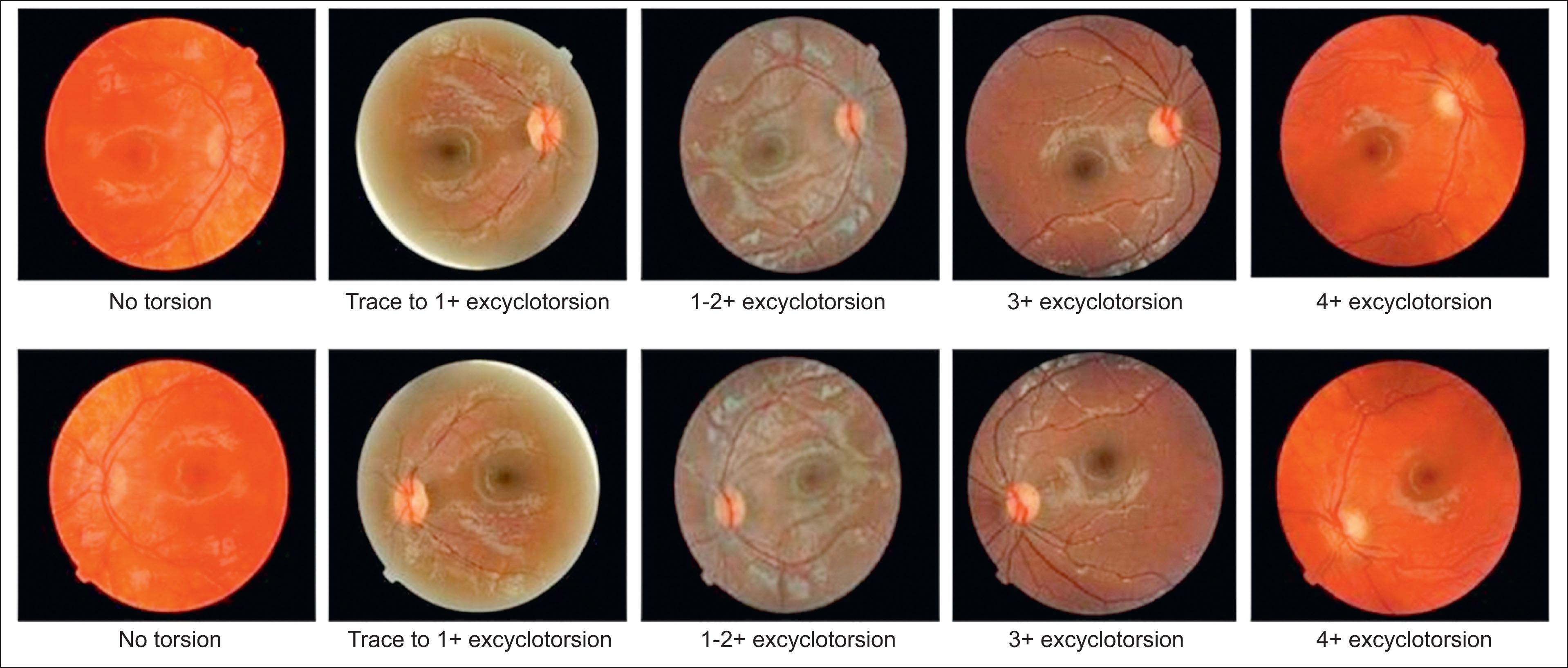
Clinically significant fundus torsion can vary from 10° to 20°. In general, 10° of bilateral fundus excyclotorsion corresponds to 2+ IO OU and a moderate V pattern; 20° of excyclotorsion corresponds to 4+ IO OU and a large V pattern. The same is true for incyclotorsion: 10° of bilateral fundus incyclotorsion corresponds to 2+ superior oblique both eyes (SO OU) and a moderate A pattern; 20° of incyclotorsion corresponds to 4+ IO OU and a large A pattern. With large angles of torsion, the eyes also appear to have UA of the antagonist of the “overacting” oblique: thus a child with 20° of excyclotorsion may appear to have a 2– SO OU as well as 4+ IO. Except for children with craniosynostosis, it is uncommon to observe ocular torsion of greater than 25°. Of note, some children with craniosynostosis can have substantially larger torsion, partly a result of excyclorotation that begins at the origins of the rectus muscles near the orbital apex. The authors have seen up to 40° of excyclotorsion in both eyes in this setting.
In eyes with ocular torsion, the relative position of the nerve and macula are rotated. The visual fields in such eyes show displacement of the blind spot, with the blind spot below the horizontal meridian in excyclotorsion and above it in incyclotorsion. This displacement of the blind spot also can be found with careful confrontation visual fields.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here