Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The first report on a toe-to-hand transfer ever done to a human goes back in time to the 19th century when Nicoladoni described staged, pedicled toe-to-hand transfer over a 4-week period. Davis was the first to combine staged transfer with microsurgical anastomosis of the dorsalis pedis artery; however, the credit for the first, one-stage toe transplantation to the thumb actually goes to Yang, who transplanted the second toe in 1966. Cobbett, on the other hand, transferred the great toe to the thumb for the first time in 1968. After that, many clinical reports using various forms of toe transfer ensued during the 1970s and 1980s reflecting the intimate relationship between toe transfer and advances in microsurgery. Nowadays, toe transplantation is the only safe and reliable procedure that replaces “like with like” in cases of missing or lost thumb and/or fingers.
For thumb reconstruction, either functional or esthetic, toe transfer is a widely accepted option; in contrast, for finger reconstruction, toe transplantation has been somewhat controversial. It is getting more acceptance now because patients have become better informed and more demanding, and colleagues have accumulated additional experience. , , Not surprisingly, digital and thumb amputations have a profound impact on quality of life, psychosocial functioning, and the ability of the patient to return to work. , Such an impact is expected to have a debilitating effect when mutilating injuries involve multiple digits. Therefore “like-with-like” reconstruction using the feet as donor sites offers a good alternative to restore function and appearance after digital amputations.
In comparison to the results obtained with prostheses or some conventional techniques, microsurgical toe transfer is the only procedure that provides functioning digits with sensitivity , , ; in contrast to hand transplantation, toe transfer does not involve lifelong immunosuppressant administration. Plus, satisfactory hand function and patients’ approval are still achievable. Reports on the use of toe transplantation for finger replacement include multiple-digit reconstruction with bilateral toe transplantation, , , combined transplantation of the second and third toes, combined transplantation of the third and fourth toes, , single transplantation of the third toe, , and other toe combinations transplanted as one unit.
Microsurgical restoration of distal digit function with partial toe transfer was first suggested in 1979 by Buncke and Rose, who used pulp neurosensory free flaps for finger reconstruction. During the past 10 years, more attention has been focused on this complex anatomic region, and various surgical procedures have been described and refined for distal digit reconstruction, including vascularized nail grafts, toe hemipulp free flaps, lesser toe wraparound procedures, and partial transplantation of a lesser toe or a great toe. This brief review leaves no doubt that microsurgical toe transplantation has revolutionized hand reconstruction and that its role will continue to expand.
This chapter focuses on toe-to-finger reconstruction but also covers many aspects of thumb reconstruction and some topics about congenital hand reconstruction.
Although technically feasible, not every patient who experiences digit amputation is a candidate for microsurgical toe-to-hand transplantation. In selecting the right patient for this type of surgery, a multifactorial assessment, which has to be thorough and complete, should be conducted focusing on amputation level, number of digits involved, patient’s age and parents’ motivation (in the pediatric population), and patient’s needs and motivations (in the adult population). For instance, a distal amputation of one digit might be psychologically more important and meaningful to one patient than a metacarpal hand deformity is to another, even though a higher functional deficit is present in the latter patient. Moreover, although it may seem counterintuitive, a single-finger amputation distal to the proximal interphalangeal (PIP) joint constitutes one of the best indications for toe transfer because of the excellent functional results that can be achieved, whereas a single-finger amputation proximal to this joint is probably best addressed with ray amputation. The patient’s overall general health, medical problems, and associated injuries should be considered as well.
Age deserves special discussion; although advanced age is not an absolute contraindication to toe transplantation, functional requirements in the hand are lower in elderly patients. Furthermore, a higher risk of medical complications and less sensory recovery can be expected at an advanced age. In contrast to elderly patients, infants appear to benefit significantly from toe transplantation, as remarkable gains in function, sensation, and ability to perform daily activities with high psychological satisfaction of the growing children and their parents are achievable , ; however, performing toe-to-hand transplantation in children younger than 2 years can be technically challenging. Occupation, hand dominance, and activity levels are all important factors for adults. Surgical indications may also differ from country to country, based on the level of workers’ compensation coverage, job opportunities, and cultural demands.
The location and number of missing digits are important for establishing reconstructive priorities. Radial pulp defects in the index and middle finger and the ulnar aspect of the thumb are more important for fine pinch and the handling of small objects. With multiple-digit amputation, reconstruction should encompass at least two adjacent fingers to enhance stability and strength and to provide tripod pinch to ensure that the thumb is functional. The radial digits (index and middle) are more important for patients with occupations that require fine manipulation, whereas the ulnar digits (ring and middle) are more necessary for work that requires a powerful grasp. ,
When toe-to-hand transplantation is being considered as a reconstructive option, donor site morbidity should be extensively discussed with the patient and relatives. Although foot function for most ambulatory activities is not restricted after the resection of one or two toes, it might be limited to some degree for specific activities (e.g., certain sports). Moreover, when both feet are used for transfer, the dominant foot, which generally is the right, should be given preference in terms of the least donor site morbidity. For instance, if a great toe and combined second and third toes are considered, the right foot is chosen to be the donor for combined second and third toes given the fact that donor site deficit will be less than that following the loss of the hallux. Foot cosmesis should not be overlooked and can be important in some cultures and in young patients. Finally, for surgeons involved in hand reconstruction, experience and familiarity with the various toe transplantation techniques are a must in order to avoid failures and complications and to offer their patients the optimal result.
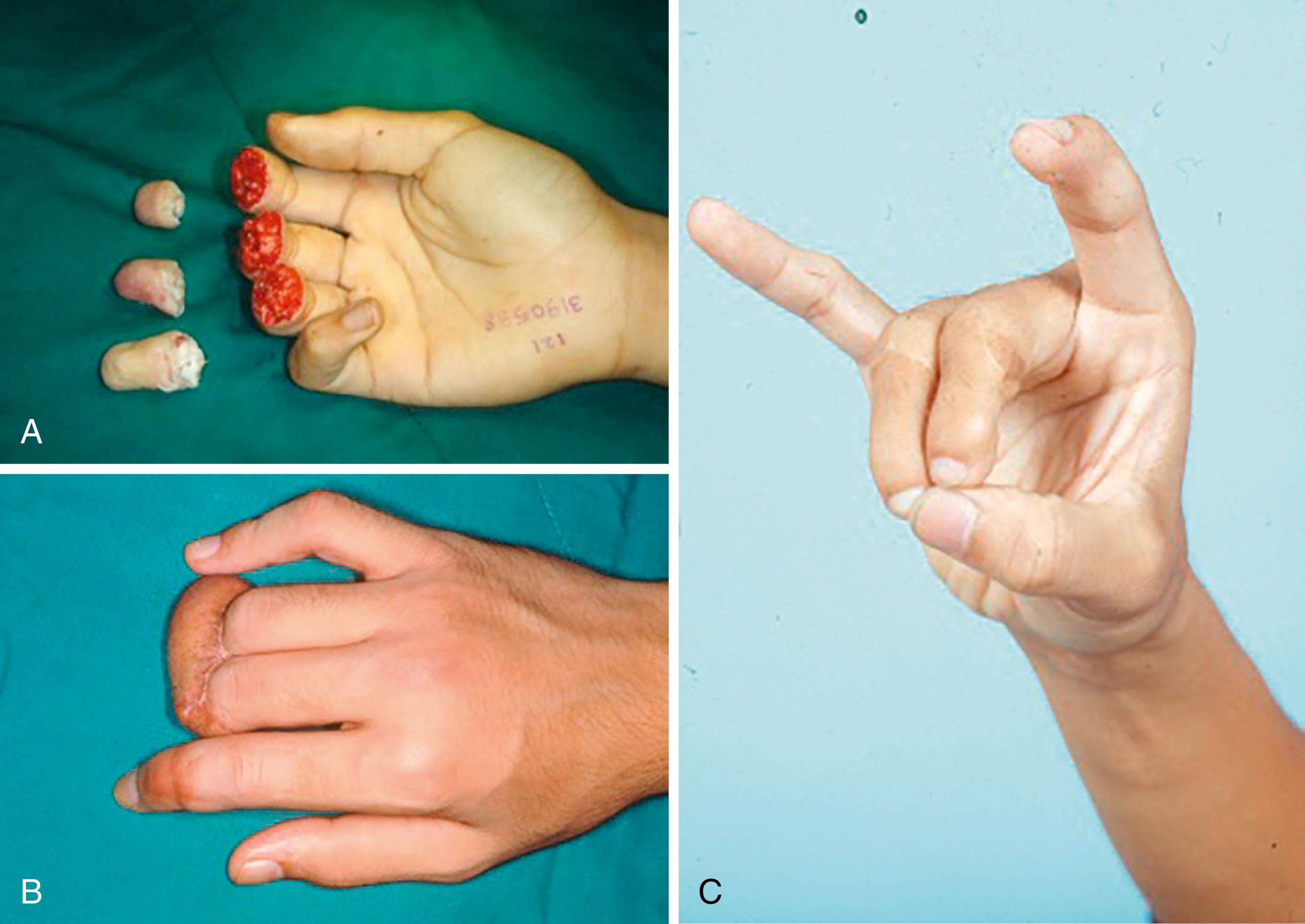
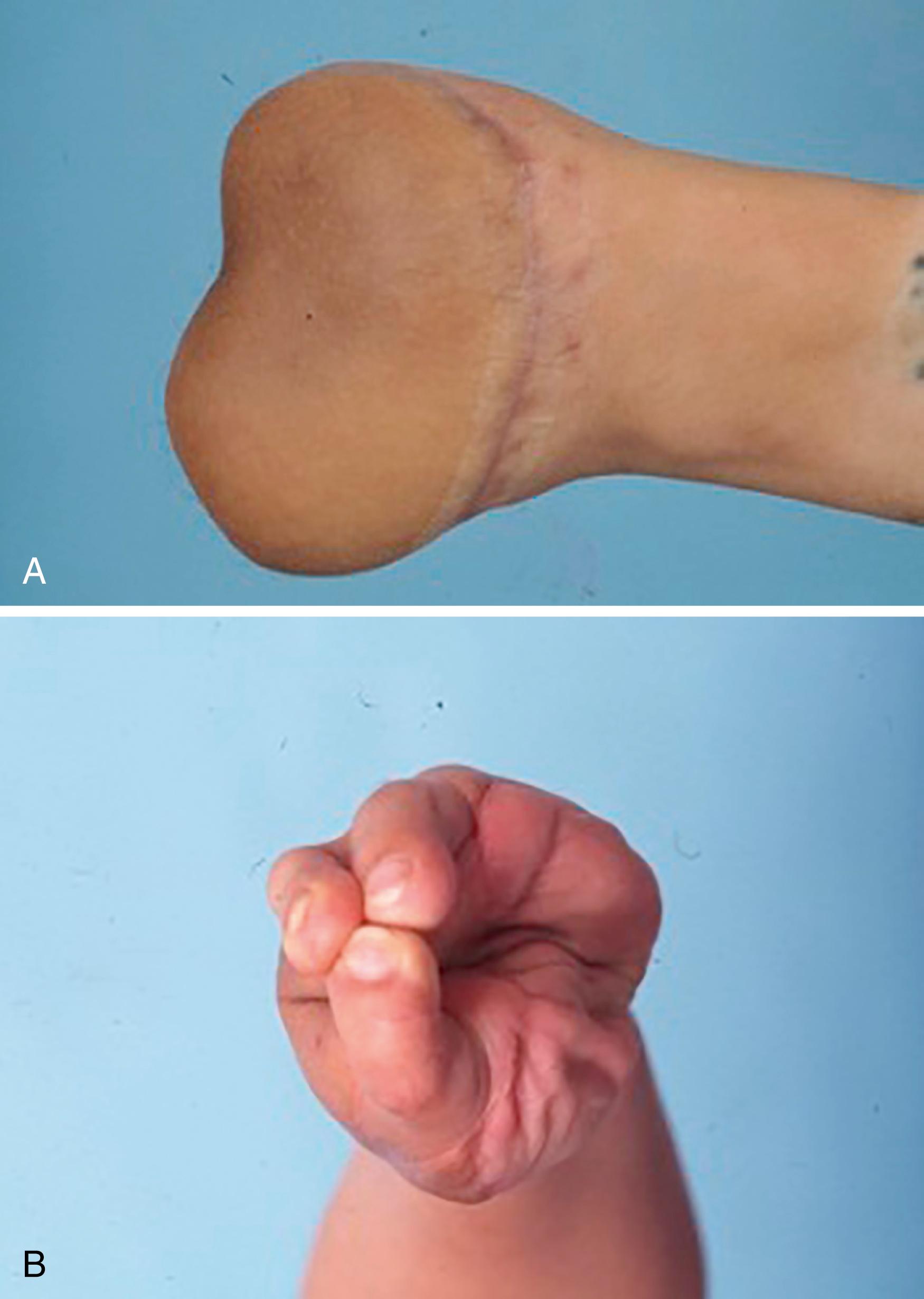
Digit replantation, including use of the distal parts, remains the best option for the management of acute traumatic amputations. This is a reliable procedure that should be attempted whenever indicated and possible. , Toe transplantation for digit reconstruction must be considered from the time of initial injury; however, and when practical, it should be discussed with the patient and relatives as an option for future reconstruction, even before replantation. This is particularly true for patients with multiple-digit amputations and when conditions for replantation are not ideal (e.g., severe crushing or avulsion injuries). If replantation fails or is not feasible, toe transplantation for reconstruction should be planned during the initial care period. Bone, tendon, and neurovascular bundle length must be preserved after debridement of all nonviable tissue and provision of adequate soft tissue coverage ( Fig. 47.1 ). , The length of all anatomic structures retained in the stump is likely to determine the type of toe transplantation and its functional and esthetic outcome. Moreover, preservation of stump length reduces the likelihood of requiring nerve or tendon grafts, and vein grafts for vascular anastomoses, during finger reconstruction, thus avoiding extensive dissection in the donor foot.
It is a common mistake to excessively shorten the digital skeleton to achieve direct or primary closure of the wound with local flaps. For skeletal fixation with toe-to-hand transplantation, bone stumps as short as 5 mm can be used for intraosseous wiring. It is therefore recommended that bone length be preserved to the extent that complete soft tissue coverage is still possible. Every effort should be made to maintain functioning joints or the cartilage surface with the articular capsule. The transferred toe can be harvested through disarticulation, and the joint capsule can be directly repaired with the recipient finger to achieve good functional results, particularly in thumb reconstruction. Metacarpal stumps can be augmented to the desired length with a nonvascularized bone block, thus avoiding proximal transmetatarsal osteotomies during toe transfer and preserving metatarsal length, which minimizes donor foot morbidity.
Preservation of the extensor mechanism in the finger is important for maintenance of balance between the intrinsic and extrinsic systems involved in extension. For distal amputations, the extensor apparatus should be left in situ on the digital stump, and the intrinsic insertions on the proximal phalanx should be preserved. For more proximal amputations at the metacarpophalangeal (MCP) joint level, retention of the extensor hood is necessary for the same reason. , Conservative debridement of flexor tendon length is important in distal digit amputations because functional results are better when the insertion of the flexor digitorum superficialis (FDS) is present. For more proximal amputations, the finger flexors must be left in situ, although they might be shortened for future tendon repair in zone 3. By preserving the flexor tendons in place, it is possible to maintain the integrity of and space within the pulley system, which is vital for future function, especially the A2 and A4 pulleys.
The digital arteries and veins are seldom intact after crushing or avulsion injuries. Every effort should be made to retain the arteries’ length in nonreplantable digit amputations because these can be used as recipient vessels for toe transplantation in the future. The ulnar digital artery in particular is larger than its counterpart in the radial side of the fingers. The veins are less of a concern, given that a rich venous network on the dorsum of the hand is usually present.
To prevent the development of neuromas in amputation stumps, proximal resection of the digital nerves has been advocated. When toe-to-hand transplantation is considered for future reconstruction, however, the nerves’ length must be preserved because recovery of sensation is faster when neurorrhaphies are performed closer to the transferred toe.
Instead of using local or regional flaps to cover the wound, soft tissue augmentation with a pedicle groin flap is a better alternative. The use of local flaps may increase morbidity, create additional deformity, and impede functional rehabilitation. The redundant skin provided by a groin flap may later prove useful for covering the transferred toe (see Fig. 47.1C ). It can also be used to protect the pedicle, create an adequate web space, and decrease scarring. Moreover, when there is enough skin available on the recipient finger (or hand), it is possible to minimize the amount of skin included during toe transfer, thus facilitating primary closure of the foot incision and enhancing donor site appearance.
In some circumstances it may be possible to overcome hand skin deficiency in a single stage if additional tissue is taken from the foot along with the toe. Although readily available, the dorsalis pedis fasciocutaneous flap is not recommended because of donor site morbidity; however, a fasciosubcutaneous flap (excluding skin) based on the dorsalis pedis or metatarsal arteries, followed by a skin graft, has been reported to lead to good success.
Toe-to-hand transplantation can be performed either primarily or secondarily. Primary reconstruction refers to transfer in the setting of an open wound. Secondary reconstruction refers to transfer after definitive wound closure is achieved. Acute, subacute, and chronic are confusing terms and of no clinical relevance to toe-to-hand surgery. It is important, however, to emphasize that in primary transfer, adequate debridement should be achieved and associated injuries should be managed before toe-to-hand transplantation is performed. Moreover, primary toe-to-hand transfer may not be suitable for nonreplantable finger amputations in children due to the potential risk of loss of the transferred toe; however, further studies are needed. Nevertheless, parents should be made aware of such a possibility, and stump closure should not compromise future toe-to-hand transfer.
From the standpoint of functional outcome, primary transfer may be more beneficial compared with secondary transfer. A retrospective study of 31 primary and 144 secondary toe-to-hand procedures showed a survival rate of 96.9% in primary and 96.5% in secondary transplants. There was no statistical difference between the two groups in terms of intraoperative anastomotic revision, reexploration, complications, and secondary procedures. Similar results were reported in a study by Woo and associates, who also noted a 30% reduction in convalescent time and a greater likelihood of patients returning to their original jobs after immediate reconstruction. Early transfer may also result in better sensory recovery than delayed transfer.
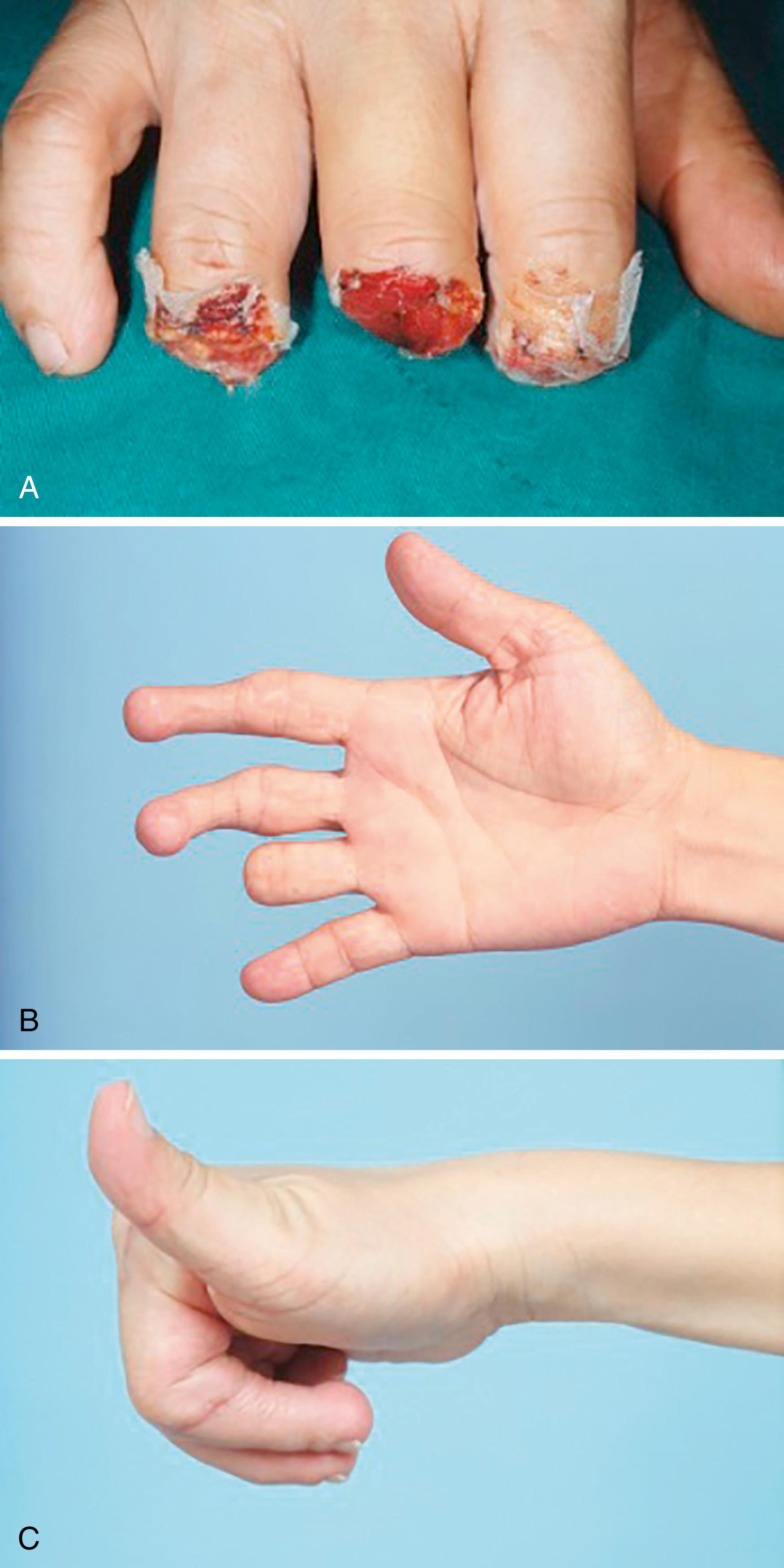
Primary toe-to-hand transplantation can be performed safely for either functional or esthetic restoration whether single or multiple toes are involved. Compared with secondary procedures, it reduces hospital stay and restores hand function and the patient’s body image in less time. In some cases, primary transfer may also be technically easier because dissection of the neurovascular bundles is not impeded by fibrosis or scar adhesion. It is recommended in highly motivated, well-informed patients in good physical condition and when wounds are clearly demarcated and clean ( Fig. 47.2 ). , , It is also recommended in the setting of multiple-extremity injury when spare parts are available. Woo and associates found that patient satisfaction with the esthetic appearance is less in primary versus secondary transfer. Some surgeons therefore recommend delayed transfer in all cases to give the patient time to understand the extent of the hand deficit, appreciate the need for the procedure, and accept the reconstructive limitations and possible donor site morbidity. In our opinion, however, the benefits of immediate transfer far outweigh these considerations.
Although a thumb amputated at the interphalangeal (IP) joint level can still perform its basic functions, fine manipulation ability and hand appearance are compromised. Therefore, when replantation is not possible, toe transplantation should always be offered as a reconstructive option, even at a distal level. The thumb can be reconstructed with either the great toe or a lesser toe. Transfer of the great toe can include the entire toe or modified transfers such as the great toe wraparound flap, trimmed great toe, twisted toe, and many others. The methods of thumb reconstruction should be individualized, taking into consideration the functional and cosmetic needs of the patient as well as donor site morbidity. In general, thumbs reconstructed with the great toe and its variants have a better functional and esthetic result than those reconstructed with lesser toes.
In cases of thumb amputation between the IP joint and metacarpal head, the functional outcome is significantly affected by the level of amputation and thenar musculature status. Amputations proximal to the MCP joint inevitably result in destruction of the thenar musculature and secondary loss of opposition. Opposable tripod pinch is one of the essential goals in toe-to-thumb reconstruction, which is usually achieved by pronation osteosynthesis in the setting of loss of the muscles of opposition. However, Lin and associates recommended primary opponensplasty in toe transfers to provide active restoration of opposition and better restoration of tripod pinch.
In cases of thumb amputation at the metacarpal level, the toe alone is inadequate to restore normal function. Although a larger flap from the foot, which includes the toe and metatarsal bone, is feasible, donor site morbidity can be quite high. Separate thumb ray reconstruction using osteoplastic techniques should be performed first, followed by second-stage toe transfer.
Just as replantation of single-digit amputations has been a matter of debate for many years, single-digit reconstruction with toe transplantation remains controversial. Because the functional deficit in the hand is minimal when only one finger is missing, some authors believe that sacrificing a toe for finger reconstruction (other than the thumb) is not justified, especially in the nondominant hand. , , However, when optimal reconstruction is desired, finger reconstruction with like-tissue transplantation from the foot usually offers satisfactory results, particularly in distal finger amputations. ,
The distal end of a digit is most frequently injured. It is defined as the end portion of the digit distal to the insertion of the flexor pollicis longus in the thumb or the FDS in the finger. , The highest density of innervation in the body surface is contained in the finger pulp; thus it is considered the “end organ of touch.” Specialized components of the distal digit include a sensate glabrous pulp and stable adherent nail. Glabrous skin characteristics allow resistance to wear and tear and provide a nonslippery surface for grasping. Attachment of the pulp skin to the underlying distal phalanx by a network of septa prevents excessive skin gliding and shearing, which is essential for strong pinching. The fatty tissue arrangement between the septa allows the pulp to conform to the shape of objects during pinch and grasp. The nail plays a major role in tactile sensibility of the pulp and in tip pinch, and it is an important esthetic component, especially in women and in some cultures. None of these characteristics can be replicated by local or regional flaps, such as the cross-finger flap or thenar flap, explaining their limitations and inferiority compared with tissue transferred from the toe.
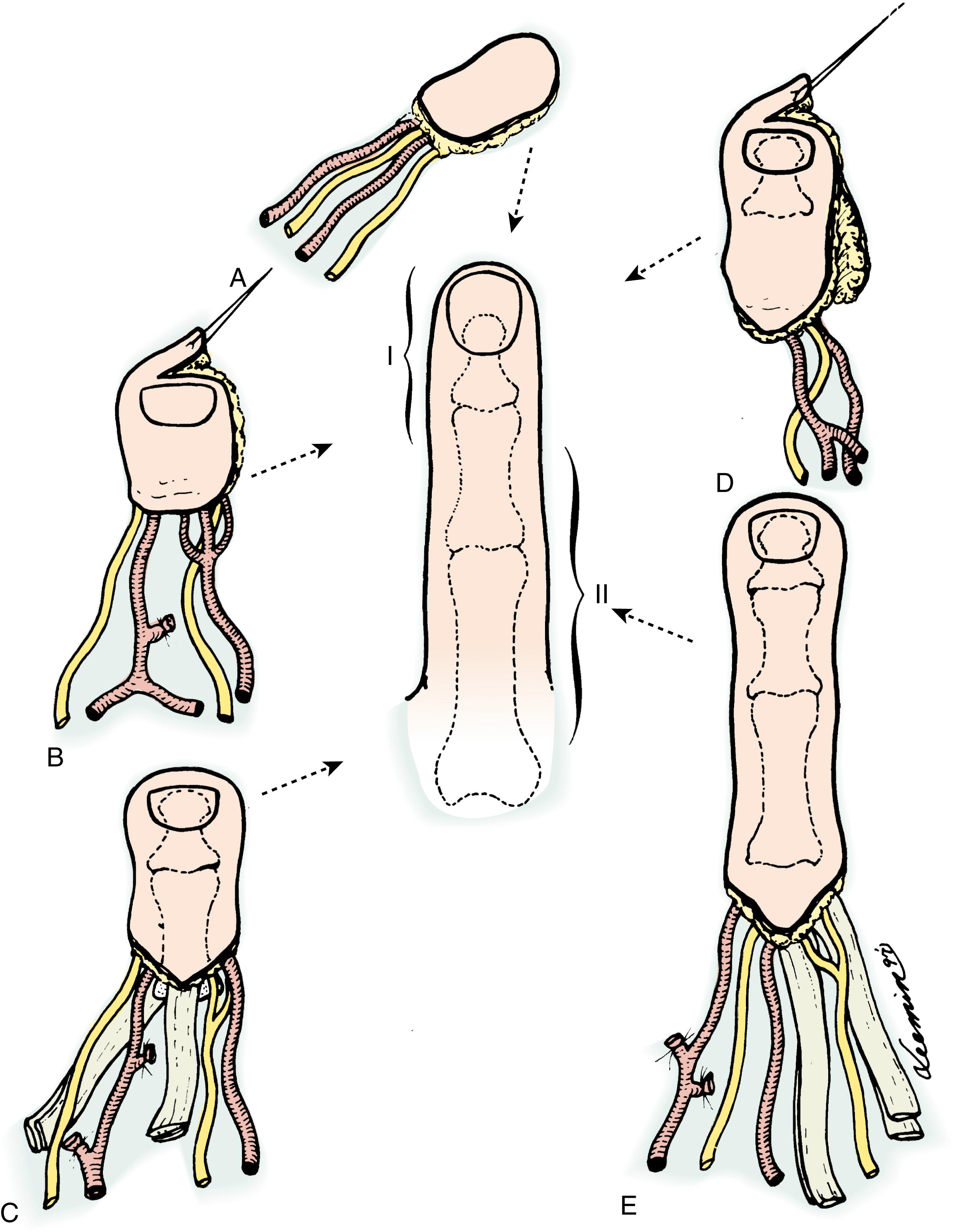
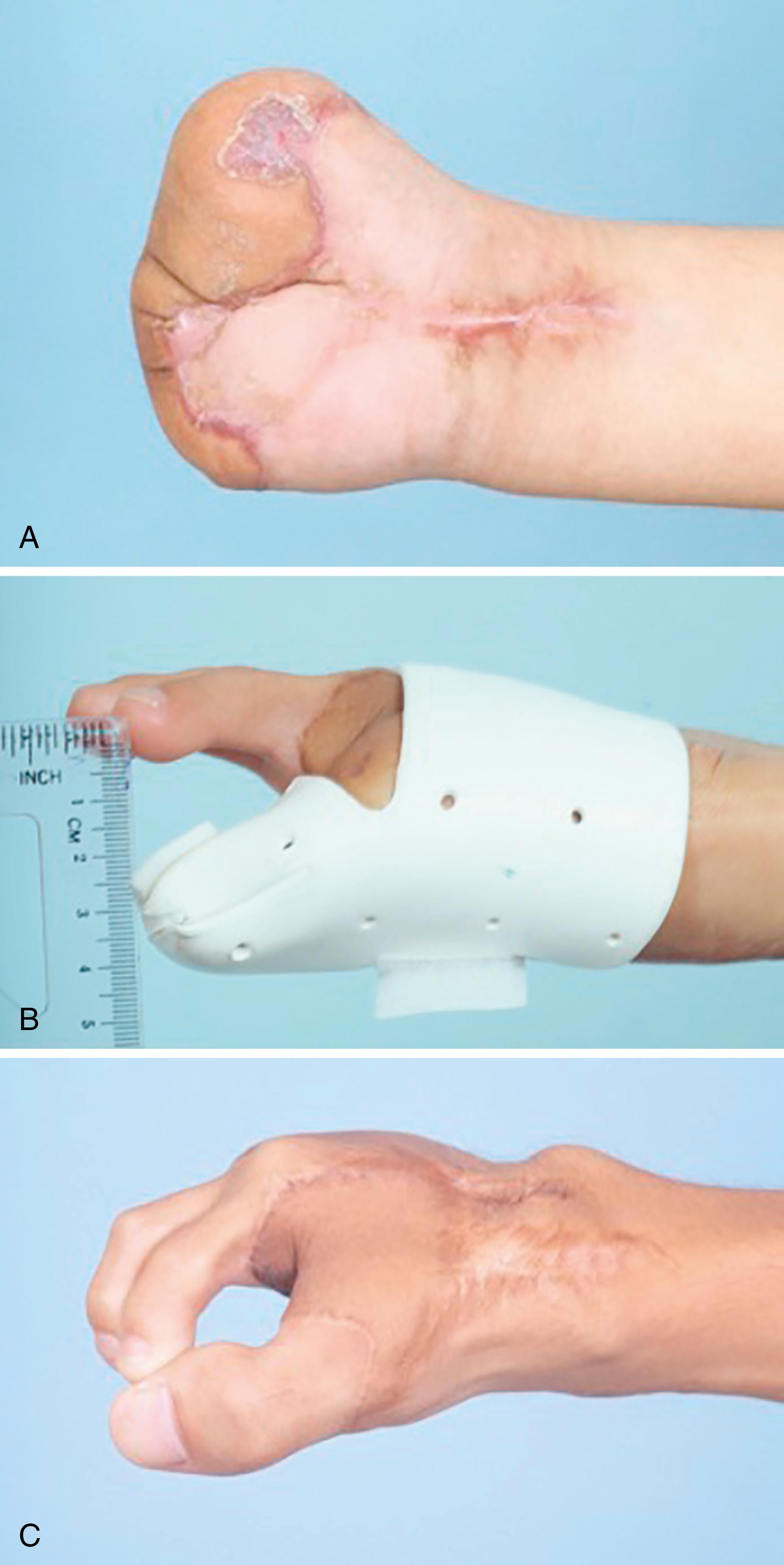
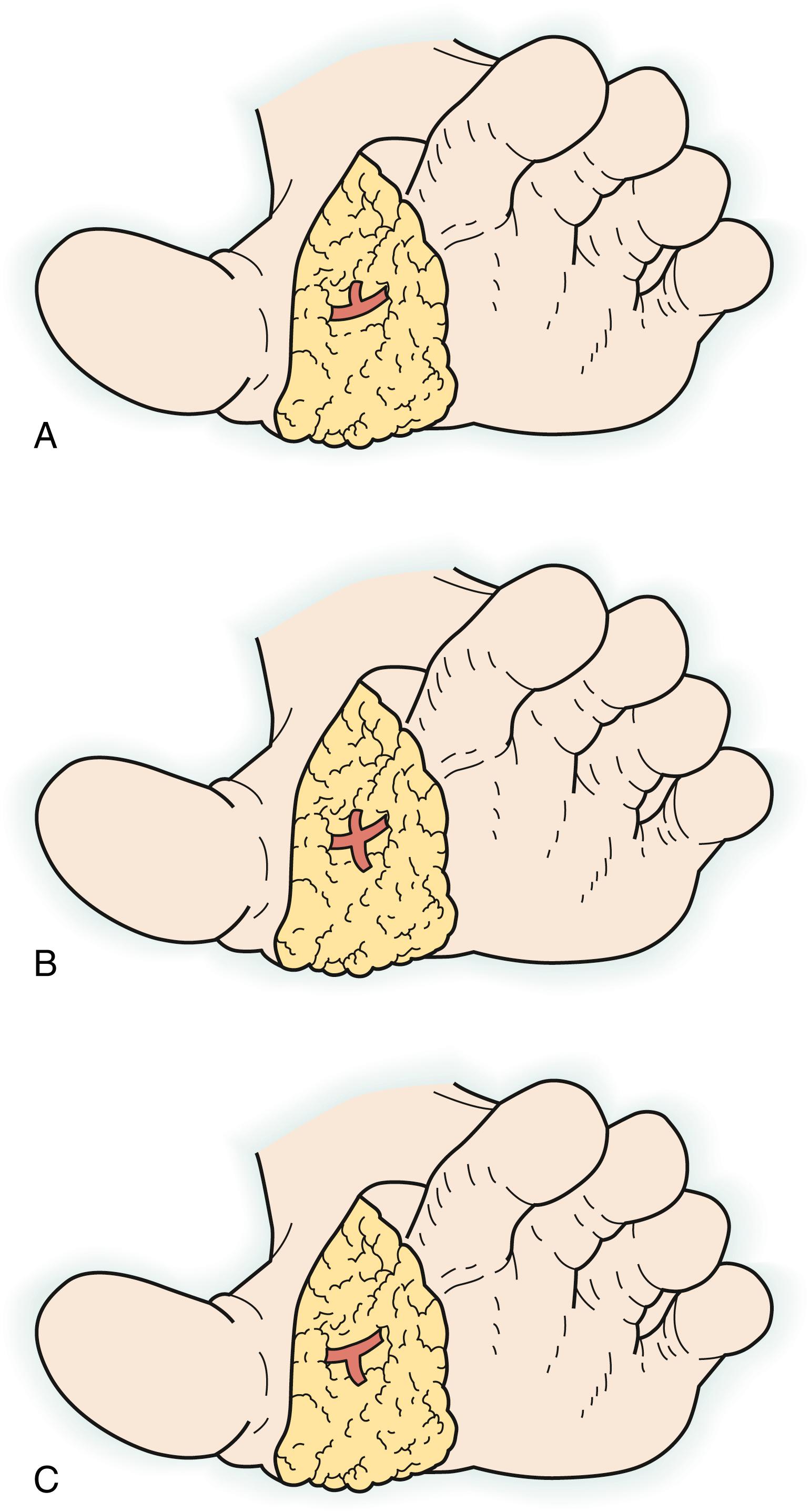
The ideal reconstruction in this part of the finger maintains digit length with adequate soft tissue padding, provides near-normal sensation, and results in recovery of nail function. Reconstructive options using partial toe transplantation in distal defects include a combination of different portions of the nail, pulp, and distal phalanx from the great or lesser toes. Depending on the defect, vascularized nail grafts, , onychocutaneous flaps, , wraparound flaps, , pulp and hemipulp flaps, , , and partial lesser toe transplantation , , can be selected for reconstruction ( Fig. 47.3 ).
Amputations between the base of the distal phalanx and the middle of the middle phalanx require partial toe transfer with inclusion of the distal interphalangeal (DIP) joint and the flexor and long extensor tendons. Modern jobs and hobbies often demand the presence of all digits (e.g., using a computer keyboard, playing a musical instrument). When indicated, this is the amputation level for which the most rewarding results are obtained with toe-to-finger transplantation (see Fig. 47.1 ).
Finger amputation between the FDS insertion and the web space (i.e., base of the proximal phalanx) presents a more controversial indication for reconstruction with lesser toes because a shorter finger might result. If the finger amputation has occurred distal to the middle of the proximal phalanx, the second or third total toe (with the PIP joint) may be long enough to achieve adequate function and esthetic results in some patients (see Fig. 47.2B ). Because of the resulting length discrepancy with the remaining fingers, more proximal amputations in a single finger might not be suitable for reconstruction with total toe transplantation, and ray amputation could yield more acceptable results. Nevertheless, a functional finger with a suboptimal but acceptable appearance can be achieved with highly motivated patients.
The same principles described for single-digit distal amputation apply to the reconstruction of two or more fingers with distal amputation. Priority should be given to reconstruction of the index and middle fingers because they play a more important role in global hand function, specifically in fine manipulation.
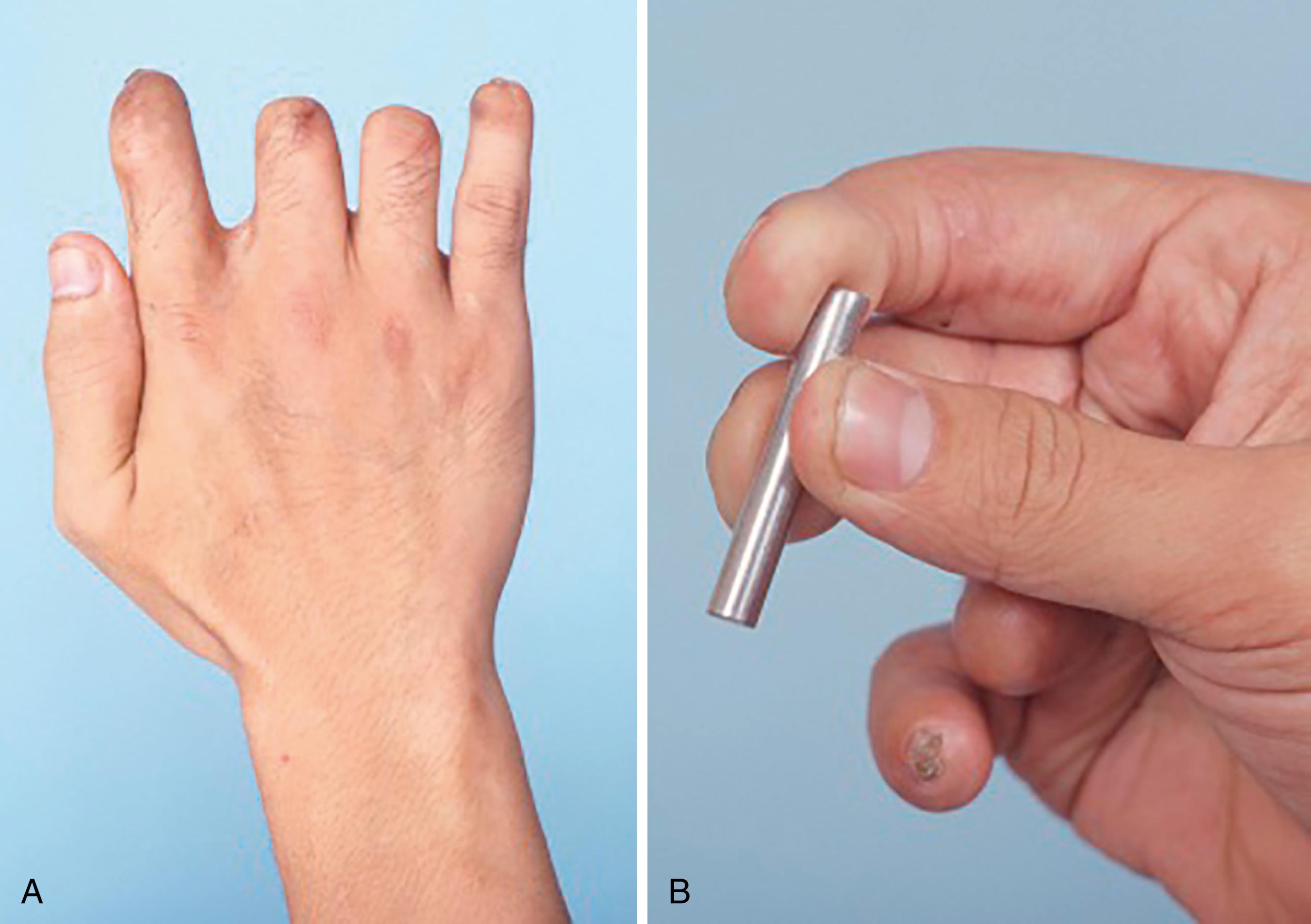
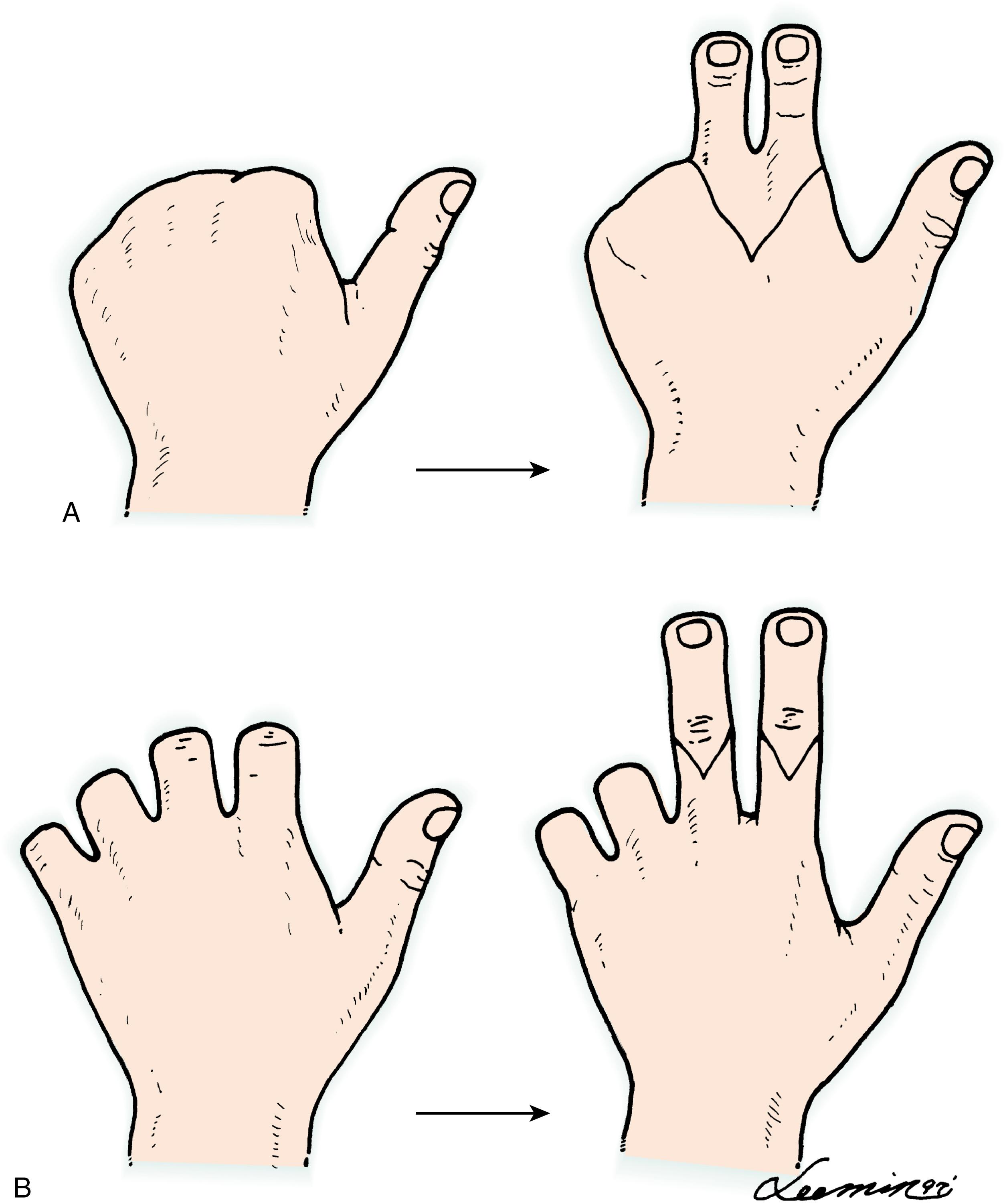
For proximal amputation of two or more fingers, the main purpose of reconstruction is to provide improved prehension ability. It is therefore recommended that reconstruction of at least two fingers be considered. , The advantages of this approach are provision of a useful tripod pinch, stronger hook grip, lateral stability, and handling precision ( Fig. 47.4 ). Reconstructive options for adjacent finger amputations include two separate lesser-toe transplantations or a combined second- and third-toe (or third- and fourth-toe) transplantation on a single vascular pedicle. For two adjacent fingers amputation proximal to the web space, reconstruction with combined second- and third-toe transplantation is a better choice, not only because it reconstructs the web but also because it limits donor morbidity to a single foot and requires only one pair of anastomoses ( Fig. 47.5 ). In amputations distal to the web space, combined toe transplantation may create a syndactylous appearance, so two separate toes (e.g., bilateral second toes) may be preferable. , ,
Recently Lin and colleagues described the use of split second- and third-toe transplantation in situations in which the web space was preserved but bilateral second-toe transplantation was undesirable owing to harvesting of the great toe. For experienced surgeons, this approach may combine the best of both options in these special situations. An additional consideration, when considering tandem second- and third-toe transplantation for reconstruction of two adjacent digits, is the length of the remaining fingers. As a general rule, the remaining fingers have to be shorter than the tip of the normal little finger; otherwise, the transplanted unit cannot simulate the pinch point and grasp arch of full-length fingers. ,
In cases with an intact articular surface on the metacarpal, the tandem toes can be disarticulated at the metatarsophalangeal joint, and the joint capsule and ligaments are circularly divided and used for reconstruction of the MCP joint (i.e., composite joint reconstruction). If the metacarpal articular surface has been damaged or is absent, transmetatarsal toe transplantation is performed.
It is not uncommon for a reconstructive surgeon to be confronted with the scenario of multiple-digit amputations. It becomes difficult to provide a treatment algorithm because these injuries have a wide array of combinations. The same principles apply here as in other digital reconstructions with toe transfers. The proportional length of the fingers should not be disregarded, as even minimal shortening of one finger draws attention to the others and gives a disfigured appearance. Therefore the reconstructive surgeon should feel free to use whatever is available to achieve the aforementioned goals of digital reconstruction. A combination of toe transfer, ray amputation, and lengthening procedures may be necessary. To simplify management, the hand is converted into an acceptable one (del Piñal classification) by means of toe transfer to the distally amputated finger and ray amputation to the proximally amputated finger with great effort to provide three functioning fingers whenever possible. ,
A more severe functional deficit and deformity are present when mutilating hand injuries involve all digits at a proximal level, with or without thumb amputation—a condition referred to as metacarpal hand. The senior author (F-C Wei) and his colleagues have proposed a practical classification of metacarpal hands and defined specific reconstructive options for toe transplantation ( Tables 47.1 and 47.2 ). , , , , This classification divides the metacarpal hand into two types for reconstructive purposes.
| Subtype | Level of Thumb Amputation | Level of Finger Amputation | Recommendations |
|---|---|---|---|
| IA | Intact or distal to IP joint | Distal to MCP joint | Bilateral second toes for amputations distal to web space Combined second and third toes for amputations proximal to web space (transproximal phalanx transfer) |
| IB | Intact or distal to IP joint | Through MCP joint with intact metacarpal articular surface | Combined second and third toes (composite joint transfer) |
| IC | Intact or distal to IP joint | Through MCP joint with damaged metacarpal articular surface or transmetacarpal amputation | Combined second and third toes (transmetatarsal transfer) |
| Subtype | Level of Thumb Amputation | Level of Finger Amputation | Recommendations |
|---|---|---|---|
| IIA | Distal to metacarpal neck | Four fingers at any level proximal to middle of proximal phalanx | Whole or trimmed great-toe transfer (transproximal phalanx transfer) |
| IIB | Proximal to metacarpal neck with adequate thenar muscle function | Four fingers at any level proximal to middle of proximal phalanx | Preliminary distraction lengthening or interpositional bone graft, followed by whole or trimmed great-toe transfer or Transmetatarsal second-toe transfer |
| IIC | Any level with inadequate thenar musculature | Four fingers at any level proximal to middle of proximal phalanx | Thumb reconstruction in a second stage after finger reconstruction and Tendon transfer to restore opposition |
| IID | Any level with damaged carpometacarpal joint | Four fingers at any level proximal to middle of proximal phalanx | Same as for IIA and IIB, but aiming at reconstruction of an immobile thumb post |
In type I, amputation has occurred in all fingers proximal to the middle of the proximal phalanx, and the thumb is either intact or amputated distal to the IP joint (considered the minimum functional length required for precise prehension). In type II, amputation of all fingers is proximal to the middle of the proximal phalanx, with thumb amputation proximal to the IP joint. For the type I metacarpal hand, it is recommended that at least two adjacent digits be replaced. Depending on the finger amputation level relative to the MCP joint (subtypes IA, IB, and IC), bilateral lesser toes or combined second- and third-toe transplantation can be used for reconstruction. For the type II metacarpal hand, a systematic strategy must be followed for the selection of donor toes and reconstructive stages.
If thenar muscle function is adequate (subtypes IIA and IIB), simultaneous reconstruction of the thumb and two adjacent fingers in one stage is preferable ( Fig. 47.6 ). If thenar muscle function is inadequate (subtype IIC), a staged reconstruction is appropriate; the fingers are reconstructed first, and a prosthetic thumb post is used temporarily to assist in determining the length and position of the transferred toe for thumb reconstruction during the second stage ( Fig. 47.7 ). Even more complex are conditions in which both hands are involved because the selection of donor toes should take into account functional impairment and deformity of the feet. ,
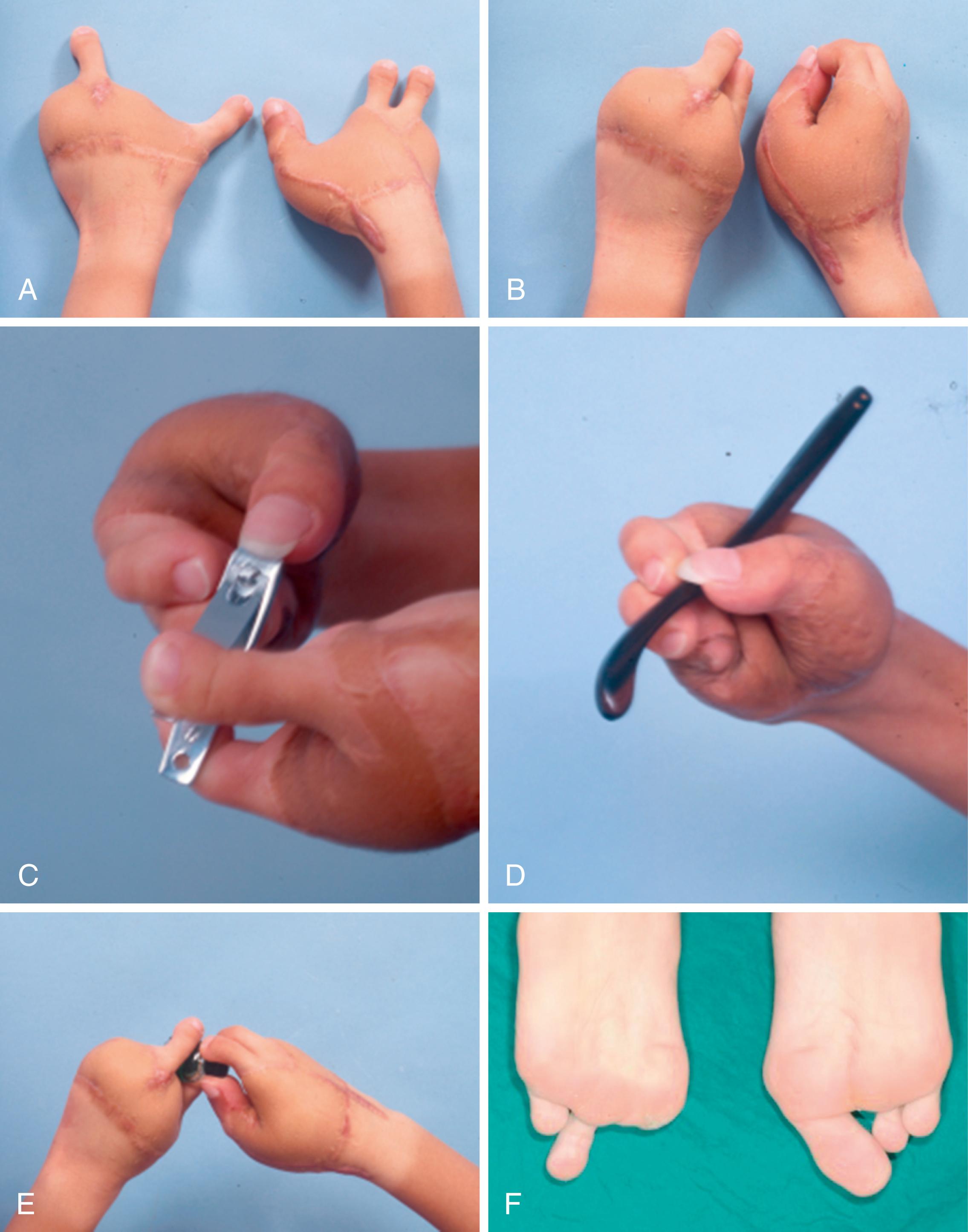
In the bilateral type II metacarpal hand, the dominant hand can be reconstructed with three toes to achieve tripod pinch, and the nondominant hand can be reconstructed with two toes to provide key or pulp-to-pulp pinch. The five toes harvested can be the right second and third toes and the left great, third, and fourth toes, sparing the second toe for foot balance. Our experience has revealed good functional recovery of the hands and no significant donor site morbidity with such an approach ( Fig. 47.8 ).
O’Brien and colleagues described the first toe-to-hand transfer for a congenital hand anomaly in 1978 and several series on different hand malformations, including but not limited to thumb hypoplasia, adactylous hand, symbrachydactyly, and so on.
For traumatic amputation of fingers in the pediatric population, management is similar to what has been described thus far. Replantation should always be attempted even in single-digit amputation. In nonreplantable digit(s), toe-to-hand transfer should be discussed with the parents extensively, and this complex procedure is clearly indicated even in the setting of a single-digit amputation. However, timing is affected by the child’s age (2 years old), and primary transfer is usually avoided in children younger than this.
For congenital absence of fingers, constriction ring syndrome is the ideal indication because the joints, muscles, and tendons proximal to the amputation site are typically present and normal. However, aplastic or hypoplastic conditions, including symbrachydactyly, have also been addressed successfully with toe transfers ( Fig. 47.9 ). , Thumb hypoplasia, in particular, remains controversial because many surgeons believe that results obtained by pollicization are better than toe transfers. Reconstruction of the adactylous hand is usually a staged procedure; although reconstructing the thumb is suggested for the first stage followed by ulnar digit reconstruction in the second stage, it can be done in reverse order.

Technical considerations in congenital reconstructions are similar to those outlined elsewhere in this chapter with a few notable exceptions. Although Lister described performing successful transfers in children as early as 6 months to 1 year old, toe transfer should usually not be attempted until the patient is around 2 years old, when the vessels are of adequate caliber for microvascular anastomosis. Another consideration regarding timing is the unilateral type of the anomaly. It is best to treat children with unilateral malformations early, before adaptive patterns are developed and the use of the abnormal hand is superseded by the normal hand. This situation does not occur in children with bilateral deficiencies.
In aplastic cases, the recipient vessels, nerves, and tendons must be identified before toe harvesting. The toes themselves also may be abnormal in patients with congenital hand abnormalities. As with adults, the first dorsal metatarsal artery (FDMA) is usually dominant and provides the pedicle for the flap. When multiple digits are required, flaps combining two or three toes can be transferred based on the plantar arch. Bony fixation must preserve the epiphyseal plates. Recipient tendons in the aplastic hand may be absent, and primary tendon transfers may be required.
Success rates as high as 96% have been reported. Sensory recovery is usually quite good, with moving two-point discrimination of 5 mm in the series of studies of Foucher and coworkers. However, the most commonly encountered problem is the unpredictable range of motion of the transplanted toe. Transferred toes usually have minimal active DIP motion, an extension deficit at the PIP joint, and a fixed-flexion deformity. Foucher and colleagues reported on 58 children with 65 toe-to-hand transfers with a mean active range of motion of 38 degrees and a mean extension lag of 25 degrees. Nevertheless, children appear to incorporate the transferred toe into their hand function quite well. Growth of the transferred toe is 60% to 100% of the normal toe. ,
Most surgical procedures involved in partial or total toe transplantation use the arterial pedicle to the great and second toe. Several authors have proposed various classifications of the vascular anatomy in the first metatarsal space. All of them describe anatomic variations in the origin of the FDMA; in the relationship between the FDMA and the interosseous muscle; and intermetatarsal ligament, FDMA diameter, and branching patterns. These descriptions have created an image of a complex and highly variable network of vessels in the first–second metatarsal interspace, making the vascular anatomy difficult to understand.
Classically, with most surgical techniques, vascular dissection begins proximally in the dorsum of the foot to identify and follow the course of the dorsalis pedis artery and its continuity as the FDMA. In the senior author’s experience, the FDMA was the dominant artery in approximately 70% of cases, the first plantar metatarsal artery (FPMA) was dominant in 20% of cases, and both arteries had the same caliber in the remaining 10% ( Fig. 47.10 ). (Notably, the pattern of dominance is asymmetric between the two feet in approximately 20% of people.) In the presence of a plantar-dominant arterial system, dissection of the dorsal aspect in the first metatarsal space needs to include only one superficial vein, and there is no need to deepen the dissection, which might damage the foot and is a waste of time.
It is easier to harvest the great or second toe (or any of the various flaps in this anatomic region) by identifying the dominant vascular pattern in the first web space at the beginning of the dissection and proceeding with dissection of the artery in a retrograde fashion. Dissection always starts in the dorsal aspect of the first web space. The junction of the lateral digital artery of the great toe and the medial digital artery of the second toe, arising from the FDMA, is identified over the intermetatarsal ligament ( Fig. 47.11 ). Further dissection of the pedicle is then proximally carried out 2 to 3 cm from this junction. If a dorsal-dominant system is present, retrograde dissection of the FDMA is facilitated by early ligation of the smaller plantar vessel, and the FDMA is isolated proximally. In most cases the artery is superficial to the muscle; however, it may also be localized within or deep in the interosseous muscle. If both vessels have a similar caliber, dissection of the FDMA is preferable because it is much easier and more straightforward. If a plantar-dominant system is noted and the FDMA is either absent or very small, the dissection is continued later during the plantar dissection.
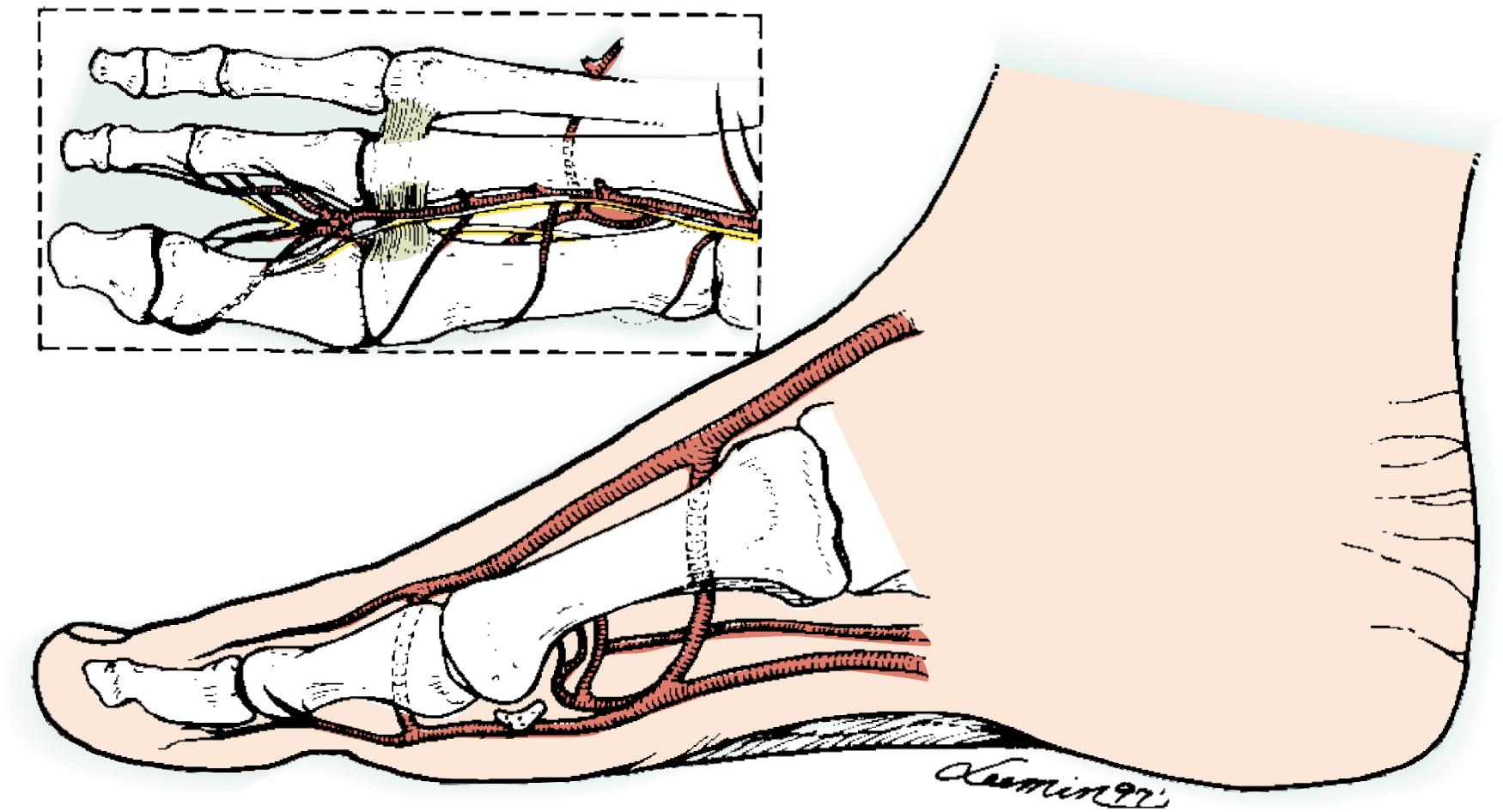
The FPMA is usually isolated up to the middle of the metatarsal shaft on the plantar surface. At this point, the union between the FPMA and the dorsalis pedis artery is located at the proximal communicating artery (or deep perforator). If a longer arterial pedicle is required, dissection of the communicating branch in continuity with the dorsalis pedis artery may be too tedious and destructive to the foot. Thus it is advisable to divide the FPMA and use a vein graft for the vascular anastomosis.
Retrograde dissection is particularly helpful in partial toe transplantation for distal digit reconstruction when only a short pedicle is needed because proximal dissection of the vascular pedicle will not be necessary. In addition, retrograde dissection is helpful in pediatric toe dissection because donor vessel diameter is the most important factor after recipient vessel availability. Therefore, if the FDMA is found to have adequate diameter, dissection proceeds more proximally; otherwise, the FPMA is chosen and no time is wasted. Moreover, routine preoperative angiography of the donor foot is not required when this approach is used to harvest any toe or flap based on the arterial system of the first metatarsal space.
Total transfer of the great toe is selected for thumb reconstruction when the amputation level is at either the proximal phalanx or metacarpal level. It aims to provide a new thumb with a better range of motion and a broader pulp surface for a more powerful pinch. However, it is often too large to simulate the normal thumb on the opposite side. The great-toe wraparound technique was developed by Morrison using the great toenail, skin envelope, and conventional bone graft to circumvent the size problem. Although it yields a nice-looking thumb, it does not provide a mobile IP joint. Trimmed transplantation of the great toe combines the advantages of total transfer and the great-toe wraparound technique. , It is indicated when there is an unacceptable size difference between the thumb on the normal opposite side and the great toe to be harvested, especially when a mobile IP joint is desirable. It is worth mentioning that with the trimmed great-toe technique, a reduction of 18 degrees in IP joint motion is expected, which does not seem to affect pulp-to-pulp pinch prehension.
The great toe usually looks portlier than the thumb, with wider transverse and anteroposterior diameters. The discrepancy involves bone as well as soft tissue elements ( Fig. 47.12A ). To assess the size discrepancy between the great toe and the normal thumb, the circumferences of the great toe and the normal thumb are measured at three points: the nail eponychium, the widest point (corresponding to the IP joint), and the middle of the proximal phalanx. The thumb measurements are transposed to their corresponding points on the great toe. An additional 2 to 3 mm is added to each measurement to allow direct closure without tension. The residual medial skin strip usually measures 0.5 to 0.8 cm wide, which represents the difference between the toe and thumb circumferences. This should be tapered to a point around the tip of the toe, leaving 2 mm of nail fold to facilitate skin closure. The proximal skin incision is determined by the level of thumb amputation and is usually marked in a circular or “V” shape (see Fig. 47.12B ). Although it is possible to trim the nail together with the underlying nail bed, this is not recommended because the nail fold may become deformed.

The procedure starts by identifying one sizable vein and the dominant arterial supply in the first web space. The vascular pedicle is dissected in a retrograde fashion to the desired length and diameter. Branches of the deep peroneal nerves are preserved. The extensor tendon is then dissected on the dorsal side, and the neurovascular bundle and flexor tendon are isolated on the plantar side. Care is taken to place the incision on the plantar aspect, lateral to the head of the first metatarsal, to prevent a scar over the weight-bearing area.
Next, the medial skin strip is incised and elevated from distal to proximal. The incision is deepened to the periosteum at the tip of the distal phalanx (see Fig. 47.12C ) but remains superficial to the medial collateral ligament on the medial surface of the IP joint. The second incision is made all the way through the periosteum. The collateral ligament, joint capsule, and periosteum are elevated as a plantar-based single, thick, strong composite soft tissue envelope, which we have designated a “perijoint flap.” This subperiosteal (perijoint flap) elevation is continued along the hemicircumference to the middle of the plantar surfaces of both the proximal and distal phalanges (see Fig. 47.12D ). A longitudinal osteotomy (see Fig. 47.12E ) is then performed with an oscillating saw while carefully protecting the neurovascular bundle. This removes a 4- to 6-mm width of the medial joint prominence, along with a 2- to 4-mm width of the phalangeal shafts.
A smooth contour of the osteotomy edges is obtained using a high-speed bur. The hemicircumferential composite perijoint flap is redraped and the redundant portion is trimmed, followed by repair under proper tension with interrupted sutures using nonabsorbable material. The repair should be tight enough to maintain joint stability (see Fig. 47.12F ). The medial skin incision is also approximated with interrupted sutures (see Fig. 47.12G ). Care should be taken to prevent injury to the nail bed or matrix because this can result in a deformed nail. Finally, the proximal phalanx is osteotomized, preserving at least 1 cm of the base of the proximal phalanx and leaving the great toe attached only by its vascular pedicle. After removal of the tourniquet, the transplant is allowed to perfuse for at least 20 minutes before proceeding with transplantation (see Fig. 47.12H ). The donor site is closed primarily. The osteotomy edges are smoothed and the remaining proximal portion of the medial skin flap of the great toe can be used to assist tension-free closure, if required.
The amputated stump is prepared through a cross-incision creating four flaps (see Fig. 47.12I ). These flaps are mobilized to prepare the bone, extensor and flexor tendons, and digital nerves. They also allow smooth closure of the skin between the recipient site and transplanted toe for a better appearance of the reconstructed thumb. The recipient artery can be the common digital artery (our first choice), the princeps pollicis artery, or the radial artery in the anatomic snuffbox. The bone, extensor and flexor tendons, recipient artery, vein, and nerves are prepared at the recipient site in the usual manner.
Flap insetting and repair of tendons and neurovascular bundles are performed as described in other sections of this text. When closing the wound defect, preservation of skeletal length and good skin coverage are important. In transplantation of the great toe, it is advisable to preserve at least 1 cm of the proximal phalanx to maintain foot span for a better appearance and to preserve push-off function of the donor foot. Skin grafting of the donor site should be avoided. With adequate planning, rarely should there be a problem achieving tension-free closure of the wound in the foot. No drains are required at the donor site.
To reduce the stigma following great toe transfer, some advocated removal of the second metatarsal bone and transposition of the second toe on top of the proximal phalanx of the hallux, followed by interposition of a tibial (medial) glabrous flap from the tibial aspect of the hallux onto the tibial side of the second toe to increase its size, and finally eponychial flap to increase the nail show on the second toe. The experience reported was limited to six cases, however.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here