Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Thoracentesis is a percutaneous procedure during which a needle is inserted into the pleural space to remove fluid for diagnostic or therapeutic purposes. When performed using real-time ultrasound (US) guidance, thoracentesis has an extremely low rate of complications.
The thoracic cavity is lined by thin serous membranes: the visceral pleura, which wraps around the lungs, and the parietal pleura, which lines the inner surface of the thoracic cavities and meets the visceral pleura at the root of the lungs in the mediastinum. The space between these two linings is called the pleural space . Each pleural membrane consists of a superficial mesothelial cell layer and an underlying connective tissue layer containing systemic capillary beds. These membranes are leaky, allowing for easy movement of both fluid and protein. In the healthy state, hydrostatic pressure of the systemic capillaries produces a small net movement of fluid across both pleurae into the low-pressure pleural space. This fluid is removed primarily via lymphatic stomata found in the parietal pleura. Normally there is a small amount of fluid, estimated at 0.26 mL/kg of body mass, present in the pleural space. An excess amount of fluid in the pleural space is termed pleural effusion .
Because the lymphatic system has the ability to remove 30 times more pleural fluid than its basal rate, it is believed that in most instances the development of a pleural effusion requires both an increase in fluid entry into the pleural space and a decrease in its removal.
The most common causes of pleural effusion in adults are congestive heart failure (CHF), pneumonia, malignancy, pulmonary embolism (PE), and cirrhosis. The most common cause in children is pneumonia, followed by heart failure, and malignancy. Pleural effusions can be classified as either transudates or exudates. Distinguishing between transudates and exudates narrows the differential diagnosis and directs management and therapy. A comprehensive list of causes can be found in Box 9.1 . The most common are discussed in the following sections.
Congestive heart failure
Cirrhosis
Nephrotic syndrome
Peritoneal dialysis
Pericardial disease
Central venous occlusion
Myxedema
Acute atelectasis
Bone marrow transplantation
Urinothorax
Malignancy
Pneumonia
Pulmonary embolism
Tuberculosis (high-prevalence region)
Post–myocardial infarction
Post–coronary artery bypass graft
Trauma
Esophageal perforation
Pancreatitis
Intraabdominal abscess
Abdominal surgery
Collagen vascular disease
Drug-induced
Chylothorax
Asbestosis
Sarcoidosis
Uremia
Meigs syndrome
Ovarian hyperstimulation syndrome
Radiation therapy
Transudates are caused by either an increase in intravascular hydrostatic pressure or a decrease in intravascular oncotic pressure. This generates an increased flow of fluid into the pleural space across noninjured capillary beds. These effusions are typically straw colored and serous with very low cellular and protein content.
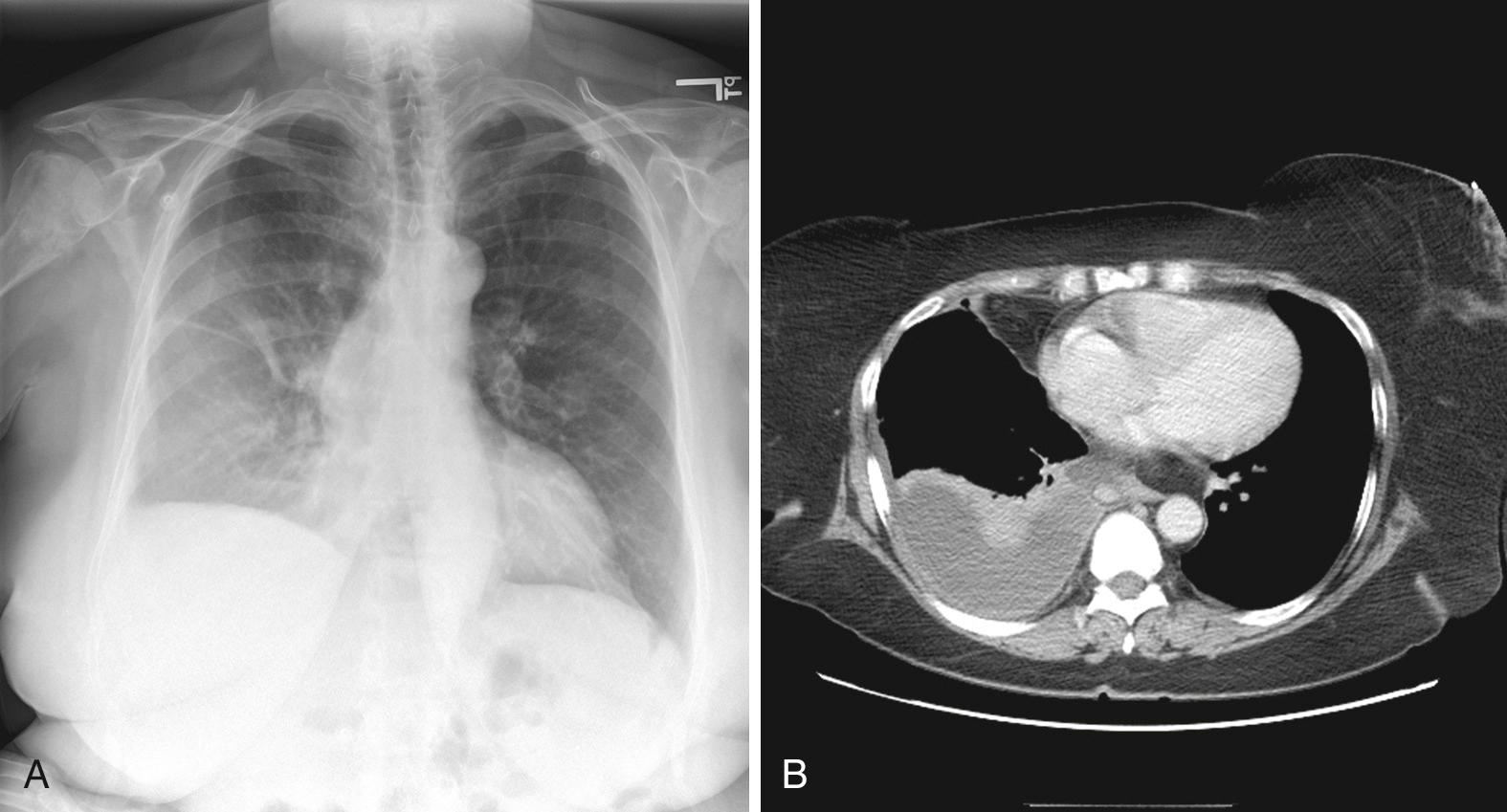
The most common cause of a transudate is CHF. The increased pulmonary capillary hydrostatic pressure in patients with CHF results in a net flow of fluid into the pulmonary interstitium. This fluid readily moves across the leaky visceral pleura into the pleural space. In addition, elevated systemic capillary pressures associated with CHF increase fluid flow across the pleural membranes into the pleural space and decrease lymphatic flow out of the thorax. Any process that causes compromised left ventricular outflow can result in a pleural effusion, including myocardial infarction, cardiomyopathy, and valvular disease. These effusions are typically small and bilateral with larger effusions on the right ( Fig. 9.1 ). Highly asymmetric and large effusions should raise suspicion for another cause.
Patients with cirrhosis are frequently hypoalbuminemic, which leads to a chronic state of decreased plasma oncotic pressure. This imbalance between the hydrostatic and oncotic forces across the pleural membrane results in an effusion. In addition, experiments have shown that high volumes of ascites can stretch the diaphragm enough to allow fluid to pass through preexisting microdefects.
Similarly, in several other disease states such as the hypoalbuminemic state of patients with nephrotic syndrome, intraabdominal fluid associated with peritoneal dialysis, or retroperitoneal fluid with obstructive uropathy can cause transudative pleural effusions in patients with renal disease.
Exudates are caused by pleural inflammation, increased pleural membrane permeability, or lymphatic obstruction. More than 90% of exudative effusions are due to malignancy, pneumonia, PE, and gastrointestinal diseases (e.g., pancreatitis, esophageal perforation). Tuberculosis (TB) should be added to this list in patients from high–TB prevalence regions.
The primary mechanism of cancer-related pleural effusion is obstruction of pleural lymphatic outflow, either via damage to lymphatic stomata or more distal involvement of the mediastinal lymph nodes. Other mechanisms include metastases to the pleurae increasing capillary permeability and obstruction of the thoracic duct with consequent chylothorax.
A pleural effusion associated with pneumonia or a lung abscess is termed a parapneumonic effusion. In the first, or exudative, stage of parapneumonic effusion, an increase in pulmonary interstitial fluid leads to flow of sterile fluid and inflammatory cells across the visceral pleura into the pleural space. When the infection and resultant inflammation continue unchecked, there is increased capillary permeability with bacterial and additional inflammatory cell transfer to the pleural space, causing the parapneumonic effusion to become complicated. This worsening pleural space inflammation results in the deposition of fibrin on the pleural surfaces with formation of loculations, and finally, in a tough peel that encases the lung.
A pleural effusion develops in at least 20% of those with PE. Therefore when the cause of the effusion is unclear, PE should be strongly considered. The effusions associated with PE are often too small to require thoracentesis, but they have been shown to be uniformly exudative, probably resulting from ischemia- and infarction-induced increases in pulmonary capillary permeability.
Effusions can also result from significant injuries such as the following. Esophageal rupture can result from forceful vomiting, as in the case of Boerhaave's syndrome, or from instrumentation, as in the case of endoscopy, gastroesophageal balloon tamponade tube placement, or rigid nasogastric tube placement. Hemothorax can result from traumatic injuries, cannulation of the subclavian vein or artery, PE, or aortic aneurysm rupture. Chylothorax develops from acute disruption of the thoracic duct, usually in the setting of trauma or malignancy. These effusions are usually large-volume collections that accumulate over an extremely short period and rapidly compromise both oxygenation and circulation.
Symptoms of small pleural effusions are usually representative of the underlying disease process and not the effusion itself. An effusion greater than 300 mL may cause symptoms on its own, usually dyspnea, chest pain, or cough. The dyspnea from a larger pleural effusion is typically the result of impaired chest wall and diaphragm movement and not decreased oxygenation or lung function. Chest pain may be dull and aching from the effusion itself or pleuritic from localized irritation of the parietal pleura, which has abundant nerve fibers. Cough is usually attributed to bronchial irritation from compression of the lung parenchyma. Patients occasionally present in extremis from a large pleural effusion that is compressing the heart and causing tamponade physiology with cardiovascular compromise.
There are numerous described physical exam findings for pleural effusion, but these may be difficult to appreciate in the emergency department (ED) environment depending on the acuity of the patient and the ambient noise ( Box 9.2 ). Dullness to percussion and decreased tactile fremitus over the effusion have been shown to be the most useful physical exam findings on systematic review. Percussion over the effusion produces a characteristic dull resonance, which shifts when the patient changes position if the fluid is free flowing. Placing the flat hand over the patient's back while the patient says the word “toy” or the phrase “blue moon” will demonstrate a reduced or absent fremitus because the fluid separates the lung from the thoracic wall and absorbs vibrations from the lung.
Decreased chest wall excursion
Bulging intercostal spaces
Egophony at superior border of effusion
Diminished breath sounds
Dullness to percussion
Decreased tactile fremitus
Pleural friction rub
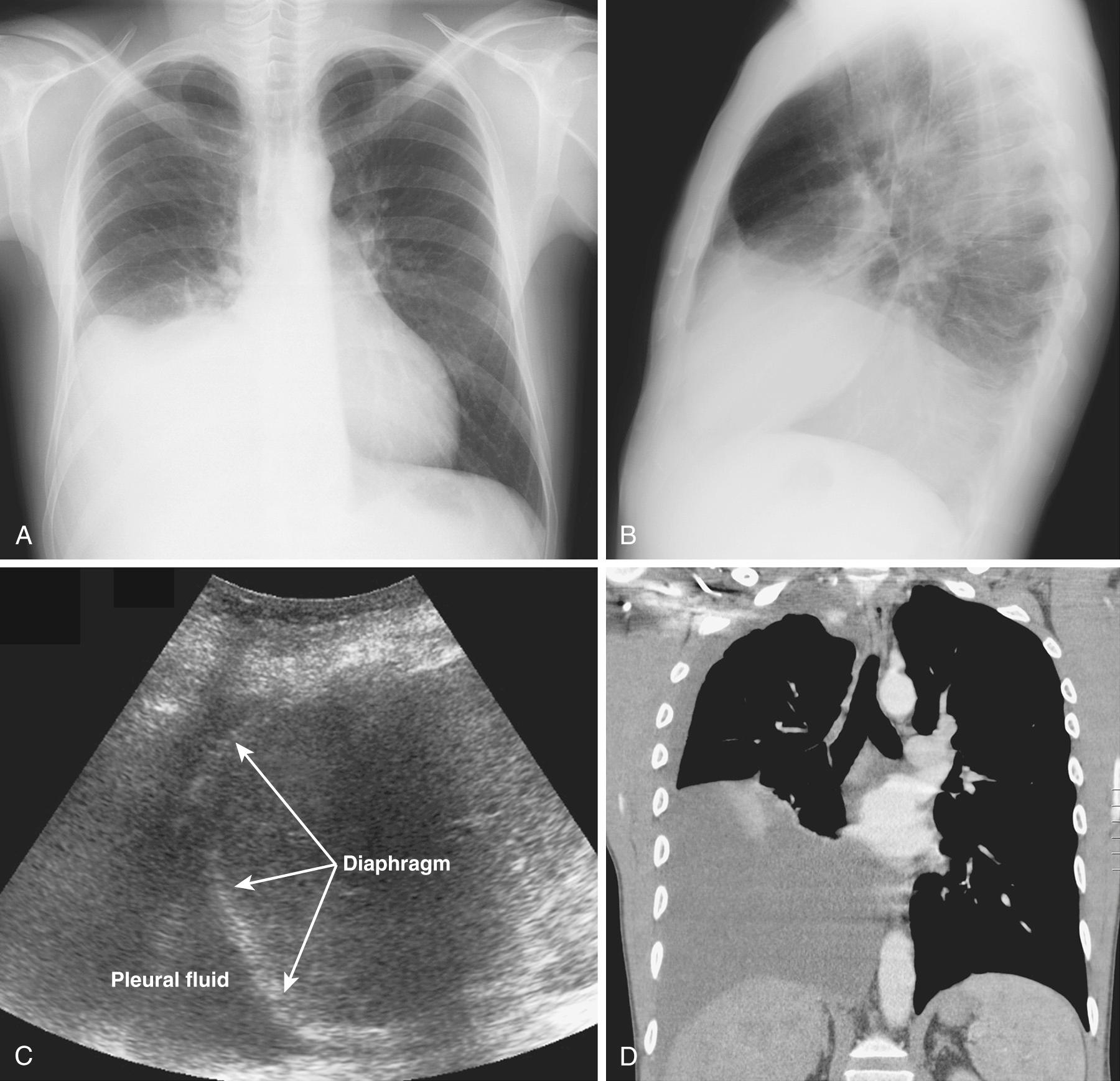
Because pleural fluid is denser than air-filled lung, a free-flowing effusion will first accumulate in the most dependent parts of the thoracic cavity: the subpulmonic space and the lateral costophrenic sulcus. Pleural effusions are usually visible on an upright chest radiograph if 200 to 250 mL of fluid is present. A lateral radiograph may reveal an effusion of 50 to 75 mL.
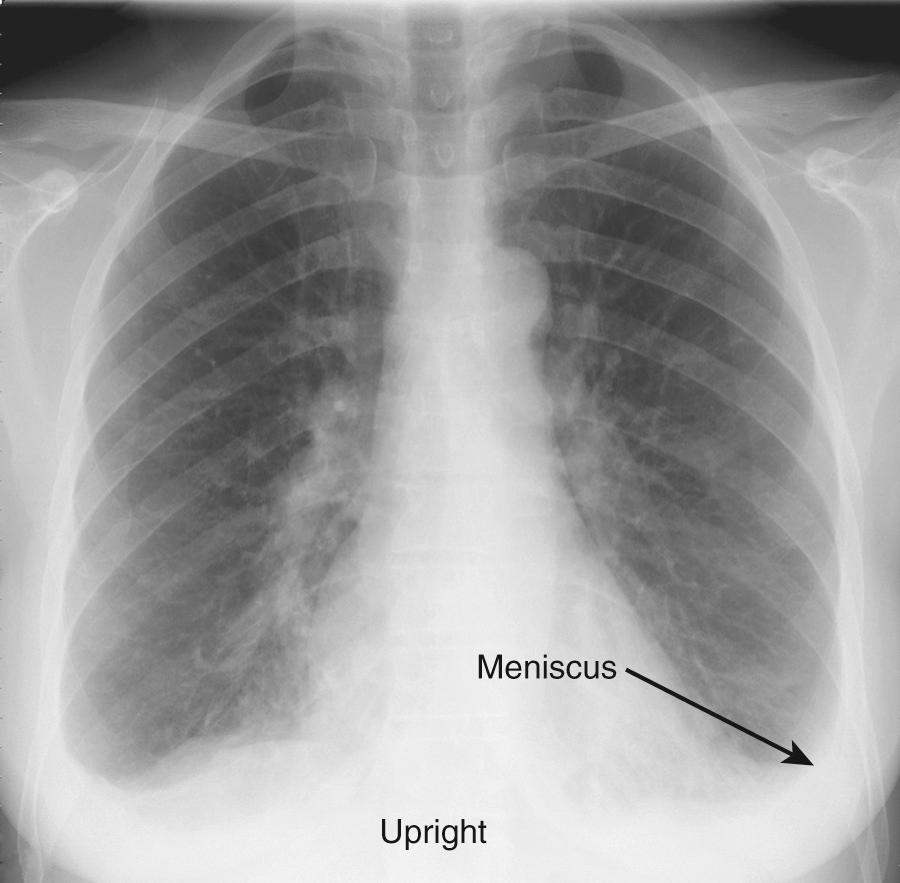
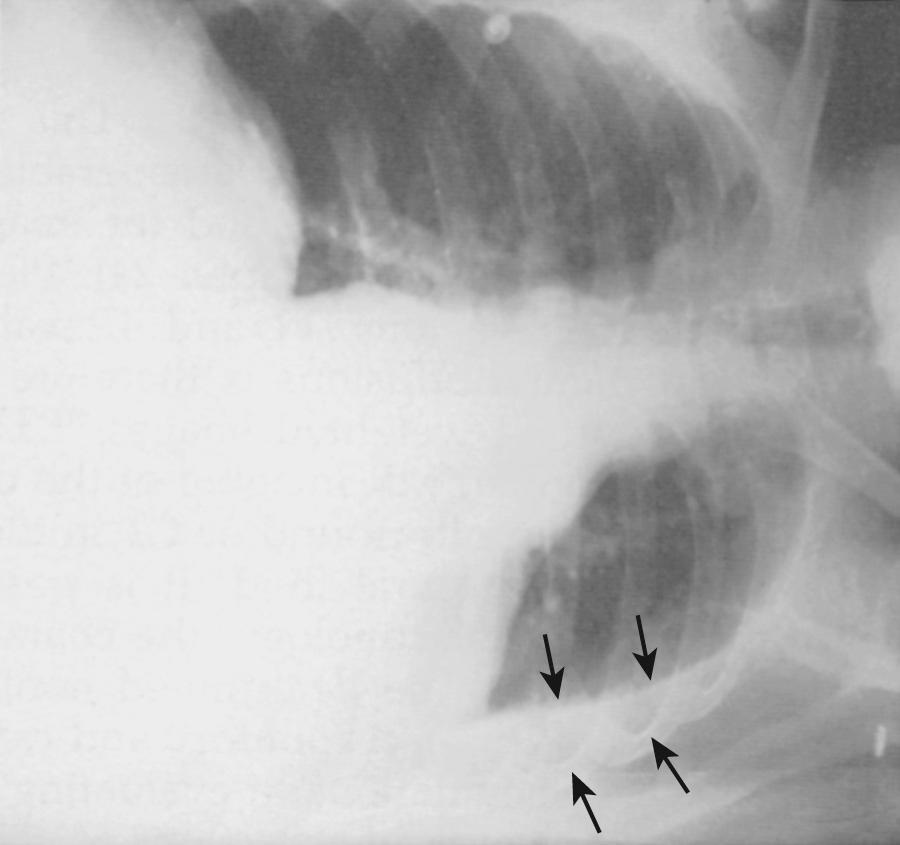
The earliest recognized sign of a pleural effusion on an upright chest radiograph is blunting of the lateral costophrenic angle, which may be seen on either the frontal or the lateral view ( Fig. 9.2 ). With a larger free-flowing effusion, the pleural fluid appears as a meniscus that curves downward toward the mediastinum in the frontal view and appears “lowest” midway through the thoracic cavity on the lateral view ( Fig. 9.3 ). The presence of air from pneumothorax or abscess may alter the appearance of the meniscus to more of a straight line (air-fluid level).
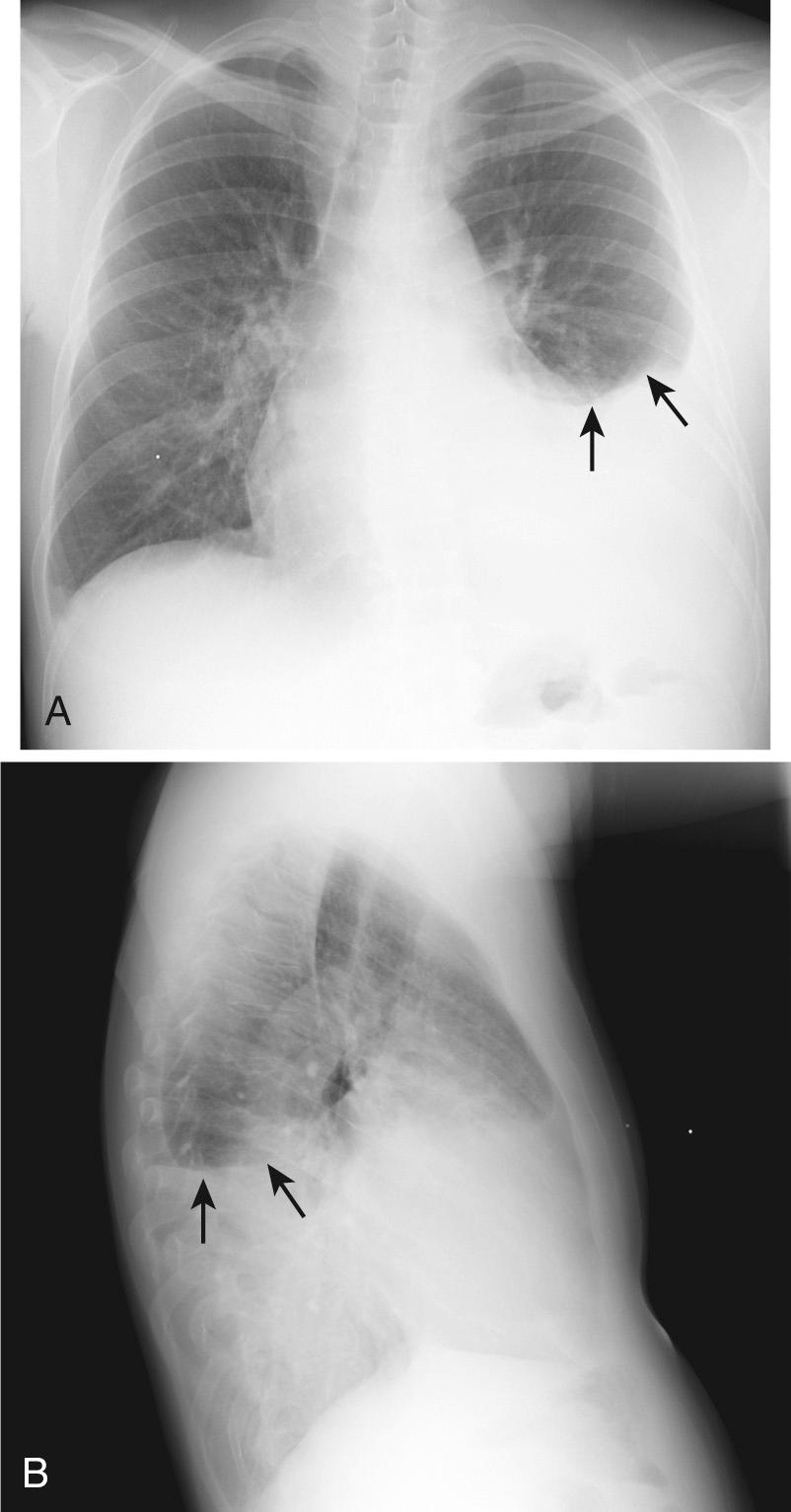
Occasionally, up to 1000 mL of fluid collects in the subpulmonic space and causes neither blunting of the costophrenic angle nor a meniscus appearance on the upright radiograph. This is called a subpulmonic effusion ( Fig. 9.4 ). This should be suspected if the hemidiaphragm is elevated and the hemidiaphragm dome peaks more laterally than expected on the upright frontal radiograph.
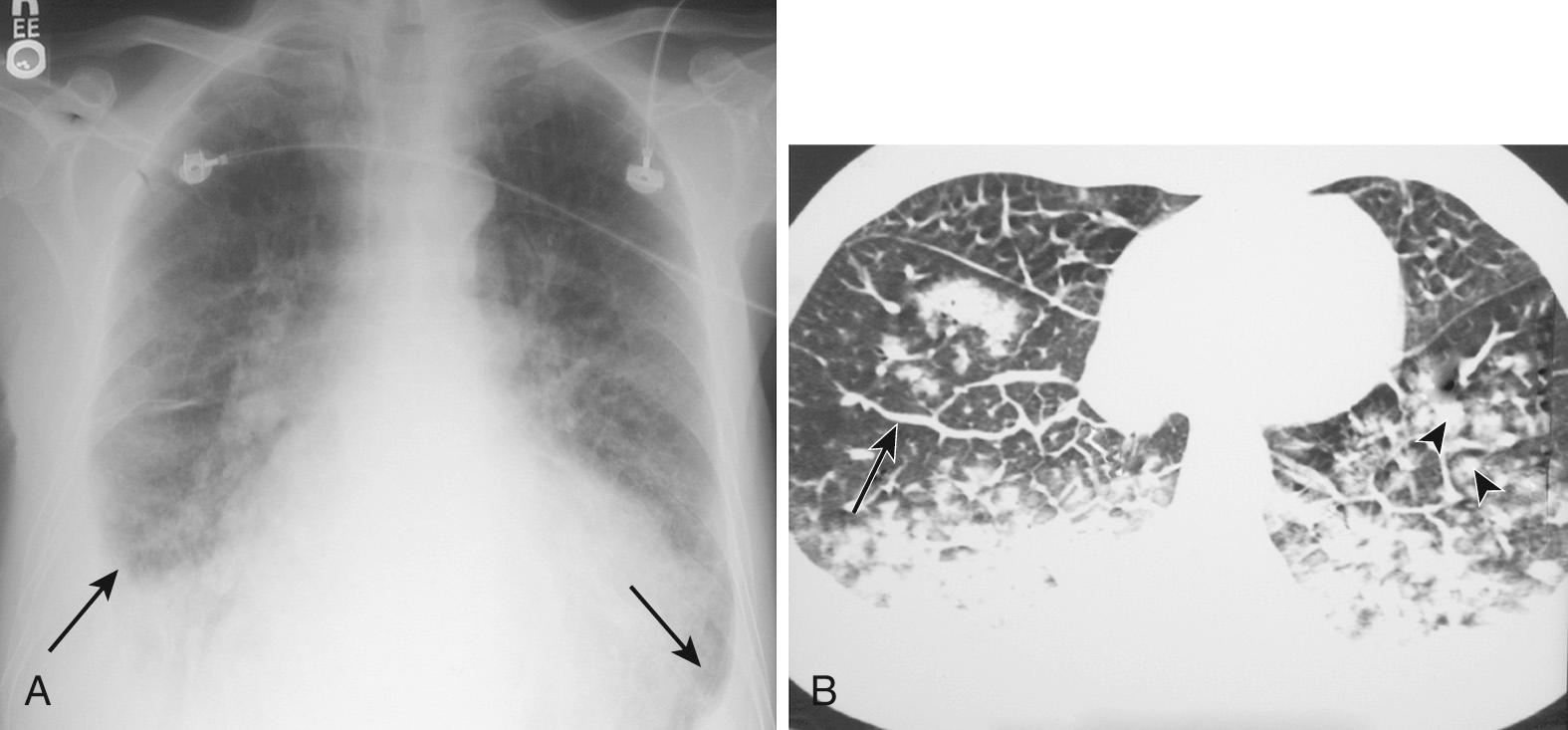
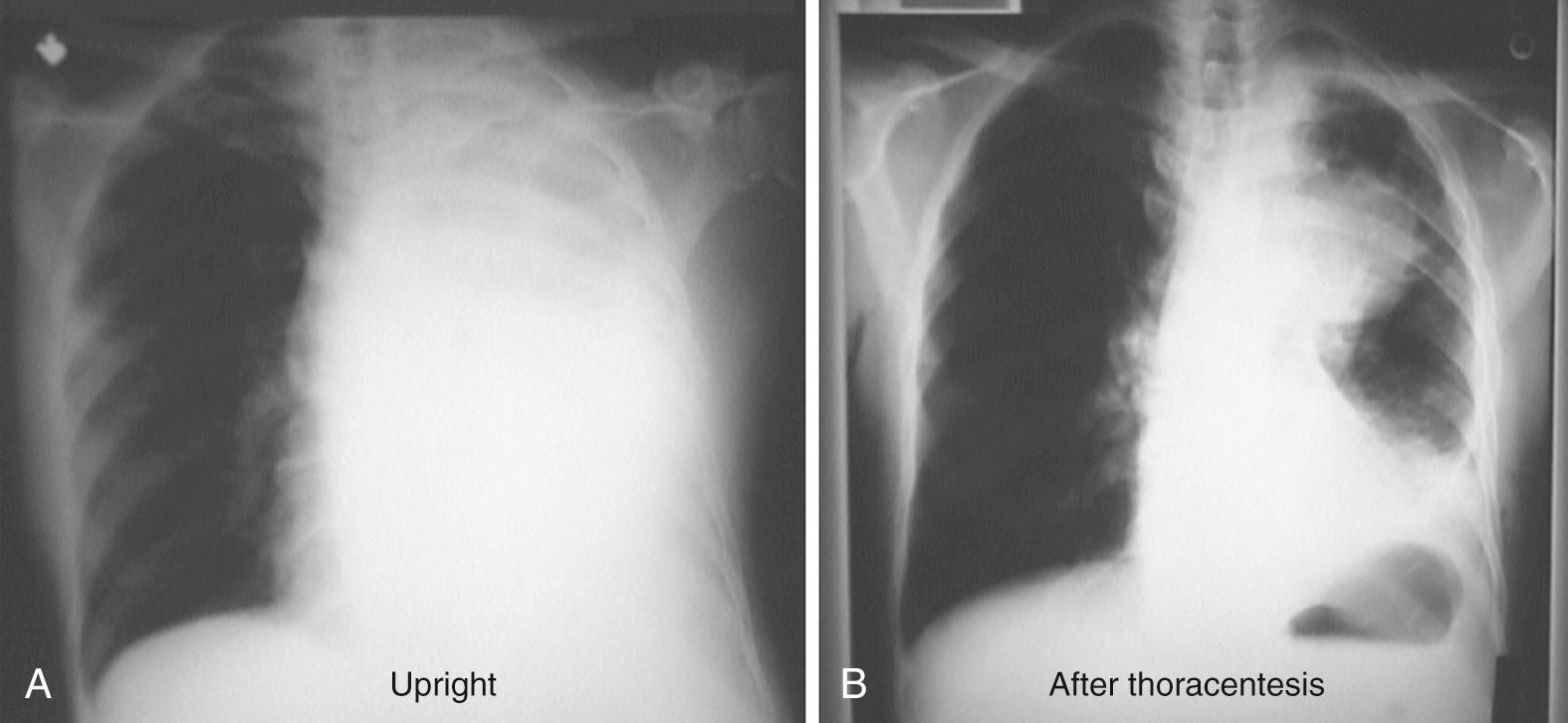
Pleural effusions are challenging to identify on chest radiograph in the supine patient, and even a significant amount of fluid may not be appreciated. If the effusion is large enough, a diffuse haziness may be appreciated ( Fig. 9.5 ). Other findings include apical capping, obliteration of the hemidiaphragm, partial opacification of a hemithorax, and a widened minor fissure.
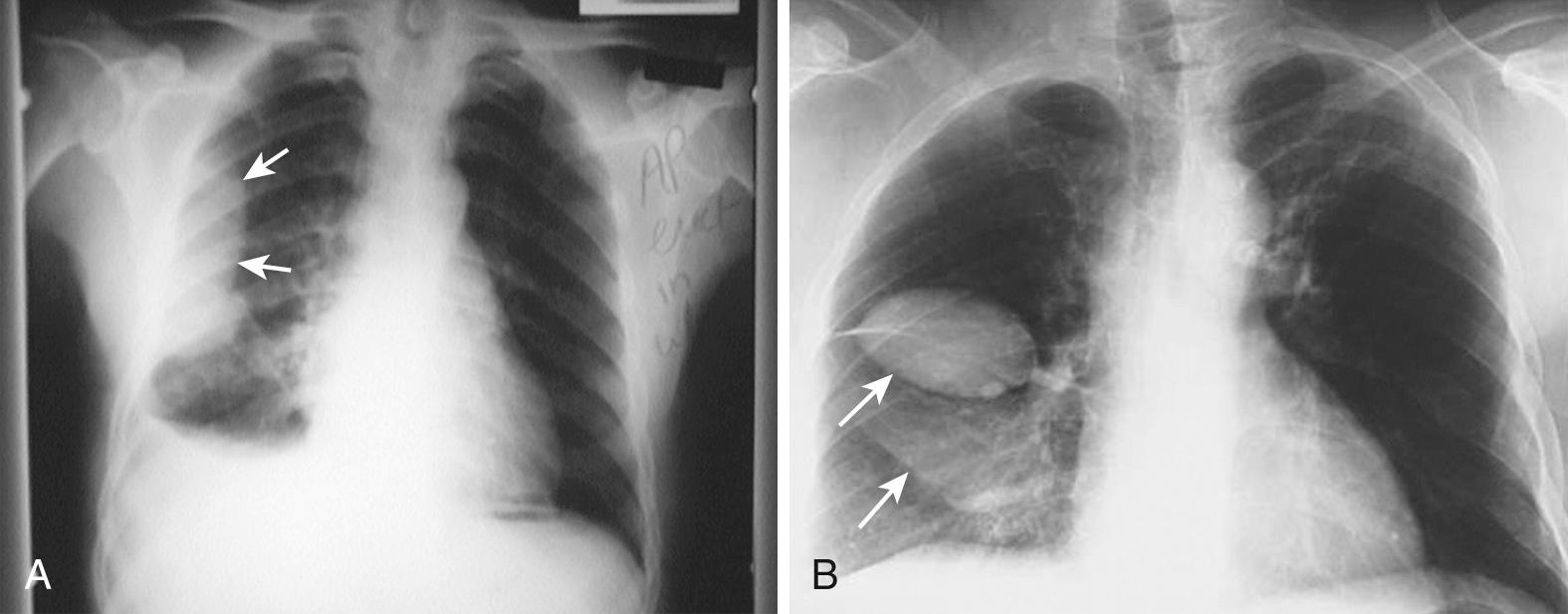
Obtaining bilateral decubitus radiographs when a pleural effusion is seen or suspected will confirm the presence of a free-flowing effusion and allow for visualization of loculations, contained abscesses, infiltrates, or masses. With the side of the effusion down, a simple pleural effusion will follow gravity and layer between the floating lung and the chest wall ( Fig. 9.6 ). A lateral decubitus view on the opposite side draws the fluid toward the mediastinum and allows further visualization of the lung parenchyma.
With a diseased or scarred lung, tissue adhesions can trap pleural fluid within the parietal, visceral, or interlobar surfaces. Because these adhesions anchor the fluid, loculated effusions are often described as “D-shaped” ( Fig. 9.7 ). Fluid loculated in the fissures assumes a lenticular shape.
In the case of a massive pleural effusion, the entire hemithorax is opacified ( Fig. 9.8 ). On such films, identification of mediastinal shift is a key to identifying the underlying disease process. In the absence of a diseased lung or mediastinum, large fluid collections push the mediastinum contralaterally. When the mediastinum is shifted toward the effusion, the lungs and main stem bronchi are diseased, obstructed, or both. When the mediastinum is fixed midline, it is likely invaded by tumor.
Computed tomography (CT) is more sensitive than plain films in detecting very small effusions and can readily assess the extent, number, and location of loculated pleural effusions. In the distinct anatomic relationships shown on cross-sectional CT, free-flowing pleural fluid will form a sickle shape in the most dependent regions (see Fig. 9.5 ), whereas loculated fluid collections will remain lenticular and relatively fixed in space. CT can also be extremely useful in elucidating the underlying disease process.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here