Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Anatomical principles underpin optimal oncological and functional outcomes in the surgical management of prostate cancer. Therefore, an in-depth understanding of pelvic anatomy is prerequisite for all prostate cancer surgeons.
Recent technology development, such as the advent of 10-times magnification, high-definition video, and 3D video systems in robotic and laparoscopic surgery, enables the surgeon to identify subtle anatomical structures like never before, ever increasing the precision of surgery.
Unfortunately, understanding the complex anatomy of the pelvis is made particularly challenging by the existence of differing terminology. The EAU Section of Uro-Technology (ESUT) expert group on laparoscopy highlighted the importance of uniform terminology during radical prostatectomy in their 2013 editorial. We refer readers to this paper for a concise summary of the various anatomical terms used in this area.
In this chapter, we review the current literature to provide an overview of the functional anatomy of the male pelvis relevant to radical prostatectomy surgery.
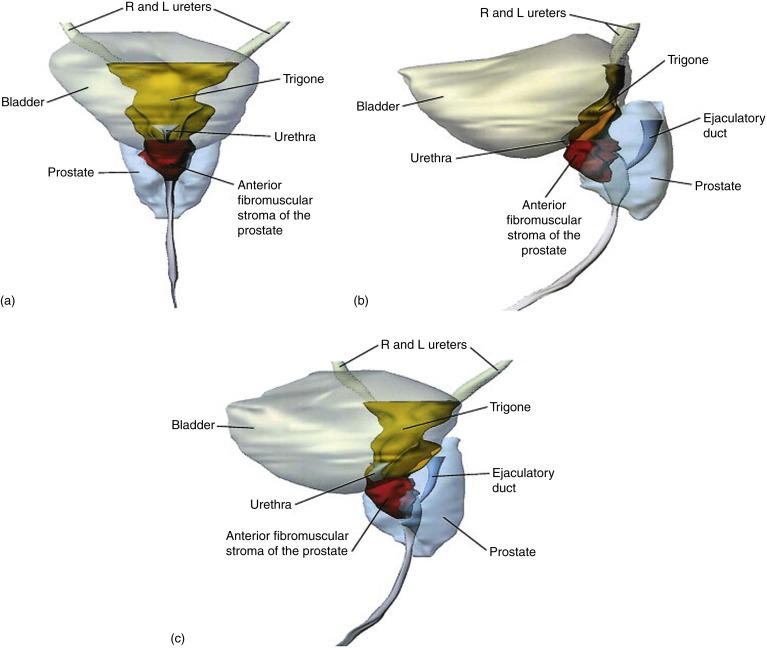
The prostate gland comprises acini of varying shapes and sizes embedded in a fibromuscular stroma. Broader than it is long, the prostate measures approximately 4 × 3 × 2 cm. Its base is fused with the bladder neck and perforated by the urethra, which traverses the length of the prostate to emerge at its apex. The prostate’s inferolateral surfaces are cradled by levator ani. Posteriorly the prostate is pierced by the ejaculatory ducts, which pass through the gland to open into the prostatic urethra ( Figure 29.1 ).
Histopathological analysis of the prostate reveals four distinct regions or zones, which center on different areas of ejaculatory ducts ( Figure 29.2 ).
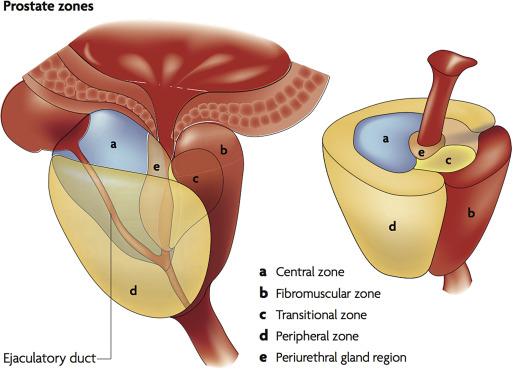
The peripheral zone (PZ) forms the bulk of the glandular prostate (70%) and arises from duct buds that develop laterally into the mesenchyme posterior to the distal urethral segment. This region is the most common site of origin for prostate carcinoma (70% cancers). Peripheral zone tumors of 0.2 mL or larger may be detected by digital rectal exam (DRE). Although the sensitivity and specificity of DRE is limited, an abnormal DRE is associated with an increased risk of a higher Gleason score and should therefore be considered an indication for prostate biopsy even if PSA is normal.
The smaller central zone (25% of the normal glandular prostate) arises from ducts clustered in a small area on the convexity of the verumontanum, immediately surrounding the ejaculatory duct orifices. These ducts branch proximally and laterally toward the prostatic base. This zone is relatively immune to cancer, but can be susceptible to tumor infiltration from adjacent zones. In autopsy and surgical specimen studies, central zone cancers account for up to 10% of prostate cancer. Although uncommon, cancers that do arise in this zone may be more aggressive.
The transition zone (TZ) arises from ducts in the proximal urethra. It accounts for less than 5% of the normal prostate gland, but can enlarge considerably in BPH. The TZ is easily recognizable on ultrasound examination, as it is diffusely hypoechoic relative to the PZ. TZ cancer is the site of origin of up to 25% of prostate cancer. Cancers from this zone show much less capsular penetration and seminal vesicle invasion than PZ cancers of comparable volume, as the TZ boundary provides a barrier to cancer spread through the PZ. When performing TRUS biopsies, separate transition zone biopsies give a very low detection rate and therefore may be omitted from the standard biopsy template at initial biopsy.
The anterior fibromuscular stroma produces the characteristic convexity of the anterior prostatic surface. It is a thick, nonglandular region that accounts for one-third of the bulk of the prostate. It is continuous with detrusor muscle proximally and the external urethral sphincter distally.
The seminal vesicles (SV) are paired thin-walled lobulated sacs that are applied to the posterior aspect of the bladder base, lateral to the ampulla of the ductus deferens. At their lower end the duct of the seminal vesicle joins the ductus deferens to form the ejaculatory duct, which opens into the prostatic urethra at the verumontanum. The tip of the SV has a close relationship to the arterial supply to the bladder base and the proximal neurovascular bundle. Frequency and extent of SV invasion correlates strongly with cancer volume. Due to the association of SV invasion and poor prognosis, radical prostatectomy routinely involves en bloc resection of the seminal vesicles.
A thorough understanding of the fasciae investing the prostate, rectum, and muscles of the pelvis is imperative to the performance of nerve-sparing surgery. Histological studies and the advent of intraoperative magnified vision have enabled an improved appreciation of the complexity of the multilayered fascia around the prostate ( Figure 29.3 ). However, the exact anatomy of these fascial layers remains controversial. In addition, the use of different terminology contributes to confusion in this area.
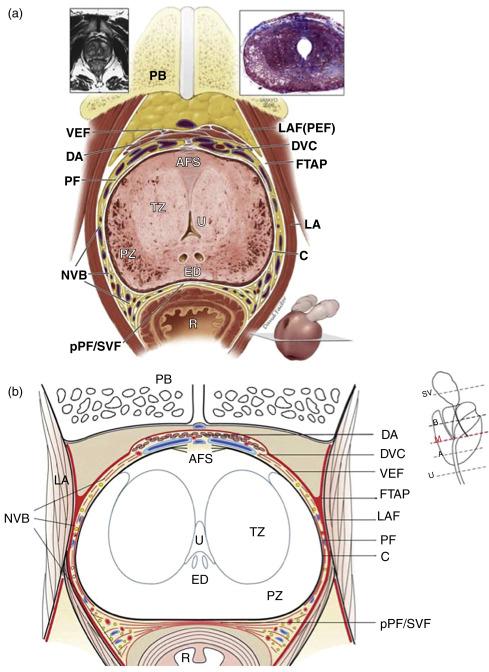
The “prostatic capsule” is not a true capsule by definition, but an incomplete outer fibromuscular band that is an inseparable part of the prostatic stroma. It represents the outermost aspect of the prostate gland and provides an important landmark in the pathological classification of the extent of prostate cancer involvement. Anteriorly, the capsule is not clearly evident, and is difficult to distinguish from the anterior fibromuscular stroma of the prostate. The capsule is also deficient at the prostatic base and apex where the prostatic stroma merges with the detrusor muscle and urethral sphincter fibers, respectively.
( Pelvic fascia, Lateral pelvic fascia, superior pelvic fascia, parietal pelvic fascia, levator fascia, outer layer of periprostatic fascia, parapelvic fascia )
The pelvic fascia comprises parietal and visceral fascia that line the walls and floor of the pelvis. This is often described collectively in prostate surgery as the endopelvic fascia. The parietal endopelvic fascia is continuous with transversalis fascia and provides cover to the pelvic muscles lateral to the fascial tendinous arch. The visceral endopelvic fascia sweeps medially from the tendinous arch, to cover the bladder and anterior prostate investing the pelvic organs and perineural and vascular sheaths.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here