Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
For optimal interpretation of imaging studies done after thoracic surgery, it is essential to understand the surgical techniques and the possible complications. The common surgical procedures that are performed in the lung, pleura, mediastinum, and chest wall are discussed in this chapter.
Almost all thoracic surgical procedures in the past have been performed via open lung approach, requiring either sternotomy or thoracotomy to gain access to intrathoracic structures. Sternotomy could be either partial or complete, depending on the procedure and the access required. Thoracotomy consists of division of one of major muscles groups in the chest wall and entering a hemithorax cavity through an intercostal space. Spreading of the intercostal space to gain a wider access window occasionally requires an additional partial rib resection or may cause rib fracture. Minimally invasive thoracic surgery, mainly referred to as video-assisted thoracoscopic surgery (VATS), has recently replaced the open lung approach for almost all indications, except lung transplant and pneumonectomy. VATS requires three to four entrance ports through which a videothorascope and trocars are introduced, thereby decreasing the risk for wound or incisional complications. Furthermore, VATS is better tolerated than open lung surgery because of reduced length of the hospital stay and marked decrease in the degree and duration of postoperative pain.
Wedge resection is a type of lung surgery during which a small nonanatomic portion of lung is excised. Pulmonary vessels, bronchus, and lymphatics in the affected segment are usually preserved. Common indications for this type of surgery are lung biopsy for diffuse lung disease, excisional biopsy of indeterminate lesions, and resection of single or multiple metastases. More rarely, wedge resection is used as a salvage procedure for primary lung carcinoma in patients who cannot tolerate larger anatomic lung resection. As well, sublobar resection may sometimes be the preferred resection for peripheral small minimally invasive cancer. A dense linear opacity representing a surgical staple line is typically visualized at the site of resection on postoperative radiographs. An associated small parenchymal hematoma usually develops during the early postoperative period and is characterized as a focal airspace opacity surrounding the staple line ( Fig. 12.1 ) that gradually resolves in the following days or weeks. Small amounts of adjacent atelectatic lung and mild parenchymal distortion can additionally be present and are best appreciated on computed tomography (CT).
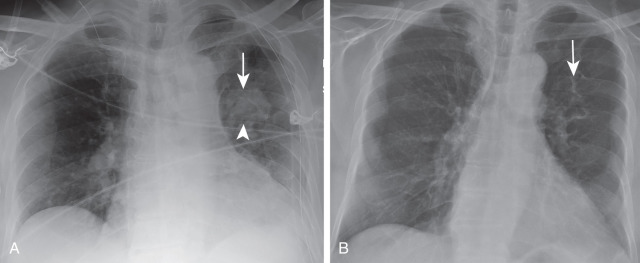
Blebectomy consists of resection of apical blebs. This procedure is usually performed in the context of recurrent pneumothorax and sometimes may be followed by mechanical pleurodesis. Bullectomy, or excision of a single bulla or multiple large bullae, is performed when bullae are causing atelectasis of adjacent lung parenchyma. The resection of these bullae favors reexpansion of the atelectatic lung and improvement in the patient's respiratory function. The radiologic findings after bullectomy and blebectomy are subtle. In fact, if normal lung parenchyma fully reexpands after the surgery, signs of these surgical procedures may only be the absence of bullae or blebs that were documented on preoperative imaging and possibly surgical staple lines ( Fig. 12.2 ).
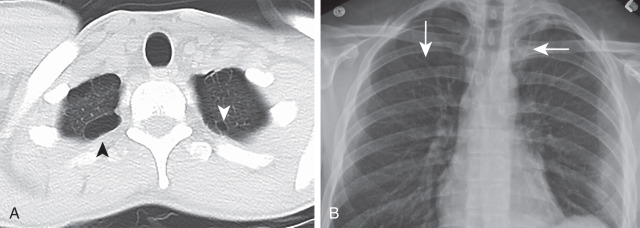
Lung volume reduction surgery has traditionally been used for treatment of severe emphysema. Nonanatomic resection of lung parenchyma most severely affected by emphysema has been shown to improve patients' respiratory status and quality of life, particularly if upper lobes are diseased. This type of surgery is often considered when medical therapy fails to improve symptoms. Volume reduction surgery may also be performed in the context of lung transplant in which donor lungs are reduced in size to fit in the recipient's chest. Long surgical staple lines are typically the only findings appreciated on radiographs. CT scan additionally demonstrates adjacent parenchymal distortion and smaller-than-usual size of the lobe that underwent reduction.
Segmentectomy is a type of anatomic lung surgery defined by the resection of one or several segments of a pulmonary lobe. Examples of surgeries involving resection of more than one segment are basal segmentectomy (all basal segments of a lower lobe, sparing the superior segment), lingulectomy (lingular inferior and superior segments), and upper division left upper lobectomy (LUL) (anterior and apicoposterior segments of LUL, sparing lingular segments). Accompanying draining lymph nodes are dissected with the segment(s) as well. This surgery can be used for resection of lung cancers if lobectomy cannot be tolerated by a patient because of poor lung function. Additional indications include excision of metastasis, benign tumors, and focal parenchymal processes (e.g., bronchiectasis). The postoperative appearance is characterized by a smaller-than-expected size of the affected lobe. The lobar bronchus remains patent, but the segmental bronchus is resected. A surgical staple line may or may not be visualized, depending on whether staples or sutures were used during surgery.
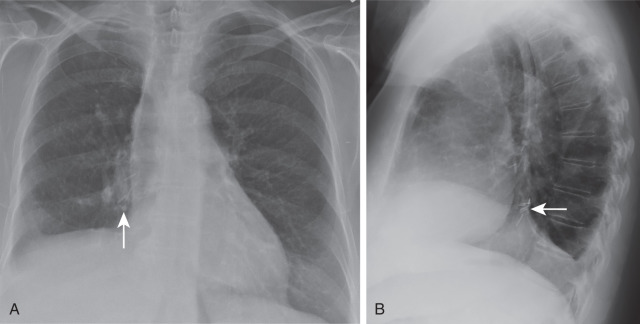
Lobectomy is considered as a definitive surgical procedure for most lung cancers. It implies resection of one (or more) lobes along with regional lymph nodes. In addition to lung cancers, some benign processes (e.g., severe bronchiectasis) and congenital anomalies (e.g., congenital pulmonary airway malformation) are indications for a lobectomy. Sleeve lobectomy is a type of lobectomy during which a diseased lobe, corresponding lobar bronchus, and segment of the mainstem bronchus are resected en bloc. The remaining lobar bronchus is subsequently connected to the residual portion of the main bronchus in end-to-end fashion. This surgery is usually performed as a lung-sparing procedure for central lung cancers invading the main bronchus as an alternative to pneumonectomy. Radiographic findings of lobectomy are similar to those of total lobar collapse. In both processes, there are volume loss of the affected lung, displacement of the hila, shift of the mediastinal structures, and elevation of the ipsilateral hemidiaphragm. Some findings, however, are characteristic of lobectomy. In particular, the presence of surgical clips in the hilar region and postthoracotomy changes (if open lung surgery was performed) confirm prior surgical resection ( Fig. 12.3 ). The absence of the fissure in the left lung and characteristic reorientation of fissures in the right lung after lobectomy is another finding differentiating lobectomy from lobar collapse and is easily seen on CT. Occasionally, a surgeon may decide to use an additional vascularized tissue to reinforce the bronchial stump and prompt its healing. This usually is achieved by additional blood supply to the stump from muscle flaps (intercostal, latissimus dorsi, or pectoralis) or fat flaps (omentum, pericardial fat pad). On postoperative radiographs, the ipsilateral hilum appears larger than expected. Additionally, a large triangular opacity extending from the hilum to the chest wall can be seen if a muscle flap was used ( Fig. 12.4 ). CT scans demonstrate soft tissue and fat density material in the region of bronchial stump tracking to the chest wall. It should be noted that these radiologic findings are present from the first postoperative radiograph and usually do not subsequently change in appearance. In contrast, progressive enlargement of the ipsilateral hilum and formation of new soft tissue density in the region of the stump in a later postoperative stage should raise a strong suspicion of local tumor recurrence.
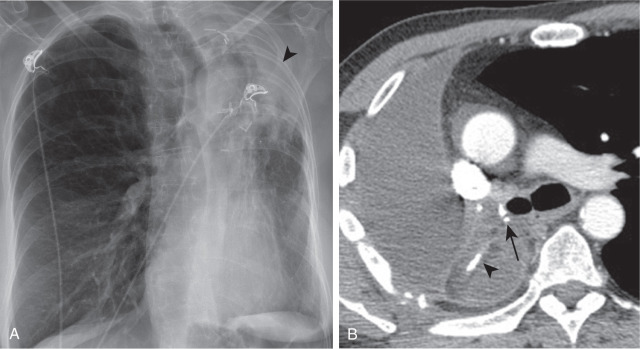
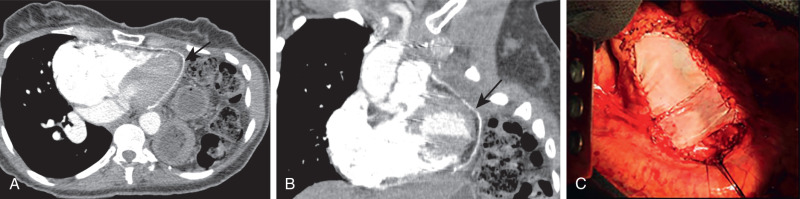
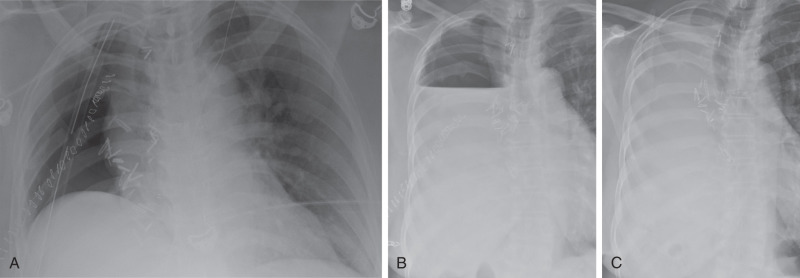
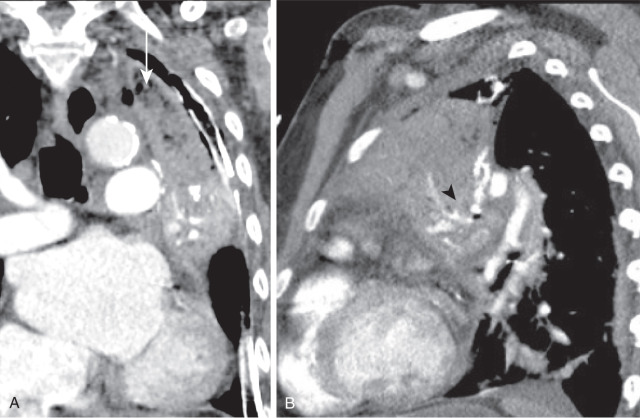
Surgical removal of an entire lung is indicated for lung cancers that invade central structures, such as the mainstem bronchus and main pulmonary artery, and those that extend through fissures. Given its higher rate of morbidity and mortality than lesser anatomic resections, a pneumonectomy is usually performed as a last resort. It is the only surgical lung resection that is not routinely performed with VATS. There are three types of pneumonectomies: classic, intrapericardial, and extrapleural. The classic pneumonectomy consists of resection of a lung and corresponding hilar lymph nodes. Tumor invasion of pericardium or intrapericardial portions of pulmonary artery or veins is an indication for intrapericardial pneumonectomy. This type of pneumonectomy implies resection or ligation of intrapericardial portions of pulmonary artery, vein, or both in addition to excision of affected lung. When a partial resection of pericardium is performed, it is followed by pericardial reconstruction with a mesh ( Fig. 12.5 ). After pneumonectomy, the earliest postoperative radiographs demonstrate predominantly air-filled pneumonectomy space with midline position of mediastinal structures. After the chest tube is clamped or removed, the air is gradually reabsorbed, and fluid fills the pneumonectomy space. This is manifested by cranial displacement of the air–fluid level, usually two intercostal spaces per day. After the air is entirely reabsorbed over days to weeks, radiographs demonstrate characteristic opacification of the entire hemithorax, which is typically attributable to a combination of fluid and shifted mediastinal structures ( Fig. 12.6 ). Eventually, some of the fluid gets reabsorbed as well, causing mediastinal structures to shift even more into ipsilateral hemithorax. The amount and rate of fluid reabsorption are variable and may take weeks to months. More often than not, some fluid chronically persists within the pneumonectomy space with a smooth peripheral margin and concave margin toward the hilum, best appreciated on CT scan (see Fig. 12.4 ). High-density mesh (either bovine or polytetrafluoroethylene in nature) can be appreciated at the site of pericardial and diaphragmatic reconstruction if resection was performed during the surgery. In the immediate postoperative period, pulmonary edema may be seen in the residual lung, more commonly in the left lung after right pneumonectomy ( Fig. 12.7 ).

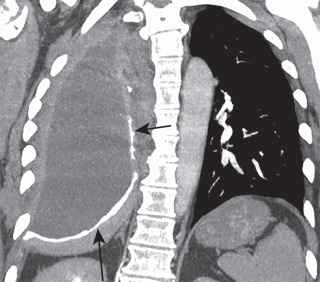
Extrapleural pneumonectomy is performed in selected patients with malignant mesothelioma. It requires resection of lung, parietal pleura, involved portions of pericardium, and ipsilateral hemidiaphragm. Pericardial and diaphragmatic defects are subsequently closed with synthetic graft and mesh. Findings on postoperative radiographs are similar to those after classic pneumonectomy. CT additionally demonstrates a curvilinear hyperdensity extending from the chest wall medially toward the midline and a round or oval hyperdensity overlying the heart, representing reconstructed hemidiaphragm and pericardial mesh, respectively ( Fig. 12.8 ). Almost all complications after classic pneumonectomy may also happen after extrapleural pneumonectomy.
Small pneumothorax is an expected early finding after a lung resection. It invariably resolves with an indwelling chest tube inserted at the time of the surgery. Pneumothorax that persists despite a chest tube for longer than 7 to 10 days suggests an air leak.
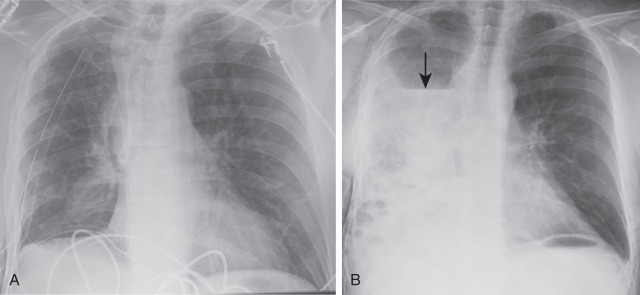
Connection between the pleural space and larger bronchus is defined as bronchopleural fistula (BPF). The incidence of this complication ranges from 0.4% to 3%. Central BPF is commonly caused by dehiscence of sutures and staples or necrosis at the level of the bronchial stump. After pneumonectomy, this commonly occurs in the early postoperative period (within the first 2 weeks). The risk factors for the development of BPF include preoperative infection, radiation, right pneumonectomy, residual tumor at the stump, a long stump, extensive mediastinal or hilar lymph node dissection, diabetes, and steroid use. Surgical reclosure is a preferred treatment in the absence of pleural infection because it minimizes the risk of possible complications, such as empyema, acute respiratory distress syndrome (ARDS), and aspiration of the pleural fluid into the contralateral lung. If not already performed at the time of initial resection, a vascularized flap is used to cover the stump to promote adequate vascular supply and promote healing. The radiographic appearance of BPF varies depending on the size of the fistula. New or an increasing amount of air in the ipsilateral pleural space is a typical presentation ( Fig. 12.9 ). If a large amount of air develops in the pleural space in the context of large BPF, it can sporadically result in a tension pneumothorax. Characteristic radiographic findings of BPF after pneumonectomy consist of increased air in the pneumonectomy space with caudal drop of more than 2 cm of preexisting air–fluid level, failure of fluid to fill the pneumonectomy space, reoccurrence of air in the previously opacified hemithorax, and contralateral shift of the mediastinal structures. In addition to these radiographic findings, CT scans may directly demonstrate a connection between the pleural space and the airway.
Postoperative lobar torsion is a rare complication after thoracic surgery. It is most frequently seen after lobectomy, although it can occur after sublobar resection, severance of pleural adhesions, and parietal pleurectomy. Although any lobe can be affected, torsion of the right middle lobe is the most commonly seen, usually after right upper lobectomy. Lobar torsion can be partial or complete, depending on the degree of rotation of its vascular pedicle. Predisposing factors include the presence of complete fissures, long slender hilar pedicle, absence of postoperative adhesions, and complete division of the inferior pulmonary ligament during upper lobectomy. Urgent surgical reduction of torsion is required to prevent venous congestion, occlusion of the arterial supply, infarction, and gangrene of the affected lobe. Radiographic findings of a lobar torsion are subtle and nonspecific. Consolidated lobe in an unusual position and change in position of an opacified lobe on serial radiographs may be seen on early postoperative radiographs. CT is much more sensitive in detection of an ongoing lobar torsion, particularly given its ability to create multiplanar reformats. The CT appearance of the torsed lung parenchyma depends on the duration and degree of torsion. It typically consists of a combination of ground-glass opacity; interlobular septal thickening in early stages; and lack of enhancement, consolidation, and necrosis as it progresses ( Fig. 12.10 ). Moreover, CT may additionally demonstrate bronchial cut-off, tapered occlusion or distortion of the proximal pulmonary artery and vein, and abnormal orientation of the fissures.
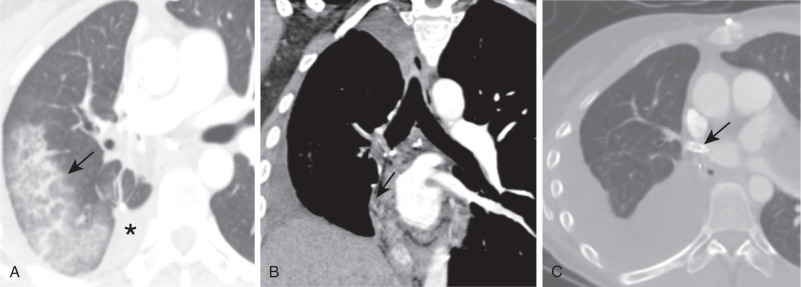
Pulmonary venous infarct is a rare complication after thoracic surgery, predominantly seen after lobectomy. It happens because of pulmonary vein thrombosis, compression, or unintended ligation during surgery. Hemoptysis is a common presenting symptom. Timely diagnosis is essential to preserve the viability of the rest of the lung parenchyma. Therapeutic options consist of antibiotics, angioplasty, stent insertion, and resection of the affected lobe. Radiologic findings depend on the stage of venous infarct: early hemorrhagic and late fibrotic stages. Radiographic findings of the hemorrhagic stage initially are manifestations of increased pressure in pulmonary veins and capillaries, which are radiographically manifested by reticular opacities with or without enlarged pulmonary veins in the portion of the lung drained by the affected veins. Afterward, patchy irregular opacities predominate, which are signs of parenchymal hemorrhage. On CT, a venous infarct typically demonstrates interlobular septal thickening, ground-glass opacities located septally near venules, and scattered airspace opacities, consistent with areas of hemorrhage and infarct ( Fig. 12.11 ). Furthermore, visceral pleura of the implicated lung may be thickened because of venous collaterals. Late fibrotic phase demonstrates characteristic findings of parenchymal fibrosis, consisting of intralobular and interlobular septal thickening, honeycombing, and parenchymal distortion. By demonstrating the exact level of venous occlusion, CT, magnetic resonance imaging, and pulmonary angiography with delayed venous phase are useful for confirmation of diagnosis and for treatment planning.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here