Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The posterior mediastinum is an anatomically diverse region that includes visceral organs, major vascular structures, large neural structures, and important lymphatic vessels. Lesions that originate in the mediastinum are relatively rare compared with the diverse pathology that can involve the mediastinum secondarily, although metastatic disease appearing in the posterior mediastinum, excluding the spine, is unusual. The most common lesions arising within the posterior mediastinum are primarily tumors of neurogenic origin. Less common is a potpourri of lesions including vascular tumors, mesenchymal tumors, and lymphatic lesions.
The posterior mediastinum, also called the paravertebral compartment, is a defined space between the posterior pericardium and the anterior spinal ligament including the paravertebral gutters. According to the traditional four-compartment model, the mediastinum is divided into anterior, middle, posterior, and superior compartments. The posterior mediastinum is bounded superiorly by the inferior border of the T4 vertebral body.
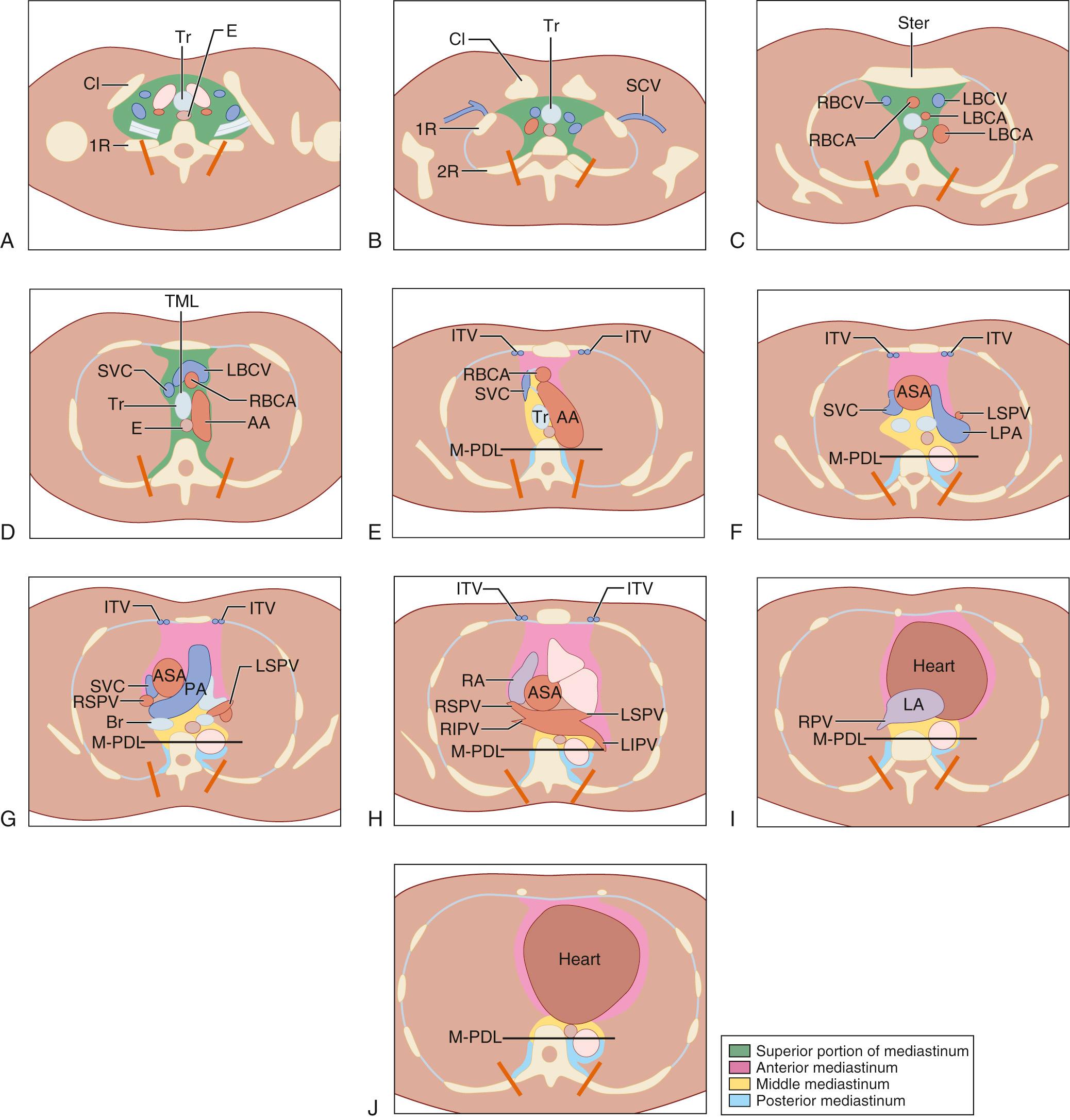
In the traditional three-compartment model without a superior division, the entire length of the spine is included in the posterior mediastinum. The diaphragm is the common inferior border for all three compartments. Within these boundaries, the posterior mediastinum contains the esophagus, descending aorta, sympathetic chain and vagus nerves, thoracic duct, azygos and hemiazygos veins, fat, and lymph nodes ( Fig. 43-1 ). Recently, Fujimoto and colleagues proposed a new mediastinal compartment classification based on transverse axial computed tomographic (CT) imaging. Because of the routine use of CT scanning in the diagnosis and management of these lesions this classification appears to be more user-friendly and clinically applicable. The authors proposed the division of the mediastinum into four compartments that are visible on CT axial images: superior portion, anterior mediastinum (prevascular zone), middle mediastinum (peri-tracheoesophageal zone), and posterior mediastinum (paravertebral zone). The authors validated their classification by retrospectively analyzing 445 pathologically proven mediastinal tumors ( Fig. 43-2 ).
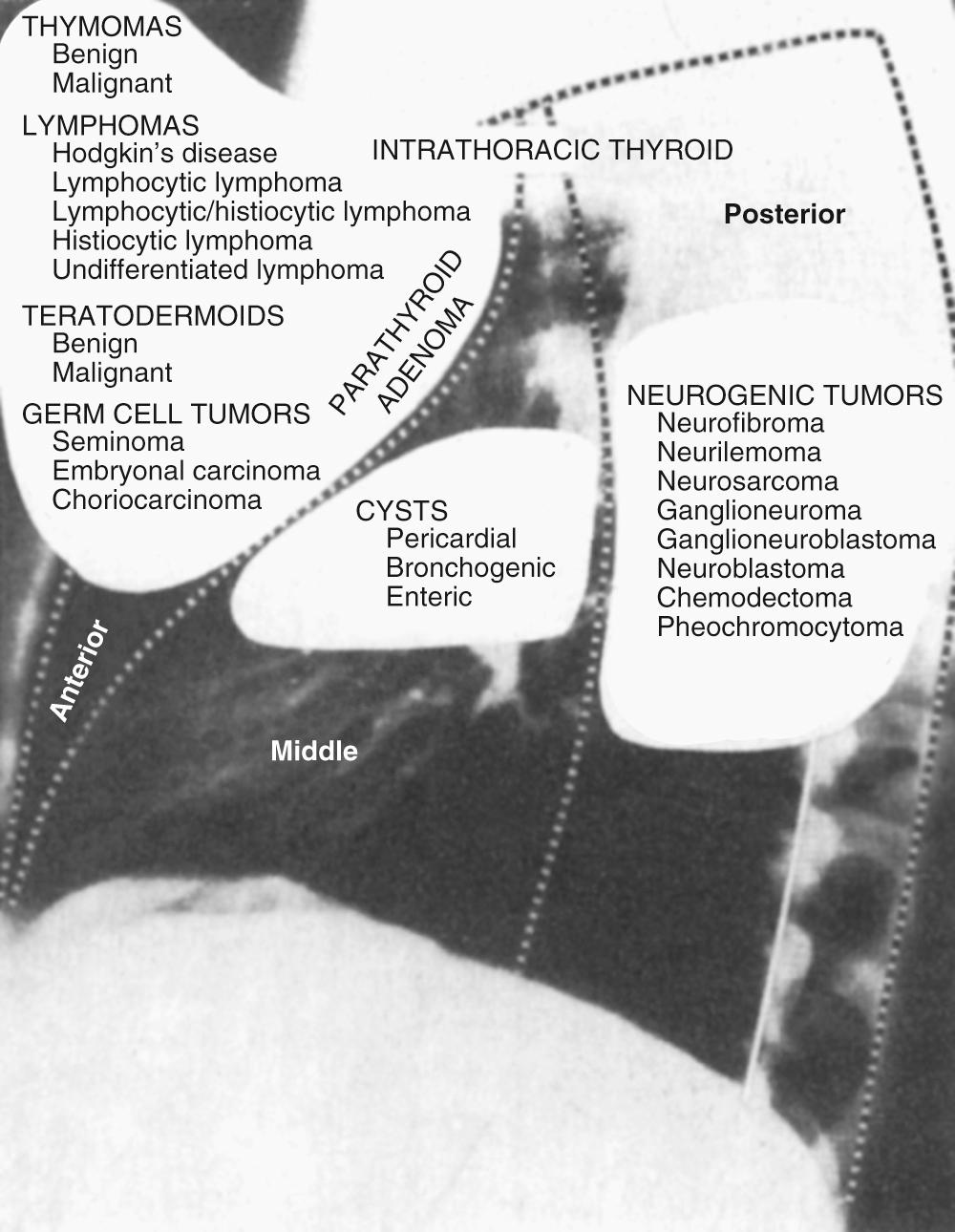
Significant differences exist between children and adults with respect to the location of mediastinal masses. In adults, 65% of the lesions arise in the anterosuperior, 10% in the middle, and 25% in the posterior compartments; this distribution is reversed in children, in whom 25% of lesions arise in the anterosuperior, 10% in the middle, and 65% in the posterior compartments. In general, the incidence of posterior mediastinal lesions is higher in children, whereas anterior lesions predominate in adults.
Approximately 50% of posterior mediastinal lesions are asymptomatic and are detected on chest radiographs or CT scans taken for unrelated reasons. As a rough guideline, the absence of symptoms is more commonly associated with a lesion that likely is benign, whereas the presence of symptoms suggests malignancy. The percentage of patients with symptoms arising from a mediastinal mass precisely parallels or equals the incidence of malignant lesions. In adults, 50% to 60% of lesions are symptomatic, whereas the percentage of symptomatic lesions is higher in children, ranging from 60% to 80%. Because the incidence of symptoms parallels the incidence of malignant lesions, a child with a mediastinal mass is considerably more likely to have a malignant neoplasm than is an adult with a mediastinal mass. When a posterior mediastinal mass is discovered, a detailed history and physical examination should be obtained, looking particularly for signs such as hoarseness or Horner syndrome. The age of the patient also significantly narrows the diagnostic possibilities.
Computed tomography (CT) is the imaging modality of choice for the posterior mediastinum because of its ability to visualize a mass on an axial cut and to provide some idea as to the extent of invasion, although distinguishing abutment from invasion remains difficult. CT often can distinguish among the various lesions and identify the origin, allowing a correct diagnosis often based strictly on radiographic imaging. Magnetic resonance imaging (MRI) has been useful in certain circumstances, specifically with dumbbell tumors to assess the presence and extent of invasion within the spinal canal, but also for cysts, and extramedullary hematopoiesis. CT scanning, however, remains the better imaging modality for most posterior mediastinal masses. Mediastinal sonography, although less expensive and comparable to CT in the diagnosis of many mediastinal masses, is not useful in the posterior mediastinum.
The decision to sample a mediastinal mass is not straightforward. Obtaining a biopsy before proceeding with resection is not necessary in some cases and potentially harmful in others. The likelihood of a positive finding in a biopsy specimen depends on the presence of local symptoms in addition to the location and extent of the lesion. Lesions in the posterior mediastinum require either fine-needle aspiration (CT guided) or a thoracoscopic approach. If these procedures are not possible because of location in the paravertebral gutters, a limited posterolateral thoracotomy should be used to obtain adequate tissue for diagnosis or, alternatively, simply to resect the lesion in its entirety.
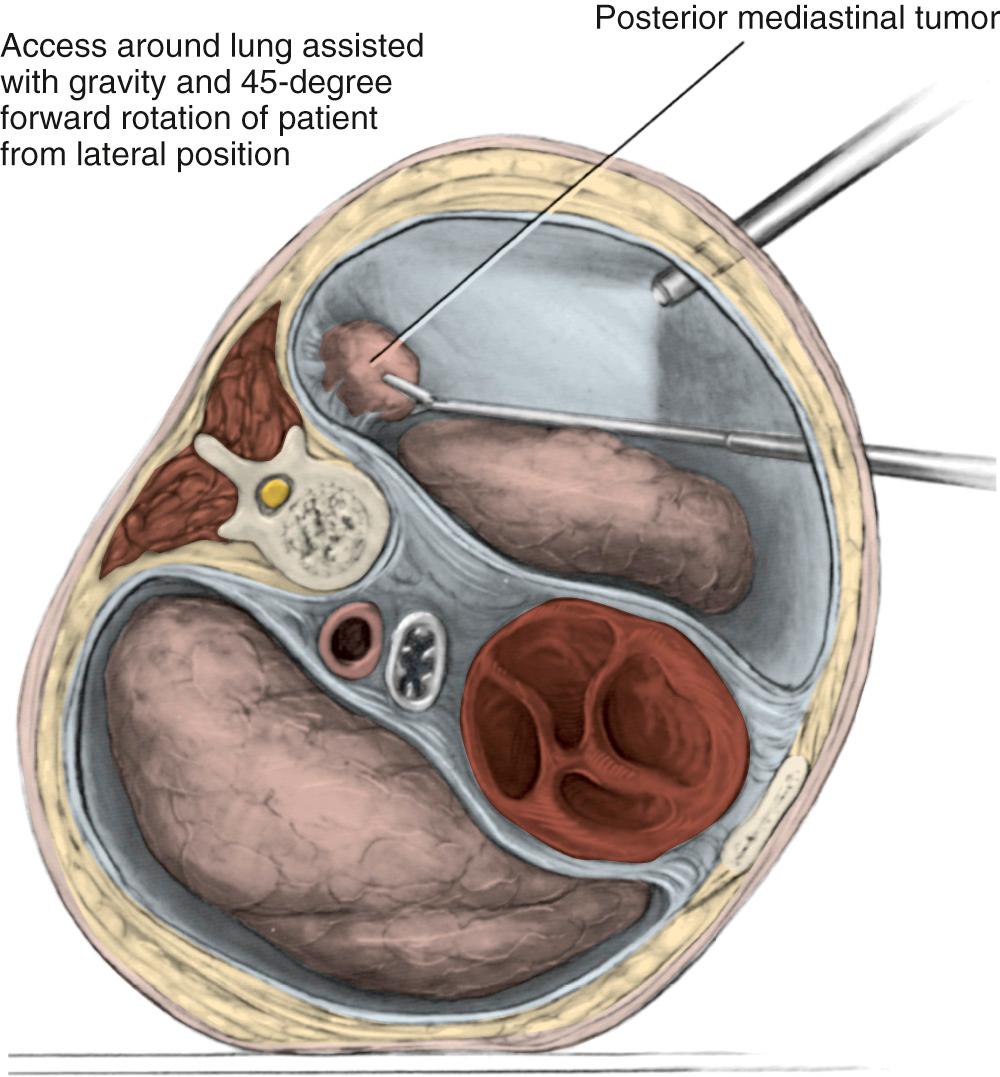
Multiple standard approaches have been described to access the posterior mediastinum depending upon the location relative to the particular aspect of the spine. These include an anterior transcervical approach, a posterior paravertebral approach, posterolateral thoracotomy or video-assisted thoracoscopy or via a transabdominal incision ( Fig. 43-3 ).
The transcervical approach is accomplished through an incision along the anterior border of the sternocleidomastoid muscle. The region that is most difficult to access is at the level of the T1 vertebral body, because transthoracic and transcervical approaches are not ideal. For a lesion at this location, an extension of the incision along the anterior border of the sternocleidomastoid muscles down to the manubrium and then out along the infraclavicular region allows the manubrium to be divided and retracted upward, giving access to the region of the T1 vertebral body. We have used this approach for a number of lesions with great success. Di Rienzo and colleagues have described a modified transmanubrial osteomuscular sparing approach for resection of lesions between C7 and T2, recognizing that either a right-sided or left-sided approach can be used because the vascular dissection is similar on both sides.
When more inferior posterior mediastinal masses need to be accessed, the paravertebral approach can be used by resecting posterior segments of one or more ribs and entering the retropleural plane that leads to the posterior mediastinum. Standard posterolateral thoracotomy, the most commonly used approach, provides excellent access to the posterior mediastinum; the location of the lesion determines the intercostal space to be entered.
The posterior mediastinum can also be accessed transabdominally through the esophageal hiatus, important in various antireflux procedures or hiatal hernia repairs, and for mobilization of the mediastinal esophagus when performing a transhiatal esophagectomy. A combined cervical approach with transabdominal mobilization allows for the removal of the esophagus extrapleurally ideally without entering either the right or left pleural reflection. A transabdominal approach at the level of the hiatus also allows access to the cisterna chili, which may need to be ligated when dealing with a chylothorax when ligation of the thoracic duct in the chest has been unsuccessful.
Currently it is the preference of most surgeons to access lesions of the posterior mediastinum using a video-assisted thoracic surgical (VATS) approach, but this depends on the surgeon's experience and comfort with video-assisted procedures. If the intent is strictly to secure material for histologic study, then VATS clearly should be the procedure of choice. Zierold and Halow conducted a retrospective review that described the use of a VATS approach for posterior mediastinal neurogenic lesions. Twenty-nine patients (13 men, 16 women; 26 to 68 years old) who underwent a thoracoscopic resection were identified. Preoperative imaging included chest radiography and CT in all patients and MRI in 15 of 29 patients (52%). All tumors were located in the posterior mediastinum and in none was there preoperative evidence of invasion or malignancy. Conversion to an open procedure was required in 12 of 29 (41%) patients (mini-thoracotomy in 11, posterolateral thoracotomy in 1). Tumor size necessitating conversion to an open procedure (mean = 4.79 cm) and tumor size amenable to thoracoscopy alone (mean = 3.84 cm) were not significantly different ( P < 0.09). They concluded that thoracoscopic resection could be performed successfully, regardless of tumor type or size; however, malignant lesions, local invasion, and tumors larger than 5 cm may require an open procedure. Cardillo and associates detailed their experience with 93 patients who underwent resection of a posterior mediastinal neurogenic tumor. The tumor was resected with a videothoracoscopic approach in 57 patients; 44 underwent VATS only, and 13 required conversion to an open approach. Mean operative time was significantly shorter in the VATS group, as was the median postoperative hospital stay and postoperative pain. No recurrences were noted at a mean follow-up of 73 months.
More recently, robotic surgery has been used for the resection of mediastinal lesions, including those in the posterior mediastinum. Melfi and colleagues recently reported on a 10-year experience of mediastinal robotic surgery in a single referral center. Sixty-nine patients were resected using the da Vinci robotic system, including 13 paravertebral neurogenic tumors. Patients were positioned in the lateral decubitus position, and the robotic arms were located based on the site of the lesion generally at the fourth intercostal space. Lesions were removed through the anterior port, where the intercostal space is widest, and the largest incision used was 3 cm. No additional utility incision was performed. The authors noted significant progression on the learning curve, especially related to the resection of anterior mediastinal lesions where the mean operative time between the first 10 resections and the second 10 decreased significantly from a mean of 194 minutes to 97.5 minutes. The authors confirmed the safety and feasibility of the robotic approach for different mediastinal lesions, but they point out that cost may be an important limitation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here