Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The peripheral veins may be affected by a variety of disorders which can be assessed by ultrasound. Deep vein thrombosis (DVT) and thromboembolic disease are the most common indications for investigation of the peripheral veins but venous insufficiency and vein mapping are also reasons for examining the veins. Anderson et al. found an average annual incidence of 48 initial cases, 36 recurrent cases of DVT and 23 cases of pulmonary embolus per 100 000 population in the Worcester DVT study. The prevalence of varicose veins and chronic venous insufficiency is more difficult to quantify, but it has been estimated that 10–15% of males and 20–25% of females in an unselected Western population over 15 years of age have visible tortuous varicose veins; 2–5% of adult males and 3–7% of females have evidence of moderate or severe chronic venous insufficiency, with a point prevalence for active ulceration of 0.1–0.2%.
The indications for ultrasound of the venous system are shown in Box 5-1 . The most frequent indication for ultrasound of the veins is for the investigation of possible DVT in the lower limb and, occasionally, in the upper limb – especially if there have been central venous catheters inserted for intensive care monitoring, chemotherapy, dialysis or parenteral feeding. Similarly, indwelling femoral catheters are prone to induce thrombosis and patients should be examined early if this is suspected. Ultrasound provides a non-invasive, reliable method for examining the venous system, particularly with respect to the diagnosis, or exclusion, of dangerous proximal thrombus in symptomatic patients. The results for asymptomatic thrombus in the lower limbs are less encouraging and this should be recognised when using ultrasound to screen for DVT in asymptomatic patients.
Diagnosis or exclusion of deep vein thrombosis in the upper or lower limb, spontaneous or related to indwelling catheters
Assessment of secondary/recurrent varicose veins
Investigation of chronic venous insufficiency and postphlebitis syndrome
Vein mapping prior to bypass grafts
Assessment of primary varicose veins if there is uncertainty following clinical examination
Localisation of veins for cannulation
Recurrence of varicose veins following surgery can pose many problems for the clinician trying to clarify the venous anatomy. Colour Doppler can be used instead of venography and varicography in most cases and may be the only examination required to define the anatomy and function in patients with recurrent varicose veins.
The impact of postphlebitis syndromes and chronic venous insufficiency is a rather larger problem than is apparent from its relatively low clinical profile. In one large epidemiological study of 4376 subjects, 62% had some evidence of varicose veins; signs of chronic insufficiency were present in 22%. Varicography shows perforator veins which are obviously incompetent and some incompetent superficial and deep venous segments, but ultrasound has the advantage that the segments of the deep and superficial systems can be examined and the direction of blood flow within each segment can be demonstrated. In addition, it is less unpleasant for the patient and allows multiple assessments to be performed without discomfort. The main disadvantage is that it is fairly time-consuming, particularly in complex cases, and requires a significant degree of expertise in order to perform examinations efficiently.
The superficial veins of the legs and, occasionally, the arms may be used for bypass grafts for the coronary or lower limb arteries. If there is any doubt about their suitability as a conduit following previous varicose vein surgery, or in terms of their calibre, ultrasound can be used to assess the diameter and length of vein available. In addition, the sonographer can map out the course of the vein to allow easier harvesting.
It may be difficult occasionally to locate a suitable vein for central venous cannulation, particularly in patients who have had multiple previous central venous lines, such as intensive care or chemotherapy patients. Ultrasound can be used to clarify the location and patency of potentially suitable veins and, in difficult cases, the puncture may be made under direct ultrasound visualisation.
The anatomy of the venous system in the limbs is more complex and variable than that of the arteries. The components and nomenclature of the lower limb veins were reviewed by a consensus group in 2002 and their recommendations are used here. The meanings of the terms ‘proximal’ and ‘distal’ may cause confusion as the veins start at the periphery and blood flows centrally towards the heart so that ‘upstream’ is peripheral and ‘downstream’ is central, which is the opposite from the situation in the arteries. The convention is that proximal describes locations nearer the heart and distal refers to points further from the heart; these terms are used in this way in this chapter.
The veins of the lower limb are divided into deep and superficial systems. These are linked by a variable number of perforator veins which carry blood from the superficial to the deep systems ( Fig. 5-1 ).
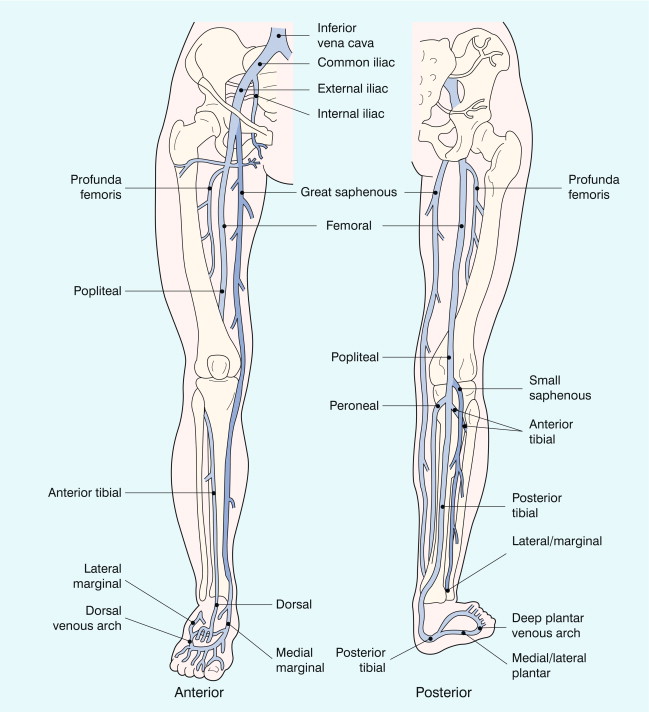
The anatomy of the lower limb veins is rather variable. Generally the veins accompany the arteries but their number may vary and the communications with other veins along the way can show a variety of patterns; however, a general arrangement is usually apparent. In the calf there are veins running with the main arteries: the posterior tibial, peroneal and anterior tibial veins; there are usually two, occasionally three veins with each artery ( Fig. 5-2 ). In addition there are veins draining the major muscle groups in the posterior calf. These are seen in the upper calf as they pass upwards to join the other deep veins in the lower popliteal region; the gastrocnemius and soleal veins are the largest of these. The gastrocnemius vein is the more superficial and may be mistaken for the small saphenous vein; clues to its true identity are that it is usually accompanied by the artery to the muscle and it can be followed distally down into the muscle rather than outwards to lie subcutaneously on the fascia around the calf, which is the position of the small saphenous vein.
The calf veins join to form the popliteal vein, or veins – there may be two, or sometimes three channels, especially if there is a dual superficial femoral vein. The popliteal vein runs up through the popliteal fossa, lying more posterior and usually medial to the artery. As well as the veins from the calf and calf muscles, it is joined by the small saphenous vein at the saphenopopliteal junction.
The popliteal vein becomes the femoral vein at the upper border of the popliteal fossa; rarely, the popliteal vein runs more deeply to join with the profunda femoris vein. The femoral vein passes through the femoral canal and runs up the medial aspect of the thigh, posterior to the femoral artery to join with the profunda femoris vein (which can alternatively be called the deep femoral vein) in the femoral triangle below the groin; the profunda femoris vein drains the thigh muscles. The confluence of the femoral and profunda femoris veins to form the common femoral vein is normally a little more caudal than the bifurcation of the common femoral artery into the femoral and profunda femoris arteries. The femoral vein may have significant segments of duplication ( Fig. 5-3 ) along its length in up to 25–30% of subjects, , these dual segments may have a variable relation to the artery, so that they may be overlooked unless care is taken in the examination of the thigh veins with both transverse and longitudinal views being obtained.
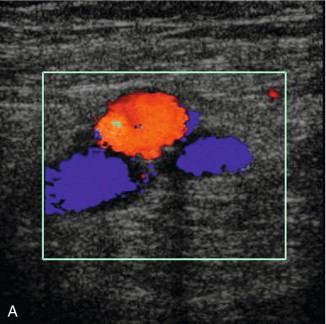
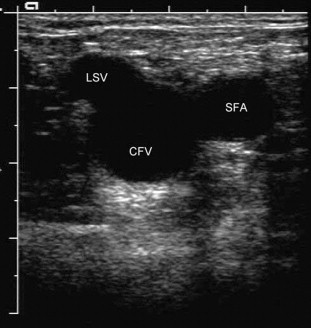
In the pelvis and groin, the anatomy is generally consistent. The femoral vein and profunda femoris vein join to form the common femoral vein, which lies medial to the common femoral artery. The common femoral vein is joined by the great saphenous vein at the saphenofemoral junction; the appearance of the common femoral vein, great saphenous vein and the common femoral artery in transverse section is sometimes referred to as the ‘Mickey Mouse’ view ( Fig. 5-4 ). The common femoral vein is also joined by veins from the muscles around the hip. These veins are variable in size and number, occasionally one of these is large enough to be confused with the great saphenous vein or profunda femoris vein but careful attention to the anatomy should clarify the situation. The common femoral vein becomes the external iliac vein after it has passed under the inguinal ligament, and then it passes posteriorly along the posterior pelvis, running alongside the external iliac artery. The internal iliac vein, which drains the pelvic structures, joins with the external iliac vein deep in the pelvis to form the common iliac vein ( Fig. 5-5 ). The two common iliac veins then join at the level of the aortic bifurcation to form the inferior vena cava, which normally passes cranially on the right side of the aorta. The left common iliac vein passes behind the right common iliac artery just distal to this confluence. In a small number of individuals this confluence does not occur and the two common iliac veins continue cranially as dual inferior venae cavae; this reflects the arrangement of paired cardinal veins in the embryo.
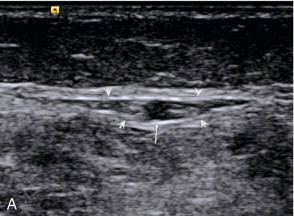
The deep veins have a series of valves along their course ( Fig. 5-6 ). These are somewhat variable in their number and location. They are most numerous in the veins below the knee; in the thigh, the femoral vein usually has one just below the confluence with the profunda femoris vein and at several levels below this. The iliac veins, in contrast, have relatively few valves; rarely a valve may be seen in the inferior vena cava.
The two main superficial venous channels in the lower limb are the great and small saphenous veins. The great saphenous vein arises from the medial aspect of the dorsal venous arch of the foot and passes in front of the medial malleolus to run up the medial aspect of the calf and knee into the thigh. In the upper thigh, the great saphenous vein curves laterally and deeply to join the common femoral vein just below the inguinal ligament. The great saphenous vein has two components in the calf: the posterior division passes up from the medial malleolus and communicates with the perforator veins; the anterior division usually joins the posterior division just below the level of the knee joint. Duplication of the great saphenous vein can be seen in the thigh in up to 50% of people, this usually takes the form of parallel channels. The great saphenous vein receives many superficial tributaries and is connected to the deep veins by perforating veins; some of these tributaries in the thigh can be quite prominent and may be mistaken for the main vein if their true nature is not recognised. In the region of the saphenofemoral junction the great saphenous vein receives several tributaries draining the groin, lower abdominal wall and perineum. These veins are of significance in the recurrence of varicose veins following high ligation, as they provide a network of collateral channels which may bypass the resected segment.
The small saphenous vein arises from the lateral aspect of the dorsal venous arch of the foot, passing below and behind the lateral malleolus to run up the posterolateral aspect of the calf to the popliteal fossa, where it passes through the deep fascia to join the popliteal vein. Classically, it enters the lateral aspect of the popliteal vein at the level of the popliteal skin crease, or within a few centimetres above this but the level of the confluence can be quite variable. It can be distinguished from the posterior muscle venous sinuses as it does not have an accompanying artery and it is seen to lie within the fascial triangle in the posterior thigh defined by the deep muscular fascia and the superficial fascia ( Fig. 5-7 ). Occasionally there is a thigh extension of the small saphenous vein, passing upwards to join the profunda femoris vein in the lower thigh – a Giacomini vein. Burihan and Baptista-Silva dissected 200 adult cadaver legs and reported 20 different patterns of termination of the small saphenous vein. In 27.5% of legs the small saphenous vein terminated in the principal deep vein of the leg (popliteal or lower femoral vein), in 25% of legs the small saphenous vein, or a branch arising from it, communicated with the great saphenous vein. In the remaining legs, there was a wide variety and combination of communications with other veins, including the deep femoral vein, the mid-thigh perforator vein, muscular veins and even the inferior gluteal vein in three legs. Other studies have shown that Giacomini veins can be affected by varicose disease with reflux either upwards or downwards in the thigh to the greater and lesser saphenous veins respectively.
The perforating veins connect the superficial veins to the deep veins. They are numerous and very variable in both size and location. In the past, they were often known by eponymous designations but with the revised nomenclature they are now identified by their anatomical location – for example: medial, lateral, or anterior ankle perforator – full details are given in the consensus statement on venous nomenclature. They are normally less than 5 mm in diameter and blood flows inwards from the superficial to the deep systems.
The technique varies depending on the clinical indication. The most common indication is the diagnosis or exclusion of DVT in the lower limb. This section therefore concentrates on this aspect and variations in technique for other indications will be dealt with in subsequent sections ( Box 5-2 ). A 7–10 MHz linear transducer will normally provide sufficient penetration, although in large or oedematous thighs a lower frequency may be required. It is important to ensure that the system is set up for the slower velocities found in veins, rather than the significantly higher arterial velocities.
Patient sitting on couch/trolley: compression of common femoral vein, superficial femoral vein from groin to adductor canal
Colour Doppler with augmentation, examine common and superficial femoral veins
Patient decubitus, or with leg elevated: compression and Doppler examination of popliteal vein(s)
Patient sitting, if possible, with legs dependent: examine the calf veins with compression and colour Doppler
Patient supine: examine iliac veins if thrombus suspected in these
It is advantageous if there is a tilting couch available so that the patient can be moved from the horizontal to various degrees of head-up elevation as necessary. In the absence of a tilting couch it is better if the patient can be examined with the thorax higher than the legs, as this produces some distension of the lower limb veins, which makes them easier to identify and the assessment of compression more straightforward.
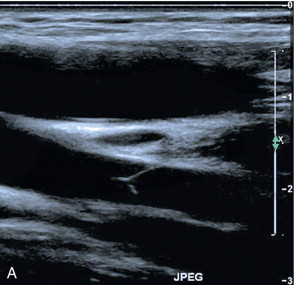
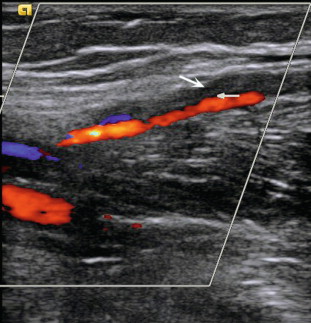
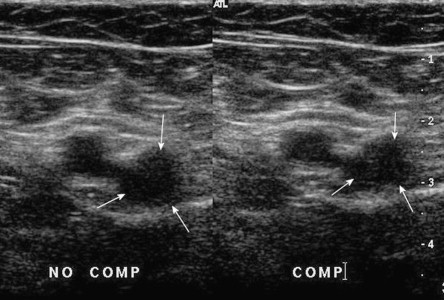
There are three components to the ultrasound examination of the veins for DVT: imaging, Doppler and compression. Thrombus may be seen in the vein, Doppler may show abnormal, or absent, flow signals and compression refers to the fact that a normal vein is easily compressible – light pressure with the transducer will obliterate the lumen of the vein, whereas thrombus in the lumen will prevent apposition of the walls. Two points should be noted in relation to compression: first, compression should be performed in the transverse plane ( Fig. 5-8 ) for the reason that if it is done in the longitudinal plane a thrombosed vein may disappear as it is no longer in the scan plane, rather than because it has been compressed. Second, fresh thrombus is soft and gelatinous, so that firm pressure can produce a degree of compression, which may give a false impression of patency. The use of colour Doppler will clarify this situation. A further reason for scanning in the transverse plane is that dual segments of the superficial femoral vein will be identified more reliably.
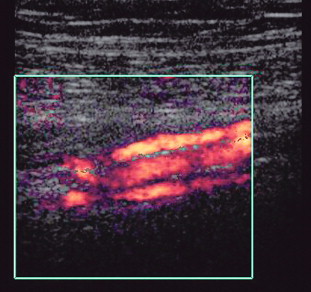
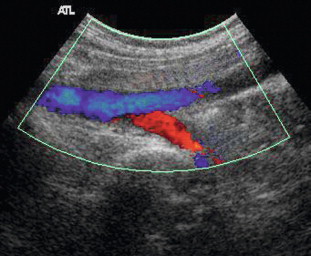
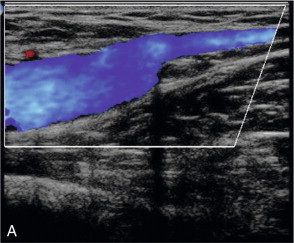
The examination begins at the groin, where the common femoral vein is located on a transverse scan and compressed. Compression is then repeated at intervals of 3–5 cm down the length of the thigh to the adductor canal. At this point the superficial femoral vein is difficult to compress from an anterior approach as it is well supported by the bulk of the anterior thigh muscles. Compression is better achieved in this region by placing a hand behind the medial thigh and pushing up with the fingers against the transducer. The scan plane is then changed to longitudinal and the vein examined with colour Doppler, or power Doppler, as the transducer is moved up the thigh. If the iliac veins are not being formally examined it is useful to obtain a spectral waveform in quiet respiration from the common femoral vein to confirm cardiac and respiratory flow variation being transmitted down patent iliac veins from the chest. Squeezing the calf gently will augment flow and allow easier detection of areas of flow or thrombosis; alternatively, the patient can be asked to plantar-flex their toes, which results in calf muscle contraction and emptying of the calf veins. Colour Doppler is often sufficient, in conjunction with the findings on compression, to confirm or exclude a diagnosis of DVT ( Fig. 5-9 ). If there is any doubt then a spectral assessment will allow a better appreciation of damped flow, absent respiratory variation and impaired augmentation.
Once the thigh veins have been examined the patient is turned into a lateral position, with the medial aspect of the leg being examined uppermost, so that the popliteal veins can be examined. Again, compression and colour Doppler are used to assess the veins. Some patients, particularly postoperative hip patients, may not be able to move into a decubitus position. In these cases the popliteal veins can be examined with the knee partially flexed up off the couch, with external rotation, if possible, so that the transducer can be positioned in the popliteal fossa; a curved array can be of benefit in gaining access in this situation. Alternatively, the leg can be elevated and supported off the couch by an assistant. In addition to the popliteal vein, the main muscular veins draining soleus and gastrocnemius should be assessed, especially if there is pain and tenderness associated with the posterior calf muscles ( Fig. 5-10 ).
The calf veins can be examined after the popliteal vein with the patient in the decubitus position on a tilted couch, or in the supine position with the knee flexed up off the mattress, if the patient is relatively immobile. Alternatively, the patient can sit on the couch with their legs over the side so that the dependent calf veins are well distended. The posterior tibial and deeper peroneal vessels are most easily located by scanning in the transverse plane from the medial side of the calf and identifying the arterial signals on colour Doppler ( Fig. 4-2 ). These veins may also be located on a longitudinal scan; again the arterial signal provides a useful guide to the position of the veins. If there are difficulties identifying the posterior tibial veins at the mid-calf level then scanning the lower calf just above the medial malleolus, where the vessels are superficial and constant in location, may be of value; the posterior tibial vessels can then be followed back up the calf with augmentation of flow as necessary in order to assess patency. In the mid- and lower calf, squeezing the calf can produce motion artefacts from movement of the calf muscles which obscure the flow signals from the veins; in these cases, squeezing the foot will produce adequate augmentation of flow. The anterior tibial veins are examined from an anterolateral approach: scanning transversely, the tibia, fibula and interosseous membrane are identified. The anterior tibial vessels are found on the superficial aspect of the interosseous membrane, although it should be noted that these veins are rarely involved in DVT in isolation from the other calf veins. The peroneal veins may also be visualised deep to the interosseous membrane in many patients from this anterolateral aspect, allowing their examination if they have not been identified from a posteromedial approach; a posterolateral approach is also of value in identifying the deeply situated peroneal veins in some patients.
The iliac veins are examined by following the external iliac vein upwards from the common femoral vein into the pelvis. A 3–5 MHz transducer is usually necessary for adequate penetration. Firm pressure may be required to displace bowel gas. This may produce narrowing or effacement of the more superficial segments of vein, resulting in an absence of signal and a possible false diagnosis of occlusion. If the pelvic veins are difficult to trace superiorly then the common iliac vein can usually be identified just distal to the inferior vena cava and aortic bifurcation; this can then be followed peripherally. In some patients it is impossible to identify the deeper pelvic portion of the iliac veins; however, if there is a patent external iliac vein which shows respiratory variation with good augmentation and a patent upper common iliac vein, then it is highly unlikely that there is significant thrombus in the invisible segment. Transvaginal scanning will show the deeper pelvic veins and may be considered if there is a need to visualise these vessels directly. In thinner patients, or patients with good pelvic access, the proximal internal iliac vein may be seen joining the external iliac vein in the pelvis ( Fig. 5-5 ). The inferior vena cava is examined if thrombus is seen extending into this vessel. It is important, whenever thrombus is diagnosed in a leg vein, that the proximal extent of the clot is identified, as this may have a significant impact on management decisions in relation to anticoagulation therapy, or the placing of a filter.
In pregnant women in the later part of pregnancy, the uterus will lie on the iliac veins in the supine position and compress them, thus reducing flow and impairing augmentation in the lower limb veins. This can be alleviated by asking the patient to turn into a semi-decubitus position, with the side being examined uppermost, so that the uterus falls away, allowing better flow in the pelvic veins. An alternative is to examine the patient standing, as the uterus moves forward away from the iliac veins in this position.
The veins of the upper limb are also divided into deep and superficial groups ( Fig. 5-11 ). The deep veins are usually paired and accompany the arteries: the radial, ulnar and brachial veins; with the axillary, subclavian and brachiocephalic veins more centrally. There is a variable pattern of communicating veins between the deep veins and between the deep and the superficial veins. The superficial system is more variable than in the leg but there are usually two main vessels: the cephalic vein on the radial aspect of the arm and the basilic vein on the ulnar side. These communicate at the cubital fossa by way of the median cubital vein and they also communicate with the deep brachial veins at this level. The basilic vein pierces the deep fascia on the medial aspect of the mid-upper arm to join the brachial veins and this combined venous channel becomes the axillary vein when it enters the axilla. The cephalic vein passes more cranially along the lateral aspect of the biceps. At the level of pectoralis major it turns medially and deeply to pierce the clavipectoral fascia below the clavicle and joins the upper axillary vein. The axillary vein also receives other tributaries from the region of the shoulder joint and the lateral chest wall.
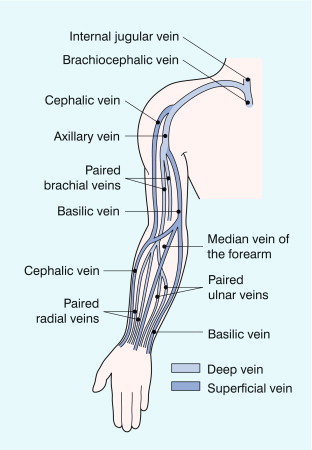
The axillary vein becomes the subclavian vein as it crosses the first rib, where it lies in front of the artery; the main tributary of the subclavian vein is the external jugular vein. The subclavian vein on both sides joins with the internal jugular vein behind the medial end of the clavicle to form the brachiocephalic vein, which is also known as the innominate vein.
Examination of the upper limb veins is normally performed with the patient supine and the arm abducted to about 90ᵒ; the patient may require some support for the arm, or they can be asked to hold onto some suitable part of the ultrasound machine beside them. A transducer frequency of 7–12 MHz can be used. The examination begins above the sternoclavicular joint, where the distal brachiocephalic vein can be assessed and the confluence with the internal jugular vein examined, particularly if central lines have been inserted. The subclavian vein is examined from above and then below the clavicle; it is seen lying in front of the subclavian artery as it runs over the first rib. The axillary vein is then followed across the axilla into the upper arm, from where the brachial veins can be examined down to the elbow. The veins below this are not usually examined unless there is some specific reason, such as the presence of a dialysis shunt. Augmentation of flow is obtained by manual compression of the forearm, or upper arm; alternatively, asking the patient to clench their fist will increase venous flow. If there is a suspicion of a possible venous compression syndrome, the arm veins can be examined with the limb in different positions of abduction; comparison of flow on the two sides can be of value.
The internal jugular vein runs in the carotid sheath from the jugular foramen in the base of the skull down to join with the subclavian vein; it lies superficial to the carotid artery. There may be significant variation in size between the two sides. It is normally compressed easily by pressure from the transducer, so a light touch is required. Flow in the vein is influenced significantly by right heart activity, so colour Doppler will show variable forward and reverse flow, with spectral Doppler showing the ‘a’, ‘c’ and ‘v’ waves of the jugular pulse. Respiratory variation will also be seen, with increased forward flow during inspiration when intrathoracic pressure is negative and slowing during expiration when the intrathoracic pressure is positive. Flow can therefore be modified by respiratory manoeuvres such as deep inspiration, or a Valsalva.
Clinical diagnosis of DVT is inaccurate and clinical scoring systems, such as the Wells Score ( Box 5-3 ), have been introduced and refined to stratify risk more accurately. In addition measurements of serum D-dimer can be used to further refine the selection of patients more likely to have a DVT who will benefit from an ultrasound scan. Patients with a low probability for DVT should have a D-dimer estimation. If this is negative, they are highly unlikely to have a DVT and do not require scanning; if the D-dimer is positive, or the patient has an intermediate or high probability score for DVT, then a scan should be performed. D-dimer levels are less useful in patients with many pre-existing conditions, or who have recently undergone surgery as false positives are more common ( Box 5-4 ).
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
A score of two or higher indicates that the probability of deep vein thrombosis is likely; a score of less than two indicates that the probability of deep vein thrombosis is unlikely. In patients with symptoms in both legs, the more symptomatic leg is used.
The diagnosis of normal or thrombosed veins is based on the compressibility of the veins, the appearance of the veins and the changes which occur to the spectral and colour Doppler findings. The main changes associated with DVT are shown in Box 5-5 . The lower limb is examined for possible thrombosis much more frequently than the upper limb, although the principles and features described are also applicable to the arm veins.
Absent or reduced compressibility
Thrombus in the vein: static echoes, incomplete colour fill-in, expansion of the vein
Static valve leaflets
Absent flow on spectral or colour Doppler
Impaired or absent augmentation of flow
Loss of spontaneous flow and respiratory variation
Increased flow in collateral channels
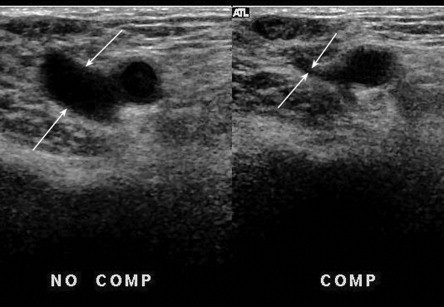
As noted above, a normal vein is easily compressible with only mild to moderate pressure from the transducer, so that the lumen is completely obliterated. A vein filled with thrombus will be held open ( Fig. 5-12 ), although it must be remembered that fresh thrombus has the consistency of jelly, so that it can be compressed to some extent by strong pressure.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here