Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acknowledgment: We would like to recognize our friend and partner Douglas P. Hanel, MD, who was a coauthor on the sixth edition version of this chapter. His contributions to it, and to hand surgery in general, are innumerable, and we are proud to have him as a partner.
Mangling injuries of the hand and upper extremity are devastating injuries that involve multiple critical structures of the fingers, hand, arm, or any combination of these. They nearly always lead to significant disability, both directly and through their psychosocial impact. Such injuries can have a dramatic influence on patients’ livelihoods and ability to carry out activities of daily living. Because the forces involved in producing mangling injuries of the upper extremity are great, serious injury to other organ systems and/or other areas of the body are generally also present and nearly always take precedence over extremity injury management.
Preserve life
Preserve tissue
Preserve function
Reconstruct and restore function of both the extremity and the patient
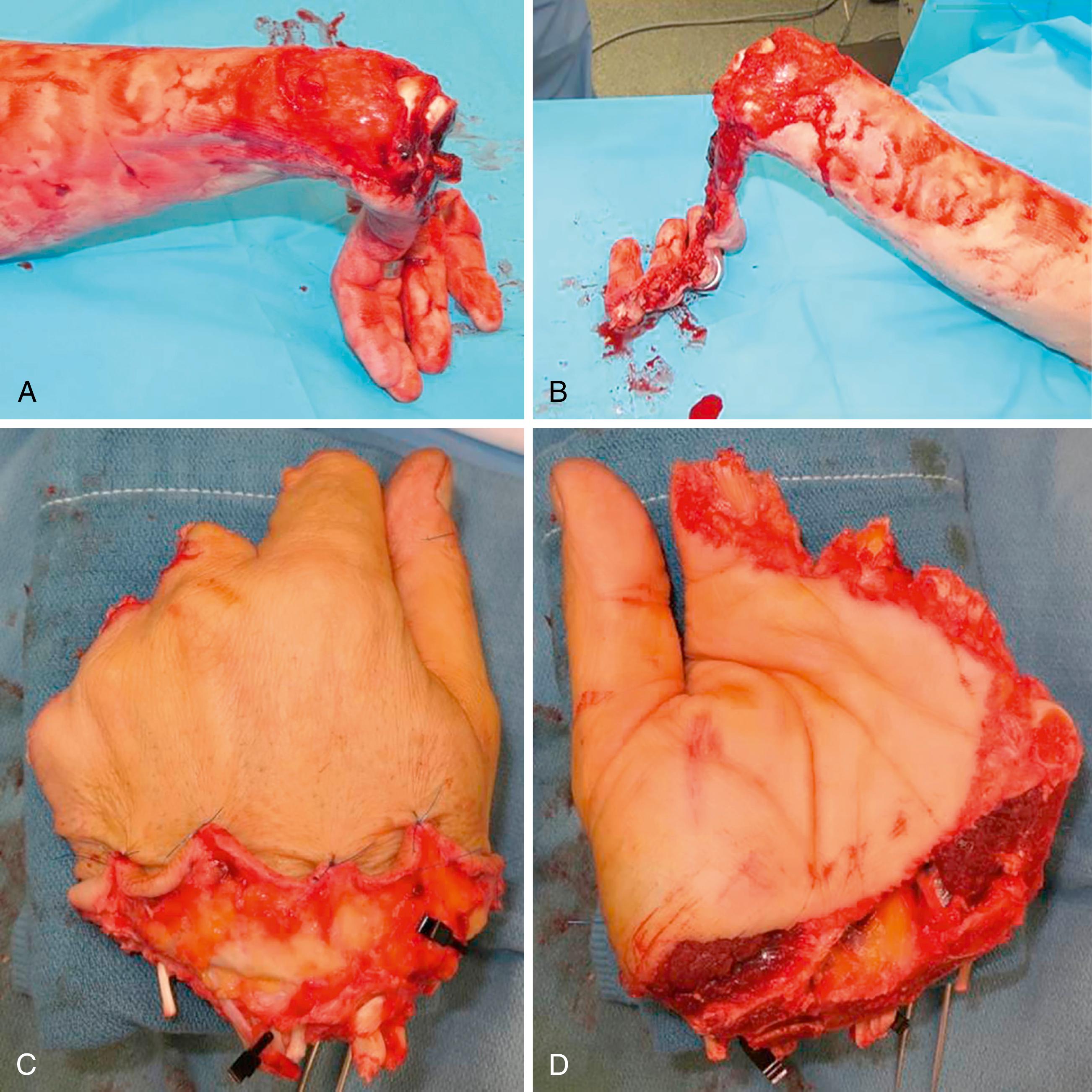
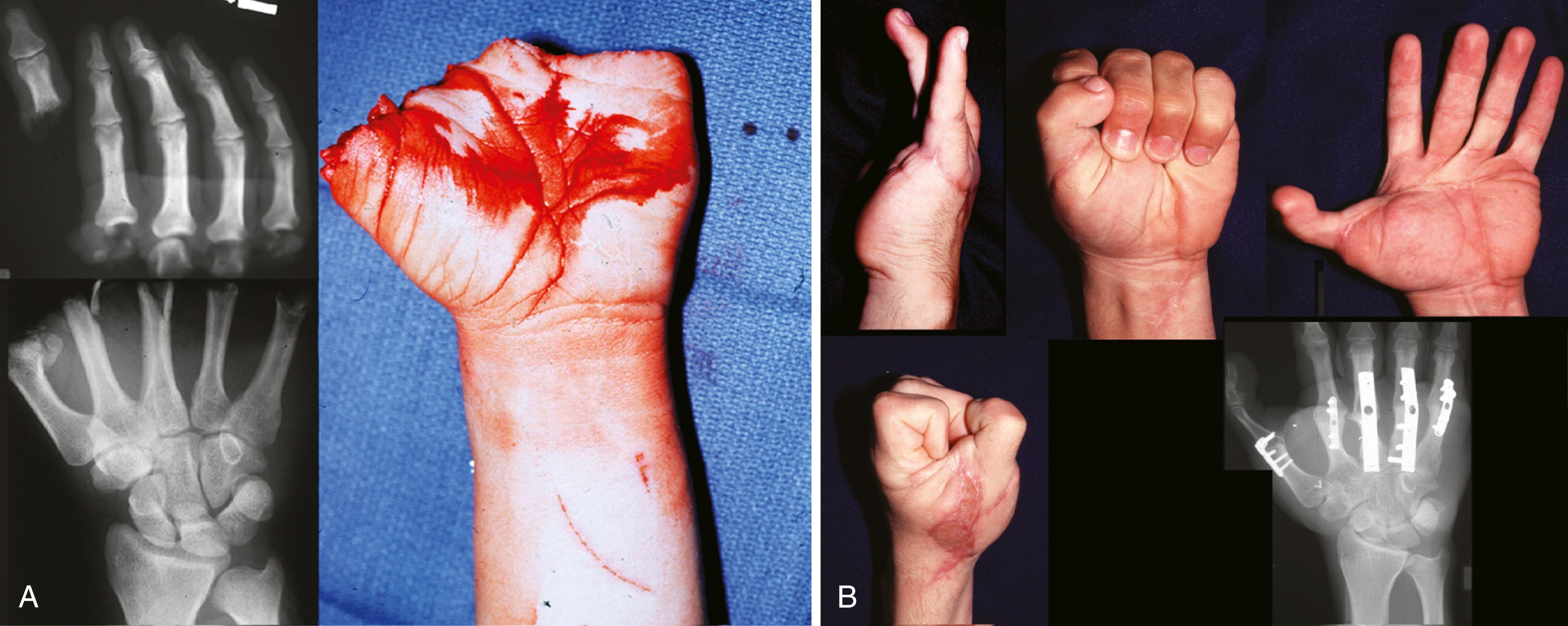
Mangling injuries generally include all or nearly all of the major functional systems of an extremity, including skin and soft tissue, vascular, nerve, muscle and tendon, bone, and joint ( Fig. 43.1 ). It is because of this multisystem injury involving all or nearly all layers of the extremity that ultimate function is at risk. Despite the best attempts at reconstruction, a scar will form from the skin down through bone and compromise the function of all structures involved and the extremity overall. Peacock elegantly described this as the “one wound–one scar” concept ( Fig. 43.2 ). ,

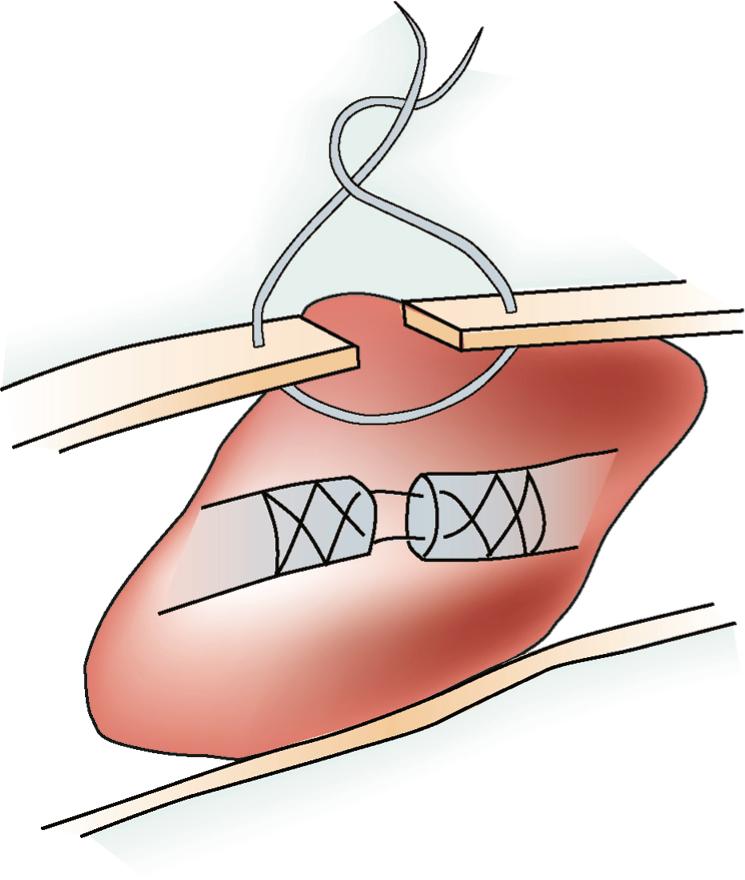
This variable involvement of critical, interdependent structures and the disabling result of the one wound–one scar concept led to the “combined injuries” model described by Büchler and Hastings. The eventual impact of the scarring process must therefore be kept in mind throughout planning and reconstruction. Efforts to minimize the negative effects of this process requires adherence to the following general principles in the management of mangling injuries:
Complete debridement of devitalized tissue
Restoration of good vascularity
Rigid skeletal fixation while minimizing additional soft tissue injury
Stable, vascularized soft tissue coverage
Timely intervention for both repair and reconstruction
Comprehensive rehabilitation
Secondary procedures, as needed
By following these principles, one can allow early mobilization of the extremity, thereby minimizing the impact of “one wound” scarring and maximizing ultimate motion.
The multisystem nature of mangling injuries demands knowledge and expertise in multiple disciplines related to trauma and reconstruction, including trauma surgery, orthopedic surgery, vascular surgery, and plastic surgery, and often benefits from a multispecialty team approach. Because of the diverse nature of mangling injuries, no two cases are alike; in general, there is no single preferred approach. Rather, a set of principles is used to guide the surgeon through the application of multiple approaches and techniques that address each of the involved systems while keeping in mind the impact of various treatment decisions on the comprehensive reconstructive plan and final outcome. Many of the specific operative approaches are detailed elsewhere in this textbook, and therefore this chapter concentrates on principles, judgment, and timing.
What is here is an outgrowth of two chapters in a previous edition of this text, Open Injuries of the Hand and Combined Injuries, to which the authors refer the reader as excellent resources on the topic of mangling injuries of the hand, , as well as several other excellent reviews. Sometimes amputation is the most appropriate treatment, and the choice between amputation and salvage with reconstruction requires looking into the “crystal ball” that shows 6 to 12 months in the future in an attempt to predict the patient’s overall function. Which of the various treatment choices is appropriate? After that question, a comprehensive reconstructive plan that includes both short- and long-term objectives must be formulated. Optimal management of a mangled extremity is therefore one of the most challenging aspects of hand surgery; it requires a broad knowledge and facility with various techniques and the judgment and experience to know when and how to apply them. It is a true test of one’s mastery of the art of hand surgery.
Careful and complete evaluation of the injury in which all functional systems are addressed
Formulation of a comprehensive reconstructive plan tailored to the patient’s needs
Thorough but careful wound debridement of all devitalized tissue
Meticulous operative reconstruction, often including secondary procedures
Restoration of good vascularity
Rigid skeletal fixation while minimizing additional soft tissue injury
Stable, vascularized soft tissue coverage
Comprehensive rehabilitation
Secondary procedures, as needed
There have been various attempts by hand and upper extremity surgeons to classify mangling hand injuries, but none of the classification systems has been universally adopted. In 1990 researchers in Seattle published the Mangled Extremity Severity Score (MESS), which used objective criteria to predict lower extremity amputation following trauma. Although attempts have been made to apply the MESS to upper extremity mangling injuries, the scoring system in general has not proved helpful in predicting which extremities should be amputated and which should be salvaged. , One of the reasons why this scoring system is not entirely useful for the upper extremity is that it is not a weight-bearing extremity; therefore upper extremities with a MESS score of 7 or greater (which, in the original study, was a predictor for amputation) can often be salvaged and be somewhat useful. Other classification systems, such as the Hand Injury Severity Score (HISS), have emerged, and while they have some utility in predicting time lost from work, they have not been helpful in predicting need for amputation. ,
A wide variety of mechanisms can produce mangling injuries, including industrial and agricultural machinery, motor vehicles, power tools, explosives, and firearms. Most mangling injuries involve some component of a crush injury whereby multiple tissue layers and anatomic systems are injured or destroyed. Certainly, crushing and blast injuries, with their extensive tissue destruction and associated late scarring, are far more difficult to reconstruct and portend a worse outcome than do sharp injuries. As a result of the immediate and delayed tissue necrosis with crushing injuries, the risk for infection is increased, and it often compromises the reconstructive plan. Degloving or avulsion injuries are also frequently mangling in that they involve amputation or partial amputation of one or more critical tissue layers. Abrasion and burn injuries, depending on the extent and depth of involvement, can also be significant components of mangling injuries.
It should be obvious that mangling injuries frequently result in severe wound contamination, depending on the environment and specific mechanism by which they occur. Farming injuries in particular are usually associated with major contamination and require more extensive and often serial debridement and irrigation and special consideration in planning antibiotic management. The combination of a contaminated injury environment with crushed and devascularized tissue is a dangerous scenario for major life-threatening infection if not recognized and appropriately managed.
A constant element in most mangling injuries is tissue devascularization, which can occur at multiple levels. Crush, avulsion, degloving, or blast injuries can disrupt major vessels or the branching perforator vessels to muscle and skin, or they can produce endothelial injury that results in thrombosis of large and small vessels, including the microcirculation. Crushing can also cause direct cell disruption and tissue necrosis. Different tissues are more or less susceptible to crushing, with vessels, fat, muscle, and skin being the most severely injured in that order. Nerve is unique in that it is often the last structure remaining physically “intact” after a crush or avulsion injury, yet axons themselves are quite susceptible to crushing or stretching, which can lead to a difficult dilemma in distinguishing neurapraxia from axonotmesis in the early stages. Tendon, ligament, and bone tend to be more resistant to crushing/avulsing forces; nevertheless, partial injuries to tendon and ligament can result in significant scarring and functional impairment that can be minimized only by timely recognition and early and aggressive mobilization.
Because mangling injuries of the hand and upper extremity are often associated with considerable force; it is not uncommon for the patient to have other significant and potentially life-threatening injuries. The mangling extremity injury, although frequently the most obvious, graphic, and visually compelling, rarely leads to loss of life. As always, one must look beyond the obvious extremity injury and evaluate the patient carefully for other serious injuries. The standard Advanced Trauma Life Support approach to any injured patient must be followed, with immediate attention to the airway, breathing, and circulation (ABCs), followed by primary and secondary surveys of the injured patient.
As always, the key components of the medical history focus on the “when,” “where,” and “how.” The time of injury is critically important, especially when dealing with devascularizing injuries. Bone, integument, and muscle have, in that order, decreasing tolerances to ischemia, with muscle being able to survive only 4 to 6 hours of it, even with the normal tissue cooling that occurs after ischemia. In addition, the longer the duration from the time of injury, the greater the risk for infection, with delays greater than 6 to 12 hours precluding primary closure or coverage. If ischemia is present, the temperature of the tissue during the ischemic period is critical inasmuch as extremity tissues devoid of muscle can be successfully revascularized after 12 to 24 hours if kept cool. In fact, successful digit replantation has been reported at 94 hours.
The “where” of an injury is also important. Farming injuries, for example, tend to be highly contaminated and require more than the usual amount of aggressive debridement, which often precludes primary closure. The presence of caustic industrial chemicals or other contaminated substances can also affect treatment choices. The social and economic aspects of the injury environment must likewise be weighed when planning treatment. A patient living in an area remote from an appropriate medical facility may not be able to follow through with the complex rehabilitation program required for a highly technical reconstruction and may be better served with a more straightforward reconstructive option.
Finally, the “how,” or mechanism of injury, can help reveal the force of it and the extent of tissue necrosis or zone-of-injury to anticipate and address during treatment. Sharp injuries tend to involve a limited zone of tissue and are therefore easier to manage, unless the injury is tangential in nature. High-velocity, high-pressure crushing or avulsion injuries have a much broader injury zone and require a modified approach to treatment, which needs to consist of more extensive debridement, thorough evaluation of adjacent tissues, removal of foreign bodies, and assessment for and treatment of compartment syndrome.
The patient’s overall health and comorbid conditions must be carefully evaluated in planning any type of complex or lengthy reconstructive procedure. The patient’s age and the presence of cardiovascular disease, pulmonary disease, bleeding disorders, or diabetes can greatly increase the risk for perioperative complications or even mortality; any of these should cause the surgeon to consider simplifying the reconstruction method or at least modifying perioperative treatment plans. Smoking or the use of other vasoactive drugs, such as cocaine, may be a relative contraindication to any type of complex microvascular reconstruction, although the data about smoking and microvascular surgery complications is somewhat mixed.
Perhaps the most important aspect of obtaining a history is determining the patient’s functional needs and goals. The age, occupation, socioeconomic environment, and social support systems should all be considered when formulating a treatment plan. Both the risks that the patient is willing to accept and the costs (financial, emotional, and time) must be considered. Willingness to endure a protracted reconstructive course and a patient’s ability to follow through with the necessary hand therapy are important issues. A self-employed farmer, without workers’ compensation insurance, will probably be interested in reconstructive options that offer an expeditious return to work and provide durable function suited for heavy work without multiple complex reconstructive procedures.
An office worker or technology professional may have very different goals and might be more willing and economically able to undergo multiple reconstructive procedures to restore optimal digit function to allow fine manipulation, keyboarding, and other such tasks. Again, the hand surgeon must make decisions based on personal knowledge and experience to try to predict the patient’s ultimate function with the available reconstructive options so that the most appropriate option can be selected for that particular patient. Both the patient and the patient’s family must be involved in this discussion, although this is often difficult to do when the patient has just suffered a mangling injury, therefore surgeons frequently must use their best judgment at the time by assessing all the known variables.
Because examination of a patient with a severely mangled extremity injury that is wrapped in blood-soaked towels or bandages is often difficult in the emergency department, definitive evaluation often must wait until the operating room. Nevertheless, assessment of injuries to major structures, in particular vascular status, is essential to determine the urgency of definitive treatment and to begin the determination of salvageability. Usually, a general assessment of vascular status, sensibility, and muscle–tendon unit function, as well as radiographic evaluation, can and should be done in the emergency department. Preliminary evaluation will also allow adequate preparation of the operating room: microsurgical equipment and supplies, implants and fixation devices, traction and radiographic devices, and other necessities.
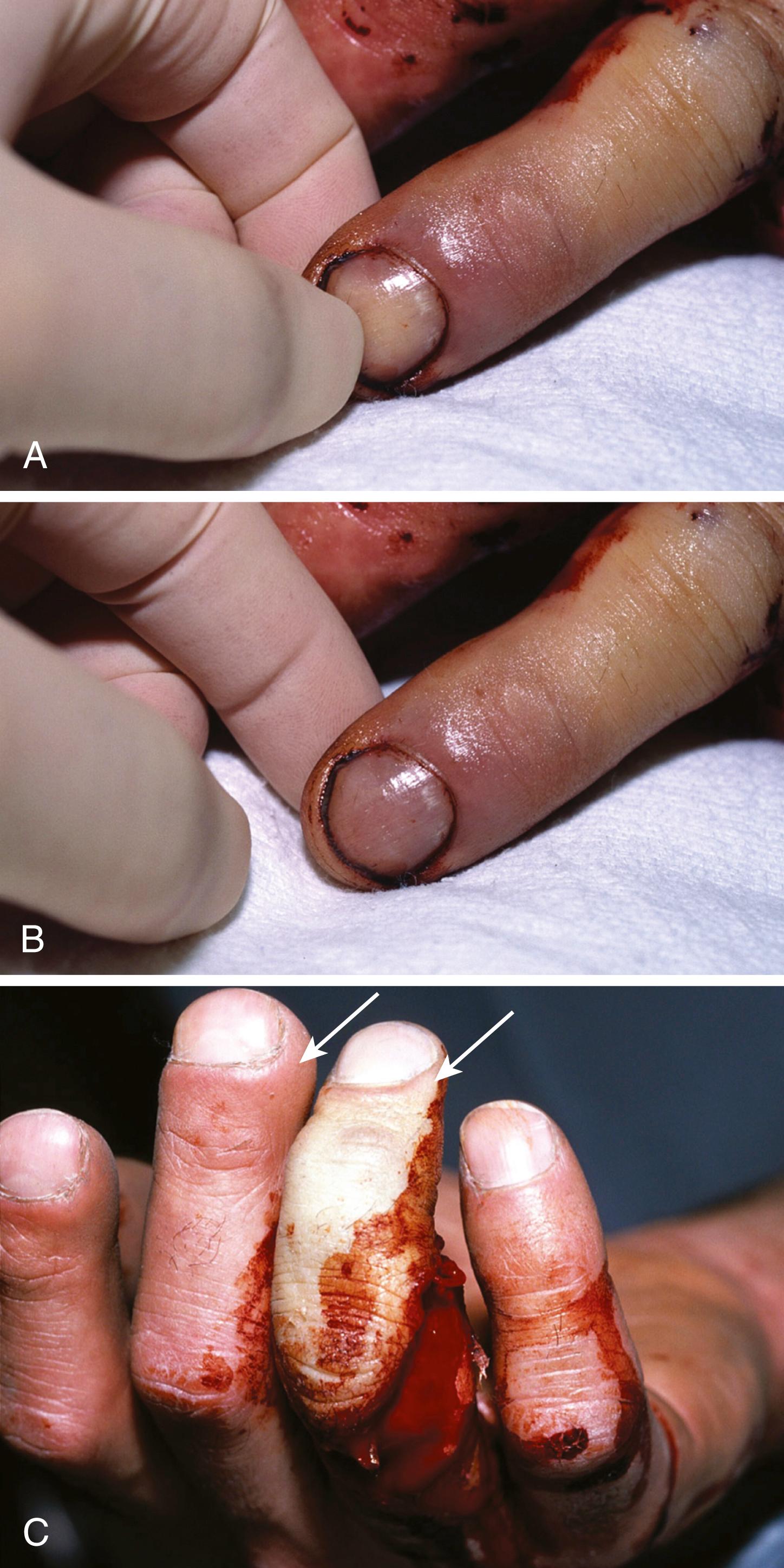
Assessment of vascular status is best performed by direct inspection of the patient’s affected tissues and comparison to adjacent or similar well-vascularized tissues. Although nail bed capillary refill is traditionally considered a good indicator of peripheral perfusion, it is in fact an unreliable indicator of perfusion. A completely devascularized digit can have what appears to be intact capillary refill beneath the nail bed when in actuality stagnant blood is merely being pushed to the sides with compression and then moving back to the center with release of pressure on the nail bed.
A far more reliable area to assess digit perfusion is the dorsal paronychial tissue on the sides of the nail, which should be pink, be spongy, and have good turgor, compressing with pressure and refilling with release ( Fig. 43.3 ). A pink color that returns within 1 to 2 seconds after the application and release of pressure indicates healthy tissue, whereas a pale color without capillary refill or turgor can represent arterial insufficiency. A dusky color with exceptionally brisk refill can be indicative of venous congestion. Probably the most reliable clinical indicator of tissue vascularity is the color of the blood that oozes from the tissue after sticking it with a needle or scalpel. Bright pink oozing reflects healthy tissue, whereas dark purplish oozing reflects compromised perfusion if it is sluggish or venous insufficiency if it is profuse. Obviously, this should not be performed on the sensate tissue of an awake patient but is often useful in an anesthetized one.
For assessing the status of the major vessels of the upper extremity and even the digital vessels, a handheld Doppler probe is very useful. The standard Allen test, performed by compressing either the radial or the ulnar artery and listening for a signal over the palmar arch or the most distant digital artery, can help determine whether either the radial or the ulnar artery has antegrade flow and whether the palmar arch is intact. Angiography has a minimal role in mangling injuries of the forearm, hand, or fingers. In any mangling or crushing injury, a high index of suspicion for compartment syndrome must be maintained.
The diagnosis and treatment of compartment syndrome are covered elsewhere, but it is worth reinforcing the importance of recognizing the intense pain of it and, in particular, pain with passive stretch of muscle–tendon units. When suspected, the diagnosis is best confirmed by direct measurement of pressure in the muscle compartment, usually with a handheld device specifically designed for this purpose. The presence of compartment syndrome and attendant tissue ischemia warrants emergency decompression in the operating room.
Although obvious deformity, crepitus, or tenderness on examination can suggest underlying skeletal injury, evaluation of the skeletal system is always performed radiographically. In most instances, standard radiographs are sufficient if care is taken, whenever possible, to ensure that emergency splints or traction devices do not obscure the underlying bones or joints. Sometimes, additional views are needed, including oblique views to assess articular congruity or stress views to evaluate ligament injury (e.g., a clenched fist view to evaluate intercarpal ligamentous integrity). In questionable cases, comparison views with the contralateral extremity, if uninjured, may be necessary.
With most mangling injuries, advanced imaging techniques, such as computed tomography (CT) or magnetic resonance imaging (MRI), are rarely indicated, although at times if the patient is stable, CT scanning of suspected carpal injuries or intraarticular displacement can be useful. If amputated parts are involved and replantation is contemplated, radiographs of the amputated part(s) should be obtained. Moreover, the joint proximal and the joint distal to the area of injury must be evaluated ( Fig. 43.4 ). Ligamentous injuries can be identified by tenderness to palpation or to stress. Stability with the application of stress should also be reevaluated under anesthesia to remove any confounding effect of involuntary muscular splinting.
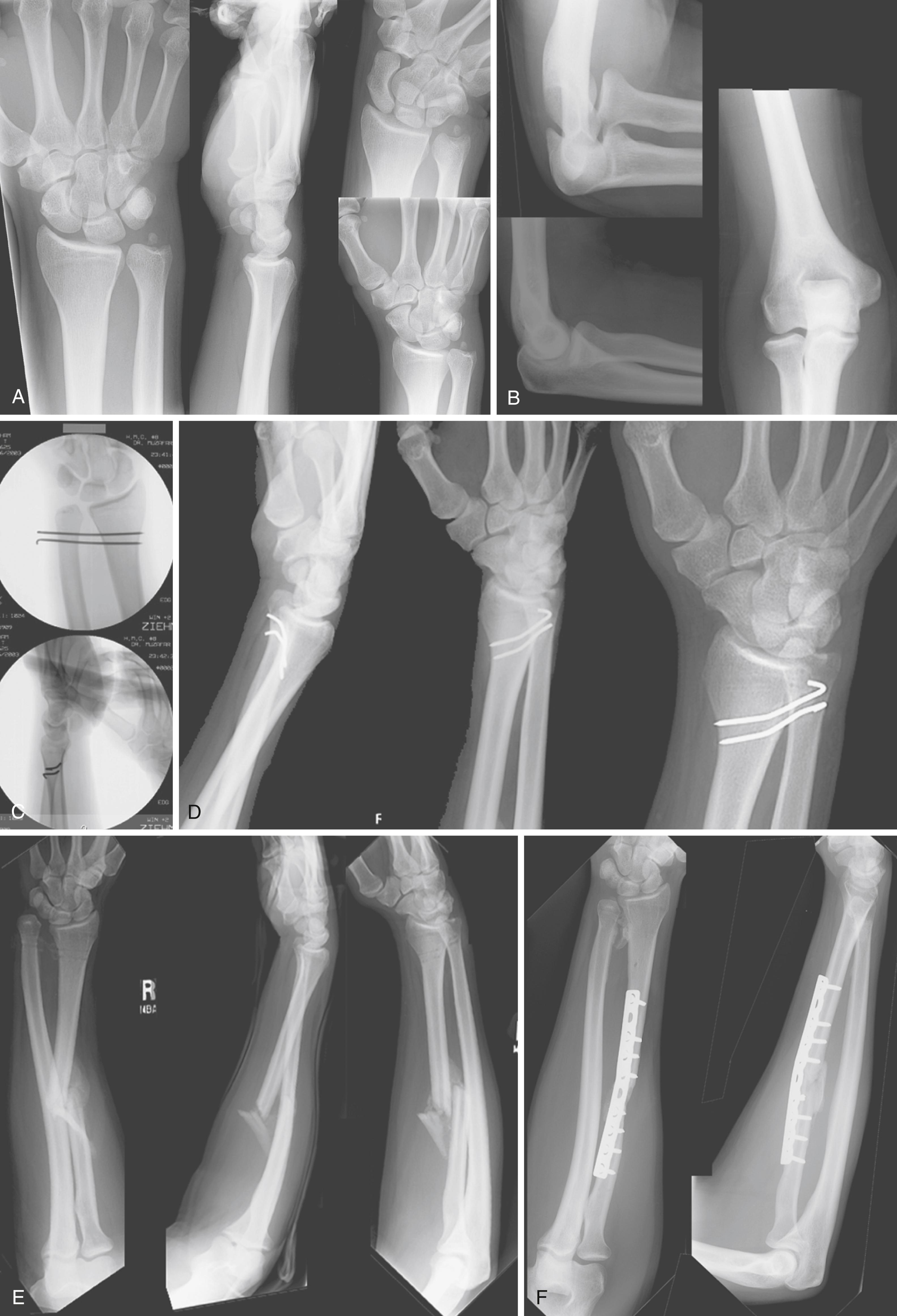
Evaluation of injury to muscle–tendon units is best performed by having the patient actively flex and extend the digits and wrist. In the presence of pain, and especially with underlying skeletal injury, this examination can be difficult to interpret. For the individual digits, noting aberrations in the normal resting cascade can indicate injury to the underlying flexor muscle–tendon unit. This simple observation can be performed even in an obtunded or sedated patient, as can evaluation of tendon function by passively flexing and extending the wrist and observing the normal cascade of digit flexion with wrist extension and digit extension with wrist flexion ( Fig. 43.5 ). In the end, however, with most mangling injuries, definitive evaluation of tendon injury must wait for careful examination in the operating room.
Nerve injury is evaluated by examining both motor and sensory function. The motor function of the median, radial, and ulnar nerves is assessed by testing both extrinsic and intrinsic muscle function. Three simple maneuvers test motor integrity: (1) resistance to palmar abduction of the thumb reflects median nerve–innervated abductor pollicis brevis function, (2) resistance to flexion of the metacarpophalangeal (MCP) joint of the small finger reflects ulnar nerve–innervated flexor digiti quinti function, and (3) resistance to extension of the MCP joint of the index finger reflects radial nerve–innervated extensor digitorum communis and extensor indicis proprius function.
Accurate sensory examination is much more difficult, especially in patients with severe injury. By using a light touch and, if questionable, pinprick testing, a reasonable assessment can nevertheless be obtained. If the injury is in the palm or digits, attention is directed to digital nerve function, whereas if the injury is more proximal, attention is directed to independent areas of sensory function, such as the volar aspect of the index or middle finger for median nerve function, the volar aspect of the small finger for ulnar nerve function, and the dorsum of the first web space for radial nerve function.
With penetrating injuries, if you “think the nerve is probably OK,” it usually is not. Equivocal results on examination generally indicate an underlying injury that warrants exploration, whereas normal sensory results usually indicate an intact nerve. With blunt or blast injuries, however, nerve contusion and neurapraxia with the nerve in continuity are common. The threshold of suspicion for exploration of nerves in patients with penetrating injuries should therefore be much lower than with blunt or blast injuries.
Laboratory studies should be obtained at the time of initial evaluation, including a complete blood count with platelets, electrolytes, and any other tests appropriate to the clinical situation (e.g., blood gas analysis, toxicology screen, amylase, and others). In addition, if there has been significant bleeding or considerable bleeding is anticipated during surgery, blood for typing and cross-matching should be obtained at this time.
In developing a treatment plan for mangling injuries of the hand and upper extremity, the surgeon must keep in mind the seven basic functions of the hand: precision pinch, opposition pinch, key pinch, chuck grip, hook grip, span grasp, and power grasp. Depending on the severity of the injury, some of these functions may not be restored. The basic units that underlie hand function are the following:
An opposable thumb
The index and long fingers, which serve as the stable fixed unit of the hand for fine manipulation and power pinch
The ring and small fingers, which serve as the mobile unit of the hand for grasping functions
The wrist ( Case Study 43.1 ) FLOAT NOT FOUND
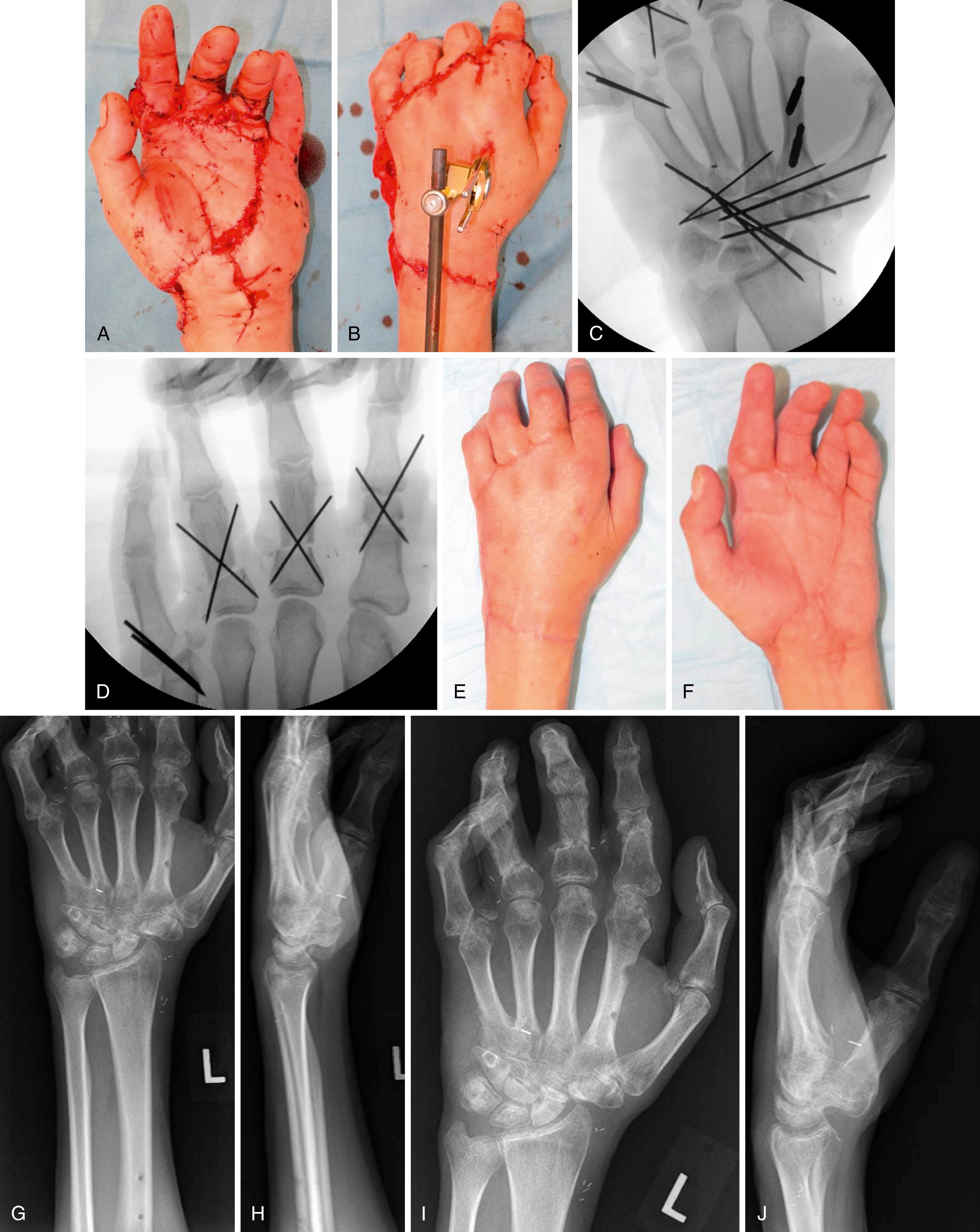
A 57-year-old male was using a chop saw when his left hand became caught in it. The patient presented with the amputated part in saline gauze on ice ( eFig. 43.1 ).
After assessing the patient and speaking with him, he indicates a desire for replantation. Based on the injury pattern, you recommend:
Revision amputation through wrist
Replantation of thumb/hand part only
Replantation of thumb/hand part, plus index finger
Replantation of thumb/hand part, plus middle finger
Answer: (d) Replantation of thumb/hand part, plus middle finger
Rationale: While a wrist-level amputation would allow the fastest recovery, it would be functionally limiting. Replantation of the thumb/hand part would not be very functional as the thumb would not have anything against which to pinch/grasp. When choosing between replantation of the index versus middle finger, the middle is typically chosen because the index is considered expendable in multiple-digit replantations.
See postoperative photos and images in eFig. 43.2 .
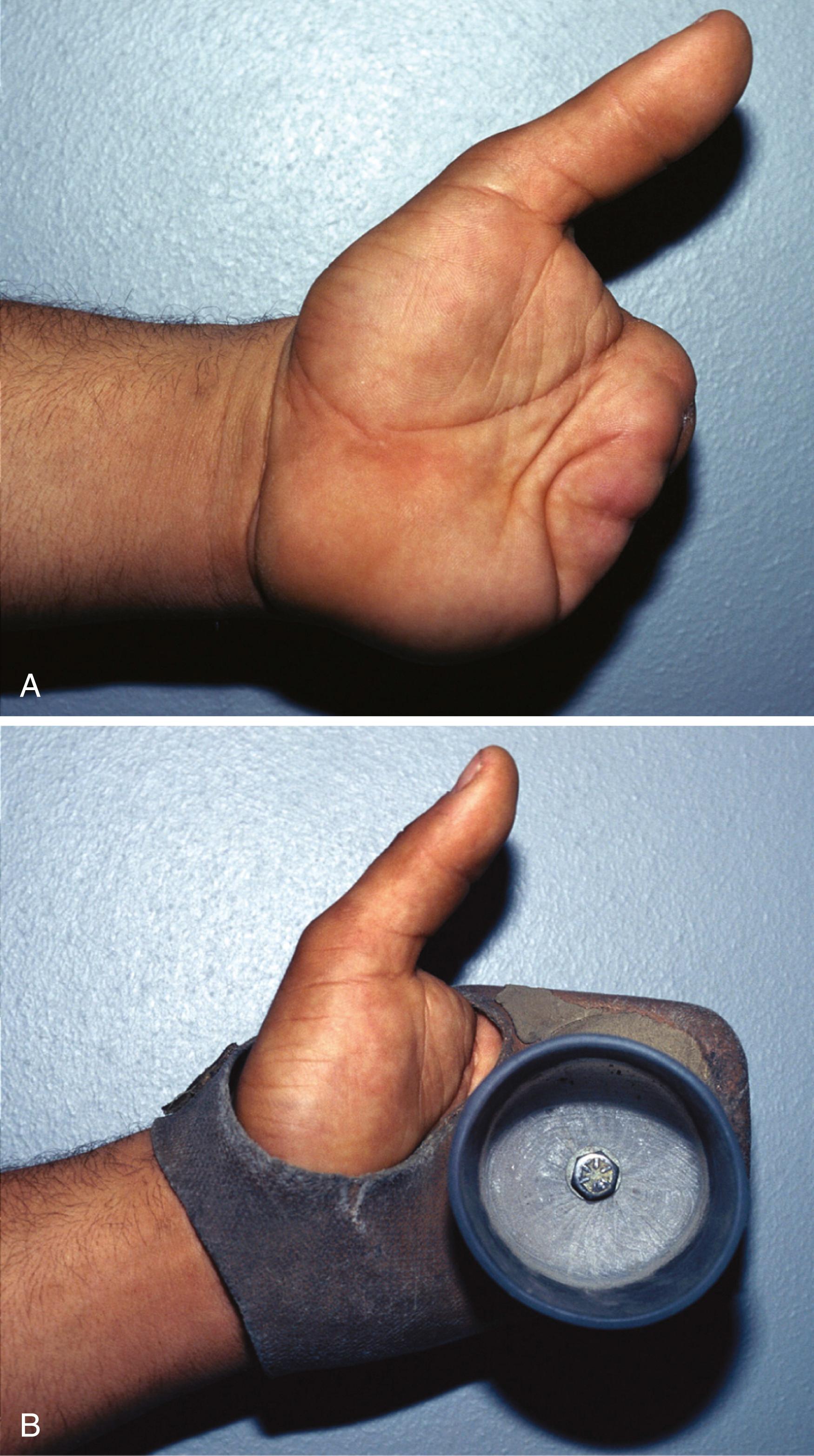
Restoring these units should therefore be the general goal of reconstruction, with restoration of an opposition digit and a stable opposition post being the bare minimum. Preservation of length should be a goal, but only functional length should be preserved. Durable, stable soft tissue coverage is a necessity, as is at least protective sensation. Without these, chronic breakdown, infection, and failure of the reconstruction can be expected. Not all patients are best served by complex digit reconstruction, especially if the digit is going to be stiff or painful. Sometimes, a prosthesis customized to the patient’s occupation is the best option ( Fig. 43.6 ). Highly functional, durable mechanical prostheses, as well as advanced myoelectric prostheses, allow excellent return of function and are discussed in Chapter 50 .
According to the guidelines of the American Medical Association (AMA) for evaluation of permanent impairment, the thumb accounts for 40% of hand function, the index and middle fingers for 20% each, and the ring and small fingers for 10% each. These contributions should be kept in mind when deciding between reconstruction/replantation versus amputation. In the case of mangling injuries, however, these relative contributions do not always apply. For example, with loss of the three central digits, the small finger effectively assumes 50% of hand function.
As discussed previously, surgeons must use their knowledge, experience, and best judgment in an effort to predict a patient’s ultimate function with amputation versus reconstruction and with the various reconstructive options. The factors of patient age, health, drug or nicotine use, occupation, and willingness and ability to undergo complex or multistage reconstructive procedures and rehabilitation must be taken into account. The topics of amputation, replantation, and thumb reconstruction are covered elsewhere in this text, and the reader is referred to these sections for more detailed coverage of the topics.
The thumb is, of course, the most important digit to preserve or reconstruct. The issues related to thumb amputation are discussed in Chapter 48 and vary depending on the level of injury. Interphalangeal (IP) joint motion and the distal phalanx are of relatively lower importance to preserve than multiplanar carpometacarpal (CMC) motion and, to a lesser extent, MCP motion. The ability to bring the thumb out of the plane of the hand and into a position of opposition is a key function that must be restored. If the thumb cannot be preserved, consideration should be given to primary pollicization ( Case Study 43.2 ). FLOAT NOT FOUND
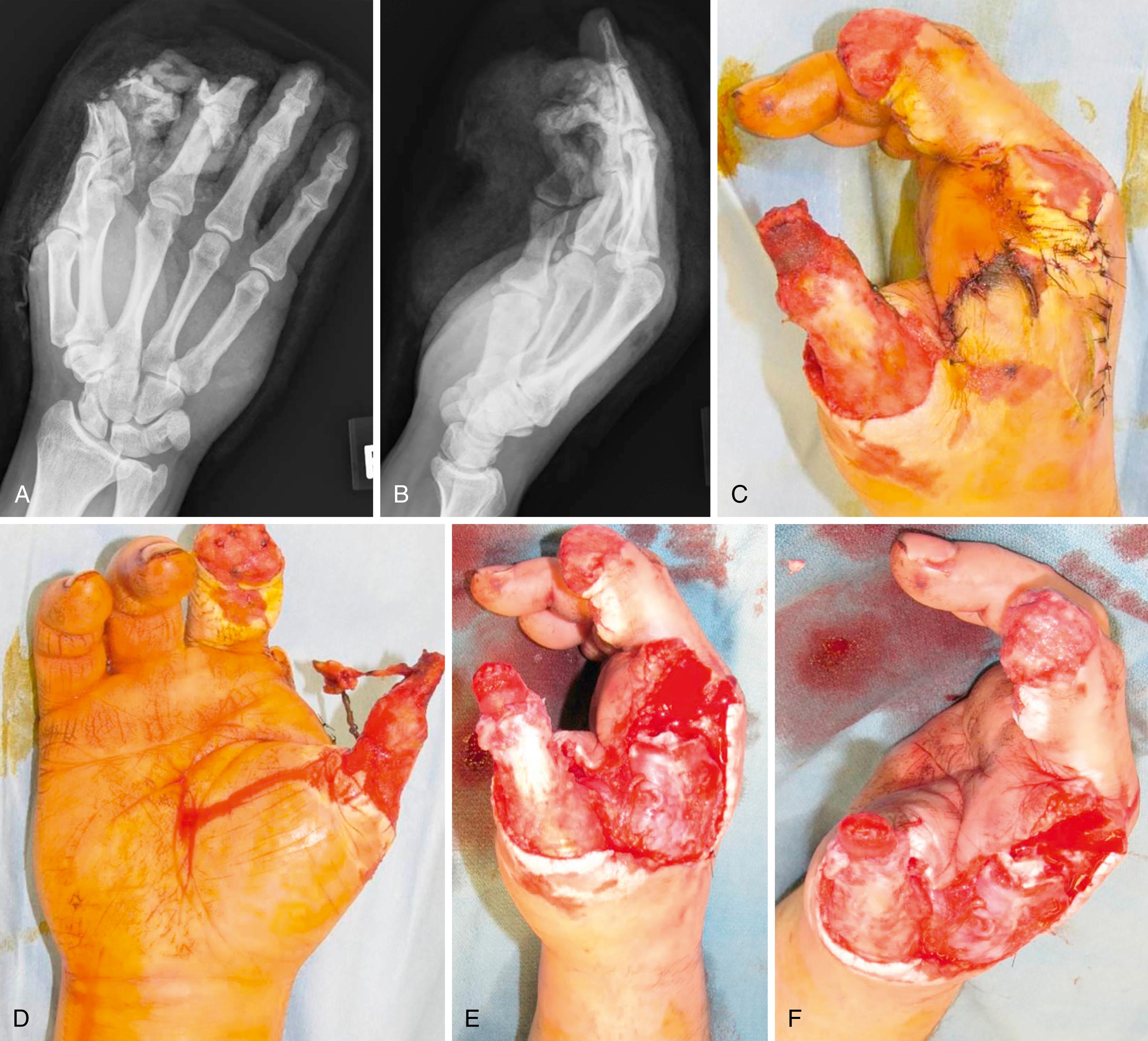
A 50-year-old male suffered a crush/avulsion injury from industrial machinery to his thumb, index, and middle finger. Initial debridement and index ray amputation were performed ( eFig. 43.3 ).
What is the preferred coverage method for this wound (keeping in mind that a toe transfer may be needed for thumb reconstruction)?
Pedicled reversed radial forearm fasciocutaneous flap
Groin flap
Free radial forearm flap
Split thickness skin graft
Answer: (b) Groin flap
Rationale: A split thickness skin graft is not appropriate coverage for the exposed thumb skeleton. While a pedicled or free radial forearm flap would provide coverage, both of these options would alter the radial artery, which is the preferred recipient artery for a toe transfer. Therefore a groin flap is the preferred coverage type.
See postoperative images in eFig. 43.4 .

The index finger is also important to preserve because of its independent profundus flexion and ability to abduct for precision pinch functions. Without good function and sensibility of the proximal interphalangeal (PIP) joint, however, the index finger is often bypassed in favor of the middle finger because it can be more of a hindrance than help. Index ray amputation can often improve function by opening the first web space. , Amputation at or proximal to the PIP level leaves only the intrinsic muscles for digit flexion, which is then limited to about 45 degrees. The long and ring fingers are important primarily for grip and grasp functions, although either can take over pinch functions for the radial digits if they are lost. Solitary loss of the ring finger probably results in the least associated functional deficit of all the digits. The small finger, even though it has the least flexion strength, is actually quite important in hand function in that it defines hand width for grip functions, use of tools, and other applications. An important component of this function is the significant CMC motion of the small finger that comes into play with terminal grip. This action has been called “ulnar opposition” by some authors.
With amputation at the proximal aspect of the middle phalanx (P2), PIP, or especially the MCP level, ray amputation also needs to be considered. Although ray amputation is usually esthetically preferable to a partial finger amputation, function can suffer. For the index finger, power grip, key pinch, and supination strength are diminished approximately 20% and pronation strength approximately 50%.
Loss of an isolated digit other than the thumb rarely results in significant compromise of hand function, and as Brown has noted, patient motivation is more important in regaining function than the actual digits lost. Loss of multiple digits, however, is common with mangling injuries and frequently results in significant functional deficits. Maintaining or reconstructing at least the thumb and one opposing digit is a minimum requirement for any type of pinch or grasp. Retaining or reconstructing an additional adjacent digit can nevertheless add significant function by providing lateral stability to the radial digit for power pinch and can allow three-jaw chuck pinch.
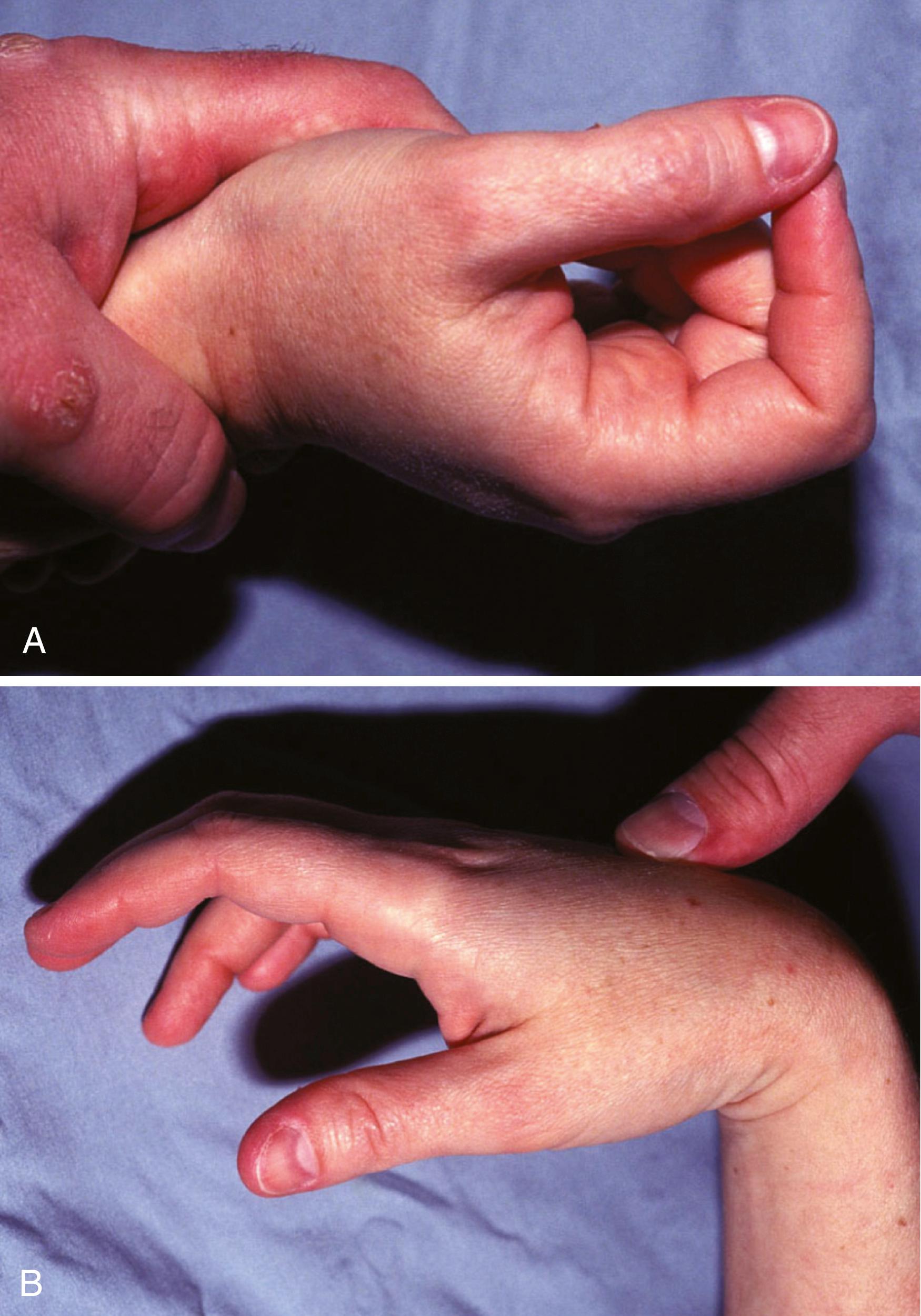
The choice of whether to salvage or fuse a joint is another decision that is often difficult. It is best made by weighing the potential loss of function from a given fusion or set of fusions against the risk for limited motion, pain, instability, or late arthrosis with reconstruction. Whenever anatomic articular congruity and ligamentous stability can be restored, reconstruction is usually worthwhile. When it cannot be achieved, the potential loss of function needs to be assessed. In general, distal interphalangeal (DIP) fusion of the digits or IP fusion of the thumb is tolerated well with limited loss of function. PIP joint motion is much more important to preserve. Littler and colleagues described the PIP joint as the “functional locus of finger function.”
Not only are fingers with fused PIP joints of little use for grip or grasp, but they also frequently get in the way and are easily injured because they do not follow the normal arc of the other fingers. An additional problem, though less so with the index finger, is the quadriga effect, which can occur when profundus excursion is impaired with arthrodesis. Although delayed arthroplasty can be considered, combined injuries involving the joint, nerve, and soft tissue, in the presence of an unreconstructible PIP joint, warrant serious consideration for amputation, especially of the ulnar two digits.
The MCP joint is perhaps the most important joint in terms of function for the index through small fingers in that it contributes 77% of the total arc of finger flexion. Most activities, however, do not require the full arc of MCP motion, and in fact as little as 35 degrees of motion can be acceptable if that arc is within the key functional range and the joint is stable. To that end, stable but markedly limited MCP motion, even arthrodesis, is far superior to an unstable, painful MCP joint ( Fig. 43.7 ).
The decision to perform partial or total wrist fusion is seldom made in the acute setting unless there is extensive, unreconstructible loss of articular surface. Usually, this decision is deferred until late function and pain can be better assessed, at which time elective arthroplasty or arthrodesis can be performed. Studies have shown that as little as 5 to 10 degrees of flexion and 30 to 35 degrees of extension are needed for most activities of daily living. , When wrist-level amputation is required, preservation of some wrist motion can be incorporated into mechanical prostheses, and preservation of an intact distal radioulnar joint can significantly improve pronation and supination under loading conditions. The functional benefit of preserving the distal radioulnar joint in a wrist-level amputation, although attractive in theory, has never been proven in practice.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here