Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Ultrasound is the most widely used imaging test in early pregnancy. Confirmation of a live intrauterine pregnancy requires sonographic identification of an intrauterine gestational sac with an embryo exhibiting cardiac activity. Other disorders such as failed intrauterine pregnancy, ectopic pregnancy, gestational trophoblastic disease, pelvic inflammatory disease, and endometriosis may complicate the ultrasound examination. The ultrasound examination is best interpreted in conjunction with the result of a pregnancy test, which helps distinguish among these possibilities. The practice guidelines for performing sonography during the first trimester are described in Chapter 12 . The current chapter focuses on the interpretation of ultrasound images in first-trimester intrauterine pregnancy, in ectopic gestations, and in gestational trophoblastic disease.
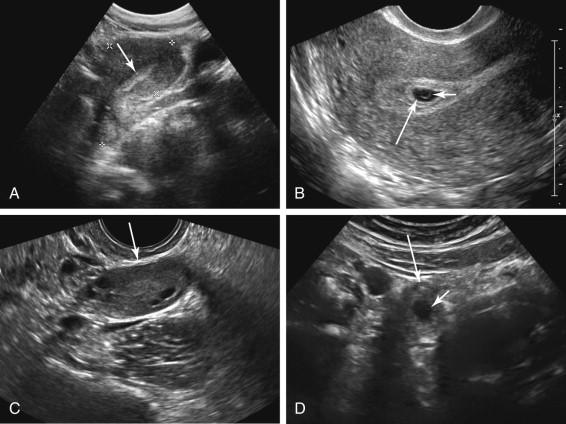
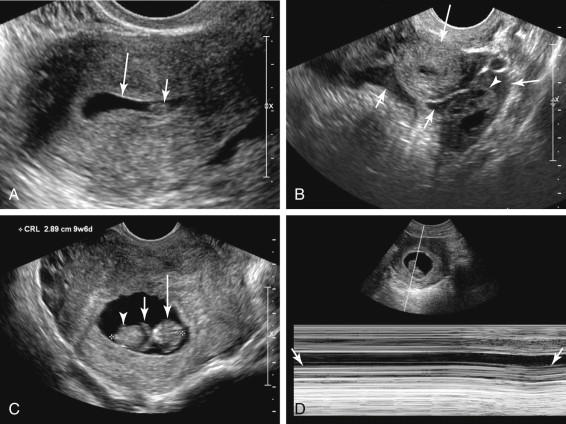
First-trimester sonography is generally performed by transabdominal (TA) and/or transvaginal (TV) approaches. The TV approach provides superior resolution compared with TA sonography, aiding in the identification and characterization of structures incompletely characterized or too small to be visualized transabdominally. For example, the improved detail afforded by TV sonography facilitates visualization of the early intrauterine pregnancy before it can be seen at TA ultrasound, potentially converting a result of pregnancy of unknown location at TA scanning to a definitive diagnosis of an intrauterine pregnancy with the addition of TV imaging ( Fig. 14-1A and B ). By contrast, the TA approach provides an overview of pelvic structures and facilitates visualization of processes located high in the pelvis, beyond the field of view of the TV probe. A superiorly located ectopic pregnancy may be missed at TV scanning because it is beyond the field of view and can be seen only at TA sonography (see Fig. 14-1C and D ). If the TA study shows a live intrauterine pregnancy and normal appearing adnexa or detects a live ectopic pregnancy, the study can typically be ended without necessitating addition of TV sonography. If TA ultrasound does not provide definitive proof of a live intrauterine pregnancy or an ectopic pregnancy, TV sonography should be performed when possible. The TA study is also important to look for findings outside of the pelvis, in particular free abdominal fluid due to hemoperitoneum in the setting of a ruptured ectopic pregnancy.
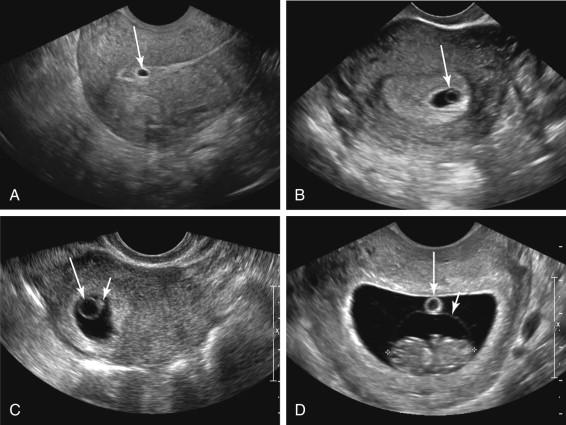
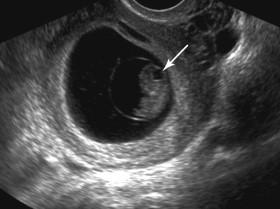
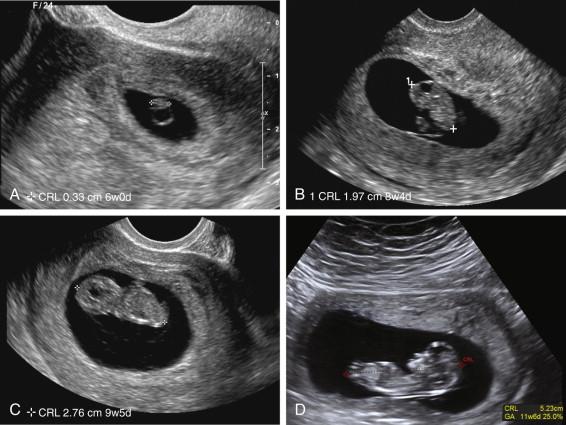
The gestational ages cited in the following discussion apply to TV sonography; the corresponding gestational ages using TA scanning would be higher. The gestational sac is the first structure identified in the uterus of an early pregnancy. A small gestational sac is generally visible at approximately 5 weeks gestation ( Fig. 14-2A ). The next structure visualized is the yolk sac, identified at approximately 5½ weeks. The yolk sac is depicted as a small, echogenic ring in the gestational sac (see Fig. 14-2B ). The embryo is not visualized until after the yolk sac is at approximately 6 weeks gestation. The embryo is first identified as a focal thickening along the outer margin of the yolk sac (see Fig. 14-2C ). Later in the first trimester, the yolk sac separates from the embryo and is found in the chorionic cavity, outside the amnion (see Fig. 14-2D ). In the majority of normal pregnancies, embryonic cardiac activity is identified almost as soon as the embryo is visualized ( ![]() , also see ). Cardiac activity should be documented with M mode or video clips, not Doppler. Doppler is associated with increased power exposure to the embryo and is not necessary to confirm cardiac activity (which can be reliably done with M mode and video clips). Consequently neither color Doppler nor spectral Doppler should be used to assess for cardiac activity in the early pregnancy.
, also see ). Cardiac activity should be documented with M mode or video clips, not Doppler. Doppler is associated with increased power exposure to the embryo and is not necessary to confirm cardiac activity (which can be reliably done with M mode and video clips). Consequently neither color Doppler nor spectral Doppler should be used to assess for cardiac activity in the early pregnancy.
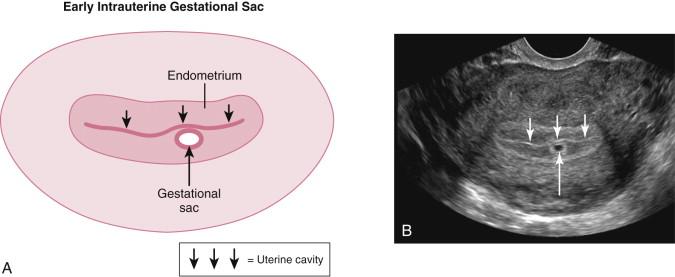
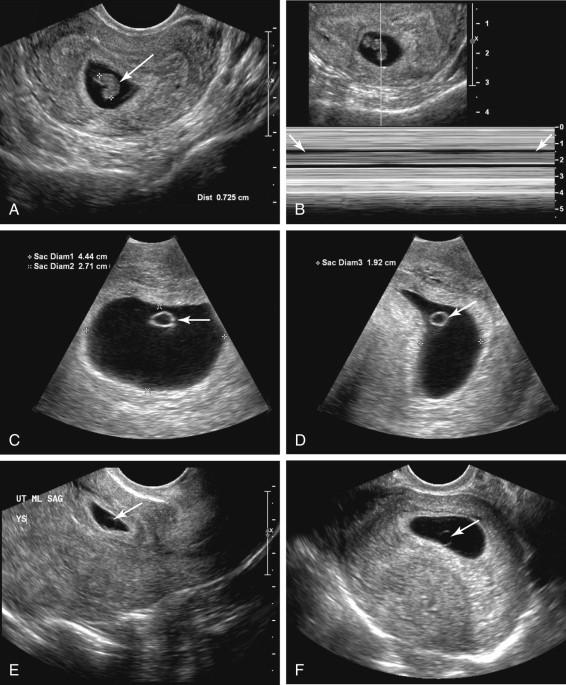
In the absence of an identifiable yolk sac or embryo, an intrauterine fluid collection should be assessed to determine whether it is an intrauterine gestational sac or a pseudogestational sac secondary to an ectopic pregnancy. An intrauterine gestational sac is likely when sonography reveals a small, rounded collection eccentrically located immediately adjacent to the uterine cavity, surrounded by a well-defined, thick, peripheral rim of echogenic tissue ( Fig. 14-3A and B ). This appearance has been termed the intradecidual sign.
Another pattern that favors an intrauterine gestational sac, termed the double decidual sac sign, is found slightly later in the first trimester than the intradecidual sign. The double decidual sac sign is composed of three discrete layers of echogenicity that surround much of the gestational sac. It is attributable to eccentric implantation of the gestation into the endometrium on one side of the uterine cavity. As the sac grows it deforms the uterine cavity, causing it to assume a curved configuration. An echogenic layer of decidual tissue develops on both sides of the uterine cavity and the uterine cavity is seen as a hypoechoic layer in between the curved echogenic lines ( Fig. 14-4A and B ). The inner echogenic layer (decidua capsularis) corresponds to the decidua immediately surrounding the gestational sac. The outer layer (decidua parietalis) corresponds to the decidualized endometrium on the opposite side of the uterine cavity from the gestational sac. The three-layer appearance is not seen at the site of implantation (decidua basalis).
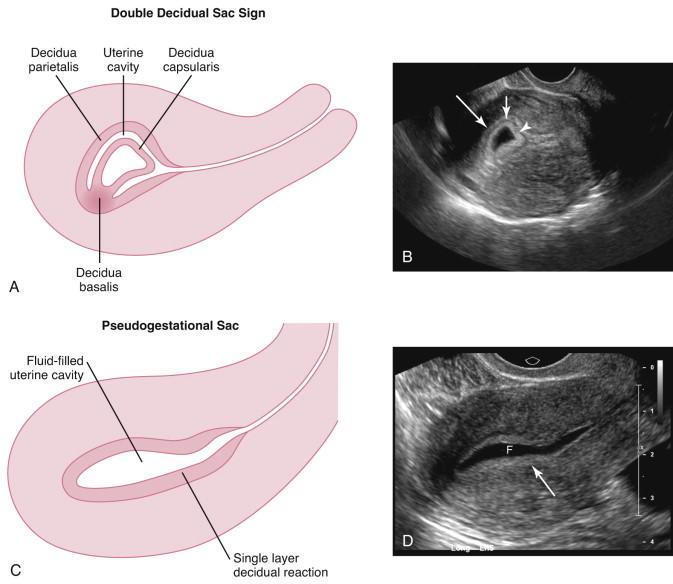
When an intrauterine fluid collection is secondary to an ectopic pregnancy, it is termed a pseudogestational sac. The fluid comprising a pseudogestational sac is located in the uterine cavity, not eccentric to the cavity as is the case with a true gestational sac, and is therefore only surrounded by a single echogenic layer (see Fig. 14-4C and D ).
There is substantial interobserver variability in identifying the double decidual sac and intradecidual signs. When clearly identified, these signs are very helpful in evaluation because a definitive intradecidual sign or double decidual sac sign strongly favors an intrauterine gestational sac. Failure to identify these features is not as useful, however, because nonvisualization does not exclude an early intrauterine pregnancy.
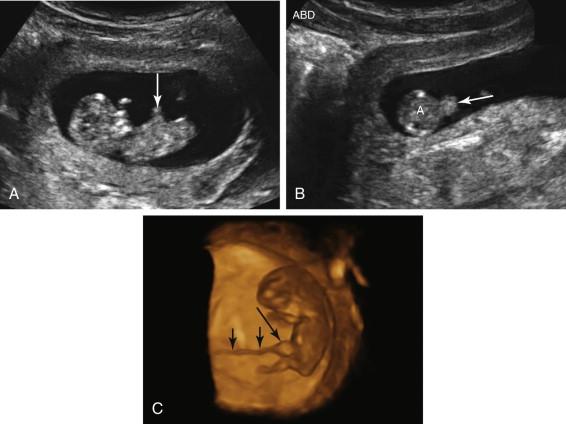
When the embryo is first visualized at approximately 6 weeks, it is difficult to identify embryonic anatomy or differentiate the crown from the rump. A pitfall that could lead to incorrect diagnosis of an intrauterine pregnancy in a patient with an ectopic gestation is visualization of an intrauterine fluid collection containing a small echogenic structure due to clotted blood or debris, mistakenly thought to correspond to a small embryo ( Fig. 14-5A and B ). It is important to identify cardiac activity early in the first trimester if the only evidence of an intrauterine pregnancy is visualization of a candidate embryo, because the normal early embryo has a nondescript appearance, without sonographically recognizable distinct body parts such as head, body, and limb buds. Later in the first trimester cardiac activity is not necessary for confirmation of an intrauterine embryo because it is unlikely that clotted blood or a conglomeration of debris could be mistaken for an embryo when more detailed anatomy with distinct body parts is seen (see Fig. 14-5C and D ). Lack of demonstrable cardiac activity at this stage of pregnancy is, however, consistent with embryonic demise: a nonviable pregnancy can be confirmed when the crown-rump length (CRL) is 7 mm or greater and no cardiac activity is seen.
The normal embryo grows in a predictable fashion. By approximately 7 weeks, the head and body can be distinguished. An increasing number of anatomic features become visible as the first trimester progresses. By the end of the first trimester the fetal bladder, stomach, choroid plexus, four extremities, and abdominal cord insertion are often visualized (see Fig. 12-8 ).
Two anatomic features seen during normal embryogenesis merit special attention because they can potentially be confused with pathology. Physiologic gut herniation is identified beginning at approximately 8 weeks and is depicted as a focal, rounded, solid structure at the base of the umbilical cord, corresponding to normal midgut herniation ( Fig. 14-6 ). Physiologic gut herniation should not be mistaken for an omphalocele. Normal midgut herniation is smaller than the remaining fetal abdomen, measures less than 7 mm in diameter, and is seen at the base of the umbilical cord. It returns to the abdomen by 12 weeks, after which it is no longer visualized. During embryologic development of the hindbrain, a cystic structure is identified in the posterior position of the head, which is related to development of the rhombencephalon ( Fig. 14-7 and ![]() ). This cystic area is usually seen from approximately 7 to 10 weeks and has a characteristic appearance, which should not be mistaken for a brain abnormality such as anencephaly, a choroid plexus cyst, or a Dandy-Walker malformation. Because physiologic midgut herniation and the cystic space in the rhombencephalon are normal embryologic processes routinely seen at antenatal ultrasound when sought, they do not need to be described in the report when their appearance and timing are typical.
). This cystic area is usually seen from approximately 7 to 10 weeks and has a characteristic appearance, which should not be mistaken for a brain abnormality such as anencephaly, a choroid plexus cyst, or a Dandy-Walker malformation. Because physiologic midgut herniation and the cystic space in the rhombencephalon are normal embryologic processes routinely seen at antenatal ultrasound when sought, they do not need to be described in the report when their appearance and timing are typical.
One of the primary indications for sonography in the first trimester is to establish gestational age. The terms gestational age, embryonic age, fetal age, and menstrual age are used interchangeably and refer to the age of the pregnancy calculated from the first day of onset of the last menstrual period (LMP). Assignment of gestational age based on LMP assumes a regular 28-day menstrual cycle. Estimated gestational age by LMP is inaccurate in women with cycles of substantially different duration than 28 days, in women with irregular menstrual cycles, and when menstrual dates are uncertain.
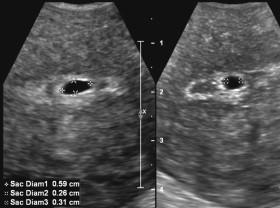
Measurement of the mean gestational sac diameter (MSD) is helpful in obtaining a rough estimate of gestational age before the embryo is visualized. The MSD is obtained by positioning the calipers along the inner wall of the gestational sac, obtaining three orthogonal measurements and averaging these dimensions ( Fig. 14-8 ). The MSD is not as accurate as the CRL in estimating gestational age. Once the embryo is seen, the CRL should be used in lieu of the MSD in this assessment. When both CRL and MSD are measured, some software packages default to averaging the gestational age predicted by CRL with that corresponding to MSD. Because CRL is more accurate than MSD, only the CRL and not a combination of MSD and CRL should be used to assign gestational age.
The CRL is measured along the long axis of the embryo from the top of the head (crown) to the bottom of the body (rump; Fig. 14-9 ). The embryo should be in a neutral position, without significant flexion or extension of the neck. A potential pitfall is mistaking the yolk sac for the head of the embryo and including it in the CRL, resulting in a spuriously large value (see Fig. 12-2B and C ).
A viable pregnancy is a gestation that can potentially result in a live infant. The terms failed pregnancy and pregnancy failure are frequently used to describe a nonviable pregnancy. Ultrasound plays an important role in distinguishing between viable and nonviable intrauterine pregnancies. The pregnancy should always be given the benefit of the doubt in making this distinction because reporting a nonviable pregnancy can lead to interventions such as pregnancy termination or administration of methotrexate, which can cause severe irreversible damage to the gestation. Even when ultrasound features favor a failed pregnancy, if there is even a slight chance it could be viable, this should be communicated and a failed pregnancy should not be reported.
Previously adopted sonographic criteria for diagnosing pregnancy failure were not stringent enough to ensure a potentially viable embryo would not be mistakenly described as nonviable. Earlier criteria have been recently modified. A review article in the New England Journal of Medicine (NEJM) describing findings of a multispecialty consensus conference by the Society of Radiologists in Ultrasound in October 2012 organizes ultrasound features, which may be seen in a failed intrauterine pregnancy, into two groups: those that are diagnostic of nonviable pregnancy and those that are of concern but not diagnostic of nonviable pregnancy.
Embryonic demise can be diagnosed when cardiac activity is not identifiable on TV ultrasound and the CRL is 7 mm or larger ( Fig. 14-10A and B , Box 14-1 ). This is a change from the previously widely adopted threshold of 5 mm, which was sometimes dubbed five and alive. It is unusual for an embryo with no identifiable cardiac activity and a CRL of 5 mm or larger to subsequently be shown to be viable, but recently published studies have reported a few embryos with CRL between 5 and 7 mm that subsequently exhibited cardiac activity. If cardiac activity is not seen in an embryo with a CRL less than 7 mm, follow-up ultrasound should be performed to assess for viability.
Single study:
CRL 7 mm or larger with no cardiac activity
MSD 25 mm or larger with nonvisualization of embryo
Follow-up sonogram:
No embryo with cardiac activity:
2 weeks or more following visualization of the gestational sac without yolk sac
11 days or more following visualization of the gestational sac with yolk sac
CRL, Crown-rump length; MSD, mean gestational sac diameter; TV, transvaginal; US, ultrasound.
A second criterion for diagnosing a nonviable pregnancy is failure to identify an embryo when the MSD is 25 mm or larger (see Fig. 14-10C and D ). A previously used threshold of 16 mm is not stringent enough because there have been reports of pregnancies with MSD between 16 and 21 mm, in which initially there was nonvisualization of an embryo, but a live pregnancy was subsequently seen. The current threshold of 25 mm was set higher than 21 mm as an added precaution to give the pregnancy the benefit of the doubt and allow for the wide interobserver variation in measurement of the MSD.
Two other ultrasound criteria considered diagnostic of pregnancy failure rely on findings on a follow-up sonogram performed after a predetermined amount of time elapses following an initial study. Failure to identify an embryo with cardiac activity following an interval of 2 weeks or more after an ultrasound that demonstrated a gestational sac but no yolk sac is considered diagnostic of a nonviable pregnancy. Similarly, failure to identify an embryo with cardiac activity after an interval of 11 days or more following an ultrasound that depicted a gestational sac and a yolk sac is also considered diagnostic of a nonviable pregnancy (see Fig. 14-10E and F ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here