Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
THE PREMATURE INFANT IS DEFINED as birth before 37 weeks gestation. Premature births can be classified as low-birth-weight (LBW) infants (<2500 g), very low-birth-weight (VLBW) infants (<1500 g), and extremely low-birth-weight (ELBW) infants (<1000 g). Alternatively, they may be classified as moderate to late prematurity (32 to <37 weeks), very premature (28 to <32 weeks), and extremely premature (<28 weeks). A neonate is an infant in the first 28 days after birth. “Premies” are commonly referred to as infants rather than neonates as a group because gestation may be very short (e.g., 24 weeks) and thus even at 37 weeks postmenstrual age (PMA), they are truly infants with a postnatal age of 13 weeks (24 + 13 = 37). These infants should be labeled with both gestational age (i.e., at birth) and postnatal age (i.e., age after birth). The use of current postconception age (PCA) or PMA (approximately 10 days older) helps define maturation of physiologic processes.
Morbidity and mortality in this population has decreased considerably compared with 30 years ago, especially in ELBW infants. This decrease is the result of many factors, including the development of specialized maternal fetal medicine and neonatal care units, antenatal corticosteroid administration, surfactant use shortly after birth, increased cesarean deliveries, and implementation of strategies to reduce lung injury, such as decreased delivery room intubations and increased use of continuous positive airway pressure (CPAP). Although survival and morbidity-free survival rates continue to increase, the trend over the past 20 years has plateaued. The cost of care is escalating, as are the number of surgical procedures and the need for specialized care these infants require. The first part of this chapter will focus on the VLB and ELBW infant, or “micropremie,” and discuss developmental physiology and its impact on anesthetic care.
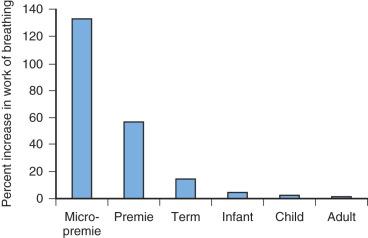
The anatomic differences of the pediatric airway are detailed in Chapter 14 ; however, there are specific challenges unique to the airway of the premature infant that must be taken into consideration. The small airways predispose the micropremie to obstruction and difficulty with ventilation. Resistance to airflow is inversely proportional to the fifth power of the radius in the upper airway and to the fourth power of the radius beyond the fifth bronchial division (see also Fig. 14.7 ). As a result, insertion of an endotracheal tube (ETT) increases resistance and work of breathing far greater for the micropremie (2.5- or 3-mm inside diameter [ID]) than for a larger infant (4 mm ID), child (5 mm ID), or adult (7 mm ID) ( Fig. 37.1 ). Similarly, partial occlusion of the ETT by secretions, blood, or kinking increases the work of breathing to a much greater extent in the micropremie. Partial occlusion of the natural airway from loss of muscle tone during anesthesia and sedation also increases the work of breathing more in the micropremie. Consequently, general anesthesia often requires placement of an ETT to ensure airway patency and provide assisted ventilation to overcome the increased work of breathing.
Diseases that narrow the airway, such as subglottic stenosis, tracheal stenosis, and tracheobronchomalacia, occur commonly in the micropremie, and the associated reduction in airway diameter further increases both resistance to airflow and work of breathing. Subglottic stenosis necessitates the placement of a smaller ETT than would otherwise be placed, further increasing airflow resistance. Although tracheal stenosis near the carina may not necessitate a smaller ETT, it still increases airway resistance from the stenosis distal to the ETT. With tracheobronchomalacia, the intrathoracic airways collapse during exhalation, again increasing resistance and the work of breathing (see also Figs. 14.10 and 33.10 ). Positive end-expiratory pressure (PEEP) or CPAP helps stent open the airway. Mechanical ventilation, rather than spontaneous ventilation during anesthesia, prevents fatigue from increased work of breathing, and maintains ventilation and oxygenation. During anesthesia, the use of smaller inspiratory-to-expiratory ratios prevents air trapping and hyperinflation of lung segments.
The cardiopulmonary system of the neonate is driven by the need to deliver sufficient oxygen (O 2 ) to maintain a high metabolic rate. The O 2 consumption of an average neonate is 5 to 8 mL/kg per minute, whereas that of an adult is 2 to 3 mL/kg per minute ( Table 37.1 ); the O 2 consumption rate in the premature infant is nearly 3 times that in the adult. It is this enormous O 2 consumption rate that explains the rapid decrease in blood O 2 partial pressures in the neonate during periods of hypoventilation. Although ventilatory gas exchange volume is nearly 10-fold greater in adults than in neonates, the tidal volume relative to body weight for both is approximately equal (6 mL/kg). In neonates, increasing the respiratory rate facilitates the elimination of carbon dioxide (CO 2 ) generated by their relatively high metabolic processes; alveolar ventilation is approximately 130 mL/kg per minute in the perinatal period, compared with 60 mL/kg per minute in adulthood.
| Variable | Infants | Adults | Infant/Adult Ratio |
|---|---|---|---|
| Oxygen consumption (mL/kg per minute) | 5–8 | 2–3 | 2 |
| Respiratory rate (breaths/minute) | 40–60 | 12 | 3–5 |
| Tidal volume (mL/kg per minute) | 6–8 | 7 | 1.0 |
| Total lung capacity (mL/kg) | 53 | 85 | 0.6 |
| Airway diameter (mm) | |||
| Trachea | 5 | 14–16 | 0.3 |
| Bronchus | 4 | 11–14 | 0.3 |
| Bronchiole | 0.1 | 0.2 | 0.5 |
The structure and function of the immature lung predisposes to alveolar collapse and hypoxia. The premature alveoli are primarily composed of thick-walled, fluid-filled saccular spaces that are surfactant deficient and require greater pressures to initially expand. Production of surfactant by type II alveolar pneumocytes begins between 23 and 24 weeks gestation, although surfactant concentrations often remain inadequate until 36 weeks gestation. These factors lead to the development of respiratory distress syndrome (RDS), which causes reduced lung volumes and lung compliance, increased intrapulmonary shunting, and ventilation-perfusion mismatch. It is clinically characterized by grunting respirations, nasal flaring, and chest retractions that develop shortly after birth. Decreased lung volumes and ventilation-perfusion mismatch may also occur as a consequence of anesthesia. The effects of immature structures, disease, and anesthesia on lung function all increase the risk of hypoxia during surgery and anesthesia.
In neonates, atelectasis might also be caused by anatomic forces that decrease lung volume. For example, the relatively large abdomen in a neonate displaces the diaphragm cephalad, placing the closing capacity within the expiratory reserve volume (see also Fig. 2.5 ). Moreover, increases in intraabdominal pressure from gastric distention associated with overzealous assisted ventilation with a face mask, replacement of bowel in the abdomen during repair of gastroschisis or omphalocele, or surgical retraction or manipulation of the abdominal contents also might shift the closing capacity to within the infant's expiratory reserve volume. The resulting atelectasis and intrapulmonary shunting may require controlled ventilation with PEEP to recruit closed lung units and improve oxygenation, emptying of the stomach, or changes in surgical maneuvers.
Micropremie lungs are particularly susceptible to volutrauma. Mechanical lung injury is no longer thought to be caused by the use of high peak-inspiratory pressures, but rather related to increased end-inspiratory lung volumes and frequent collapse and reopening of alveoli. A ventilation strategy using small tidal volumes (4–6 mL/kg), greater respiratory rates, PEEP sufficient to avoid alveolar collapse, and permissive hypercapnia reduces lung injury in the premature lung. Permissive hypercapnia (arterial partial pressure of CO 2 [Pa co 2 ] 45–55 mm Hg) results in smaller periods of assisted ventilation and reduced incidence of bronchopulmonary dysplasia (BPD), without an increase in adverse neurodevelopmental outcomes.
BPD is an important chronic lung disease of prematurity, defined as the need for supplemental oxygen at 28 postnatal days. Traditionally, BPD has been associated with premature infants subjected to high levels of O 2 and ventilation therapy that causes a lung injury–induced increase in cytokine activation. Other factors that increase the risk for developing BPD include chorioamnionitis and the persistence of a hemodynamically significant patent ductus arteriosus (PDA).
Alveolarization begins around 36 weeks gestation. Therefore lung injury in the premature infant interrupts pulmonary maturation, resulting in larger but fewer alveoli than normal lungs. Decreased lung development in infants with BPD diminishes the surface area for pulmonary gas exchange, which increases O 2 requirements. Moreover, some infants with BPD have reduced lung compliance and increased airway resistance and hence have prolonged pulmonary time constants. Some infants with severe BPD have abnormal muscularization of the vessels in the periphery of their lungs, leading to pulmonary hypertension and right ventricular hypertrophy.
A number of strategies may be implemented to prevent the development of BPD. Modalities include antenatal corticosteroid administration to the mother and early postnatal administration to the infant, exogenous surfactant therapy, and specific ventilatory strategies, such as early and aggressive use of CPAP instead of intubation with positive-pressure ventilation. Treatment of existing BPD often requires ventilatory and medical therapies. Ventilatory goals should be aimed at the avoidance of intubation if possible, and the use of permissive hypercapnia and smaller tidal volumes in those whose lungs are intubated. Infants with BPD are often treated with diuretics to decrease pulmonary alveolar and interstitial edema. As a result of chronic furosemide treatment, metabolic abnormalities may exist. Hypercalciuria from furosemide may lead to secondary hyperparathyroidism and nephrocalcinosis in some infants. Hydrochlorothiazide and spironolactone produce less severe metabolic abnormalities. Bronchodilators such as aminophylline, albuterol, or ipratropium may be beneficial in reducing airway resistance in some infants with BPD, although data are conflicting. Finally, large doses of steroids, especially dexamethasone, provide relief for some infants with severe BPD that is refractory to other medical and ventilator therapies. However, dexamethasone may cause systemic hypertension, hyperglycemia, hypertrophic cardiomyopathy, and alteration of neurologic and pulmonary development in some children.
A severity index for BPD based on the need for supplemental oxygen and/or positive-pressure ventilation or nasal CPAP has been developed and shown to identify a spectrum of risk for adverse pulmonary and neurodevelopmental outcomes in preterm infants ( Table 37.2 ). Although this severity index has not been studied in the context of anesthetic risk, experience suggests that such infants requiring supplemental oxygen, positive pressure, or medications for reactive airways are at greater risk for perioperative pulmonary complications. Anesthetic goals include minimizing the inspired oxygen concentration and tidal volumes while maintaining adequate arterial oxygen saturation (Sa o 2 90%–94%) and ventilation (Pa co 2 50–55 mm Hg). The use of smaller tidal volumes decreases the risk of pneumothoraces and interstitial emphysema. Preoperative evaluation of infants with BPD requires a very careful history and physical examination, particularly focused on the pulmonary and cardiovascular systems.
| Gestational age | <32 weeks |
| Time point of assessment | 36 weeks postmenstrual age or discharge home, whichever comes first |
| Therapy with oxygen >21% for at least 28 days | |
| Mild BPD | Breathing room air |
| Moderate BPD | Need for <30% oxygen |
| Severe BPD | Need for ≥30% oxygen and/or positive-pressure ventilation or nasal continuous airway pressure |
Some prematurity-related diseases, such as retinopathy of prematurity (ROP) and BPD, have been associated with neonatal exposure to supplemental oxygen (hyperoxia). Oxygen toxicity from hyperoxia leads to the formation of reactive oxygen intermediaries that impair intracellular macromolecules, leading to cell death. The formation of oxygen free radicals also promotes an extensive inflammatory response, leading to secondary tissue damage and cell death. Oxygen-induced vascular endothelial growth factor (VEGF) signals disturbances associated with abnormal angiogenesis; it may be detected in both ROP and BPD.
Controversy exists over the optimal oxygen saturation to target in the premature infant. Two studies, the SUPPORT trial ( S urfactant, P ositive Pressure, and Pulse O ximetry R andomized T rial) from the United States and the BOOST II trial ( B enefits O f O xygen S aturation T argeting) from the United Kingdom, Australia, and New Zealand reported that a reduced oxygen saturation target range of 85% to 89% had a reduced incidence of ROP but an increased mortality compared with a target range of 91% to 95%. However, the COT ( C anadian O xygen T rial) and BOOST-NZ (BOOST New Zealand) trials found no significant differences in either death or disabilities among the two target ranges.
Recent evidence suggests a more graded approach according to gestational age, with increasing oxygen saturation targets with increasing age, rather than a generalized approach that aims to target a single goal. For example, one study suggested that an infant younger than 33 weeks should have an oxygen saturation target between 83% and 89%, whereas an infant between 33 and 36 weeks should have a goal between 90% and 94%. However, the optimal range for the graded approach is controversial, as well. Because of the possible increase in mortality, most practitioners use the 91% to 95% target range of oxygen saturation.
Micropremies possess a biphasic ventilatory response to hypoxia. Initially, ventilation increases in response to hypoxia, but after several minutes, ventilation decreases and apnea may ensue. The ventilatory response to CO 2 is decreased in the micropremie, and hypoxia further blunts this response. Anesthetic drugs depress the ventilatory responses to both hypoxia and hypercapnia. Hypoxia and hypercapnia occur commonly as a result of apnea and hypoventilation during emergence and recovery from anesthesia. Thus the combination of anesthetic effects and an immature respiratory control system (see also Fig. 14.11 ), as well as immature intercostal and diaphragmatic muscles, increases the risk of hypoxia, hypercapnia, and apnea in the postoperative period (see also Figs. 4.8 and 4.9 ).
Apneic episodes occur commonly in the micropremie but decrease with advancing PCA. PCA is defined as the sum of the conception age and the postnatal age. These apneic episodes usually involve both a failure to breathe (central apnea) and/or a failure to maintain a patent airway (obstructive apnea). Central apnea results from decreased respiratory center output, although it may be precipitated by abrupt changes in oxygenation, pulmonary mechanics, brain hemorrhage, hypothermia, or airway stimulation. Apnea may also occur without a precipitating event (i.e., idiopathic). Preterm infants with apnea do not increase ventilation in response to hypercapnia, compared with those without apnea, thereby delaying resumption of breathing and prolonging the apneic episode. During obstructive apnea, the airway becomes obstructed in the hypopharynx and larynx as a result of pharyngeal muscle incoordination. Anesthetic drugs may further decrease pharyngeal muscle tone, precipitating airway obstruction during recovery from anesthesia. The combination of anesthetic effects and immature respiratory control places the micropremie at risk for central and obstructive apnea for a prolonged period of time during recovery from anesthesia.
Not surprisingly, apnea occurs commonly after anesthesia and surgery in premature infants. Like apnea of prematurity, postoperative apnea may be central, obstructive, or mixed in origin. The term postoperative apnea usually means prolonged apnea (>15 seconds) or brief apnea accompanied by bradycardia (heart rate ≤80 beats/minute). Postoperative apnea typically occurs as a cluster of episodes over several minutes, with minutes of normal breathing in between the clusters. Bradycardia may occur with apnea, usually beginning at the onset of apnea and is not a response to hypoxia but likely a vagal-mediated response. Arterial oxygen desaturation usually follows the apnea, although many apneic episodes may not have any associated desaturation. Arterial desaturation is worse with obstructive apnea than with central apnea.
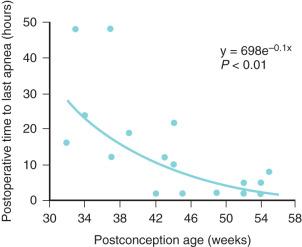
The incidence of postoperative apnea depends on PCA, hematocrit, and the type of surgical procedure ( Fig. 37.2 ; see also Fig. 4.7 and E-Fig. 4.5 ). The most significant risk factor is the PCA; the less the PCA, the greater the risk, with the incidence of postoperative apnea in the micropremie greater than 50%. Postoperative apnea can occur in the micropremie even without a history of apnea of prematurity. After the initial decrease in postoperative apneic events in premature infants occurs at approximately 44 weeks PCA, a second significant decrease to near that of full-term infants occurs at 60 weeks PCA. Therefore most centers have adopted a policy where premature infants need to be monitored for 12 continuous hours of apnea-free events after anesthesia when younger than 60 weeks PCA. Many admit these infants for overnight monitoring. Anemia (hematocrit <30%) and younger gestation increase the risk of apnea for a given PCA. Postoperative apnea usually begins within an hour of emergence from anesthesia. In the micropremie, it can continue to occur up to 48 hours postoperatively, despite the elimination of anesthetic agents (see Fig. 37.2 ). In fact, postoperative apnea can occur after surgery with desflurane- or sevoflurane-based anesthetics, or even after surgery for which a regional anesthetic was administered and no general anesthetic drugs were used. Although spinal anesthesia may reduce the incidence of apnea within the first 30 minutes in PACU, the incidence of late apnea is the same as that after general anesthesia. Postoperative apnea is more common after major procedures, such as a laparotomy, compared with peripheral surgical procedures, such as inguinal hernia repair. These observations indicate that the neurohormonal response to surgery and postoperative pain may play an important role in the origins of postoperative apnea.
Management of postoperative apnea includes close observation with a cardiorespiratory monitor and pulse oximeter, administration of intravenous (IV) methylxanthines, such as caffeine and theophylline ( Table 37.3 ), and prevention/treatment of anemia or hypovolemia. Caffeine is generally preferred over theophylline as it has a greater half-life and thus needs less frequent dosing (see also E-Fig. 4.6 ), its enteral absorption is more reliable, has fewer adverse side effects (tachycardia and feeding intolerance), and generally does not require serum drug monitoring. A loading dose of 10 mg/kg (IV or oral [PO]) is followed by a maintenance dose of 2.5 to 5 mg/kg daily. Aminophylline 5–10 mg/kg, a predrug of theophylline, can also be used intravenously. Apnea can be exacerbated by opioids in the premature neonate, so their avoidance, if at all possible, is recommended. Obstructive apnea often responds to changes in head position, insertion of an oral or nasal airway, or placing the infant in a prone position. Nasal CPAP, high-flow nasal prongs (HFNP), or tracheal intubation and mechanical ventilation may be required for several days postoperatively if these measures fail.
| Cause | Treatment |
|---|---|
| Central | Increase O 2 delivery |
| Increase fraction of inspired O 2 | |
| Increase hematocrit (?) | |
| Xanthine derivatives: | |
| Theophylline | |
| Caffeine | |
| Obstructive | Neck extension |
| Prone or lateral position | |
| Oral airway | |
| Nasal continuous positive-airway pressure |
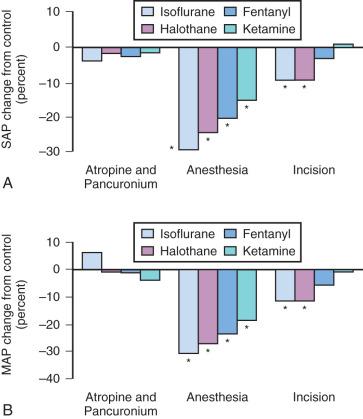
The micropremie remains at greater risk of cardiovascular collapse during anesthesia and surgery than does the full-term infant for several reasons. The fetal heart differs from the infant heart in that it has more connective tissue, less organized contractile elements, and increased dependence on extracellular calcium concentration. In addition, the less compliant fetal heart has a flatter Frank-Starling curve (see also Figs. 18.3 and 18.4 ) and is less sensitive to catecholamines because of near-maximal baseline β-adrenergic stimulation (see also Chapter 18 ). Consequently, cardiac output in the micropremie depends more on heart rate than it does in the term neonate. The increased resting heart rate in the micropremie also does not permit cardiac output to increase to the same extent as in an infant or child. Additionally, the vagotonic response caused by succinylcholine or its metabolites (succinylmonocholine) and synthetic opioids may lead to bradycardia. These cardiac reflexes can be offset by the vagolytic effects of pancuronium or atropine.
The micropremie has a greater blood volume per kilogram, but it has a smaller absolute blood volume ( Table 37.4 ). Therefore relatively little blood loss during surgery can cause hypovolemia, hypotension, and shock. Because autoregulation is not well developed in the micropremie, the heart rate may not increase with hypovolemia, and blood flow and oxygen delivery to the brain and heart may decrease with relatively little blood loss. Anesthesia blunts baroreceptor reflexes in the micropremie, further limiting the ability to compensate for hypovolemia. The combination of limited ventricular stroke volume reserve, an increased heart rate, small blood volume, and limited autoregulation predispose the micropremie to cardiovascular collapse during major surgery.
| Blood Volume (mL/kg) | Weight (kg) | Total Blood Volume (mL) | 25-mL Blood Loss Proportion of Total Blood Volume (%) | |
|---|---|---|---|---|
| Micropremie | 110 | 1 | 110 | 23 |
| Premie | 100 | 1.75 | 175 | 14 |
| Full-term neonate | 90 | 3 | 270 | 9 |
| Infant | 80 | 10 | 800 | 3 |
| Child | 70 | 20 | 1400 | 2 |
The lungs are not required for gas exchange in utero because the placenta performs this function. The fetal circulatory pattern consists of atria and ventricles working as units in parallel (see Fig. 18.2 ). As little as 10% of the fetal right ventricular output may circulate through the lungs. Most of the blood returned from the lower extremities and a portion of the umbilical venous blood supply passes into the pulmonary arteries and subsequently through the ductus arteriosus (DA) into the systemic circulation (see Chapters 16 and 18 ; Fig. 18.1 ). The superior vena caval blood supply circulates through the foramen ovale (FO) into the left atria and subsequently into the systemic circulation. With expansion of the lungs and increase in oxygen tension during the first breath, pulmonary vascular resistance decreases and blood flow to the lungs increases, matching perfusion with new ventilation. The increased oxygen tension and loss of prostaglandin E 2 -based relaxation are thought to result in closure of the DA. Any factor that increases pulmonary vascular resistance (e.g., hypoxia, hypercarbia, acidosis, and hypothermia) may cause the circulation to revert to a fetal circulatory pattern with shunting of deoxygenated blood from the right to the left side of the heart via a patent foramen ovale (PFO) or patent ductus arteriosus (PDA). This right-to-left shunting of blood explains in part why some infants remain hypoxemic despite ventilation with 100% O 2 after severe desaturation.
In addition to aeration of the lungs, the removal of prostaglandins from the placenta and release of vasoactive substances at birth cause the DA to constrict and functionally close around 12 to 24 hours after birth, with anatomic closure in 2 to 3 weeks. Failure of the DA to close at birth occurs in 1/2000 full-term births, but affects up to 60% of ELBW infants with the incidence increasing with decreasing gestational age. It is thought to be due to immaturity and failure of smooth muscle cells within the ductus to constrict, as well as immaturity of the lungs, which are responsible for metabolizing prostaglandins.
With the increase in systemic vascular resistance and decrease in pulmonary vascular resistance at birth, a PDA often results in significant left-to-right shunting of blood, causing excess pulmonary blood flow, congestive heart failure, and respiratory failure. Diastolic runoff of blood into the pulmonary artery leads to a widened pulse pressure (owing to low diastolic blood pressure) and risk of coronary ischemia. In a neonate with RDS or persistent pulmonary hypertension, right-to-left shunting across the PDA may occur, producing cyanosis. Paradoxical embolism is another concern with a PDA, as well as a PFO. Fluid restriction and diuretic therapy, often used to treat congestive heart failure from left-to-right shunting through a PDA, further increase the risk of hypotension during surgery. The use of nonsteroidal antiinflammatory drugs to close the PDA can also cause renal compromise.
Persistent pulmonary hypertension (PPHN) and refractory hypoxemia in neonates occurs in approximately 2/1000 live births. PPHN is diagnosed when right-to-left shunting of blood occurs through a PDA and/or PFO in the absence of other congenital heart disease. Right-to-left shunting results from the failure of the pulmonary vascular resistance (PVR) to decrease at birth, thus preventing the conversion from fetal to neonatal pulmonary blood flow. The exact etiology of PPHN is not understood, but has been attributed to a variety of factors, including increased muscularization of pulmonary arterial vessels, impaired endothelial release of nitric oxide (NO), increased production of vasoconstrictors (e.g., endothelin-1), and impaired VEGF. It can be associated with circumstances leading to perinatal distress (meconium aspiration, sepsis, asphyxia) or can be idiopathic, and rarely, genetic.
PPHN is suspected in severely hypoxic neonates who do not have a significant increase in postductal O 2 saturation despite mechanical ventilation with an increased fraction of inspired oxygen (F i O 2 ). A greater preductal versus postductal O 2 saturation supports the diagnosis because it reflects the extrapulmonary right-to-left shunting of deoxygenated blood via the PDA. An echocardiogram excludes the presence of a congenital heart defect as the cause of or a contributing factor in the pulmonary hypertension and/or right to left shunt. It is imperative to diagnose and treat PPHN in a timely fashion as the morbidity, including neurodevelopmental delay, cerebral palsy, deafness, blindness, and mortality are substantive. Premature infants tend to have worse outcomes and have more severe PPHN, requiring extracorporeal membrane oxygenation (ECMO) support earlier and more frequently than full-term neonates.
The American Heart Association and American Thoracic Society have published guidelines for the diagnosis and treatment of PPHN. Treatment strategies aim to maintain adequate systemic blood pressure, maximize oxygen delivery, and optimize ventilator management to protect lung volume and function. Normal lung expansion should be the goal of mechanical ventilation. Caution must be taken to avoid overdistending the lung, which can increase PVR. In cases of severe parenchymal lung disease, such as meconium aspiration, in which airway disease can lead to atelectasis and intrapulmonary shunt, PEEP and exogenous surfactant may be used to recruit alveoli. Although inspired O 2 is a potent vasodilator, maximum dilation of the pulmonary vasculature is achieved by relatively low levels of O 2 , and hyperoxia can potentiate lung injury. For these reasons, increasing the F i O 2 often does not improve gas exchange in PPHN. Acidosis causes pulmonary vasoconstriction and should be avoided in patients with PPHN. This led to the practice in the past of inducing alkalosis by hyperventilation of the lungs or by infusing sodium bicarbonate. However, there is no evidence of any long-term benefit with this approach, and such management has been shown to worsen pulmonary vascular tone and lead to worse neurodevelopmental outcomes. ECMO should be considered in those infants with severe sustained hypoxemia or compromised hemodynamic function.
Inhaled nitric oxide (iNO) is a selective pulmonary vasodilator used to treat PPHN. NO is normally produced by the endothelium and diffuses into subjacent smooth muscle cells, where it increases cyclic guanosine monophosphate (cGMP) levels that play a role in intracellular calcium levels and vasomotor protein function, leading to vascular relaxation ( Fig. 37.3 ). iNO decreases PVR, limiting right-to-left shunting of blood, increases systemic O 2 partial pressures, and reduces the need for ECMO support in neonates with pulmonary hypertension. However, not all infants respond to iNO, and studies have failed to demonstrate that iNO reduces mortality, length of stay in the hospital, or risk of neurodevelopmental impairment. In contrast to full-term neonates, the success of iNO in the micropremie with hypoxic respiratory failure and pulmonary hypertension remains unclear. Even among full-term neonates, some conditions such as congenital diaphragmatic hernia (CDH) do not respond well to iNO.
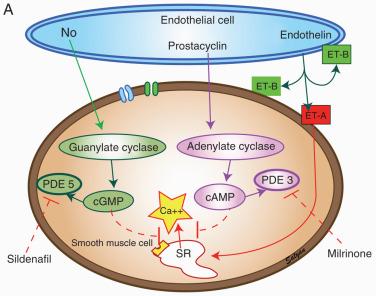
When iNO is administered, the optimal initial dose is 20 ppm ( Fig. 37.4 ). There is no advantage in terms of improvement in oxygen requirements to starting iNO at doses greater than 20 ppm. Moreover, doses greater than 20 ppm for extended periods may produce methemoglobinemia and/or nitrogen dioxide. Methemoglobin levels should be monitored if large concentrations of iNO are used. Fig. 37.4 delineates both treatment and weaning algorithms for iNO. Care must be taken to slowly wean the iNO to avoid rebound pulmonary hypertension. Weaning should cease if the oxygen requirements increase at any stage during the weaning process and resumed once the oxygen requirements stabilize. Some who encounter hypoxemia during weaning may benefit from phosphodiesterase inhibitors such as sildenafil or milrinone. Sildenafil (Revatio) is a phosphodiesterase-5 inhibitor that selectively reduces PVR. It has been recommended for PPHN that is refractory to iNO, although the US Food and Drug Administration (FDA) issued a blackbox warning in 2012 against chronic use of sildenafil in children. It may be administered orally or intravenously. Milrinone may also be added to treat infants with PPHN when left ventricular dysfunction is present. Prostacyclin-I 2 (e.g., epoprostenol IV or treprostinil oral, IV or subcutaenous) has been used to treat PPHN (as well as iNO-resistant PPHN); however, it has a very brief half-life (5 minutes) and requires permanent vascular access for continuous administration. Any interruption in therapy will rapidly result in profound rebound pulmonary hypertension with many untoward adverse effects. Inhaled prostaglandin-I 2 analogs (e.g., iloprost) and endothelin receptor antagonists (e.g., bosentan) may also be used in iNO refractory PPHN.
The central nervous system (CNS) is incompletely developed at birth. Regions of the CNS develop at different times during gestation; consequently, the impact of premature birth depends on gestational age at birth and the severity of cardiovascular, respiratory, and other postnatal stressors. The area of the brain most susceptible to injury in the micropremie is the periventricular white matter. The white matter consists of preoligodendrocytes, astrocytes, and neuronal axons. Late in the second trimester (24–27 weeks gestation), preoligodendrocytes and astrocytes multiply tremendously and most cortical and subcortical structures begin to develop. The periventricular white matter is perfused by arteries penetrating from the cortical surface and by lenticulostriate arteries from the circle of Willis. During this period, the periventricular white matter is particularly susceptible to neurologic injury as it is a “watershed region,” susceptible to poor perfusion and hypoxic-ischemic injury during hypotension, reduced cardiac output, hypoxemia, and hypocarbia.
Neural pathways responsible for the perception of pain develop during the first, second, and third trimesters (see also Chapters 2 , 44 , and 45 ). During the first trimester, peripheral sensory receptors and spinal reflex arcs mature, yielding the “withdrawal reflex” to non-noxious stimuli. Neurons that transmit nociception appear in the dorsal root ganglia at 19 weeks gestation, and afferent neurons from the thalamus reach the cortical subplate and cortical plate between 20 and 24 weeks gestation. However, it is not until early in the third trimester (29 weeks) that pathways between the thalamus and somatosensory cortex are functional. Significant controversy exists regarding the exact gestational age at which perception and memory of pain occur. The hormonal responses to pain and stress may be exaggerated in neonates, although the clinical significance of this has not been defined. Nevertheless, our approach in the micropremie is to administer anesthesia during surgery and provide pain management postoperatively.
The neonatal brain requires a larger percentage of glucose production because of the greater brain weight in proportion to body weight. Multiple animal models and clinical studies implicate hyperglycemia as detrimental to the adult brain during global and focal ischemia, such as with a cerebral or hypoxemic ischemic event and during cardiac surgery with deep hypothermic cardiac arrest. In contrast, hyperglycemia in neonates appears to protect the brain from ischemic damage or at the very least be less harmful than hypoglycemia. Studies in both neonatal rat and pig hypoxia-ischemia models observed less brain damage with greater glucose concentrations. Many mechanisms exist for this strikingly different outcome between neonates and adults. Relatively mild hypoglycemia is known to cause brain damage in preterm infants. Micropremies with critical illness are especially prone to hypoglycemia because they contain limited stores of glucose and consume glucose anaerobically. Thus the administration of dextrose-containing fluids (carefully controlled with an infusion pump to minimize wide serum glucose fluctuations) and close monitoring of blood glucose concentrations are vital during anesthesia. Mild or moderate hyperglycemia during surgery is best managed by reducing the rate of infusion of dextrose-containing solutions and not administering insulin, with its attendant risk of hypoglycemia.
Despite decreases in mortality in the micropremie, long-term neurologic and developmental disabilities remain common in this group and include cerebral palsy, cognitive deficits, behavioral abnormalities, as well as hearing and visual impairment. In a study of ELBW infants, only 25% were classified as “normally developed” at 5 years of age. Twenty percent exhibited major disabilities. Brain magnetic resonance imaging (MRI) has identified a spectrum of abnormalities in these infants. The most common abnormality is diffuse high signal intensity on T2-weighted imaging in the periventricular cerebral white matter. Diffusion-weighted imaging shows increased apparent diffusion coefficient values, indicative of increased water content and delayed white matter maturation, suggesting ischemia-reperfusion injury in periventricular white matter, which has activated microglia and damaged preoligodendrocytes. Damage to preoligodendrocytes impairs myelination of cerebral white matter axons and accounts for many of the fine motor, speech, and cognitive deficits. On MRI, tissue volumes in the basal ganglia, corpus callosum, amygdala, and hippocampus are reduced and correlate with smaller full-scale, verbal, and performance IQ scores. Collectively, these MRI findings indicate that different regions of the brain vary in their susceptibility to injury during development and that such injuries lead to specific long-term disturbances in neurocognitive function.
Intraventricular hemorrhage (IVH) occurs in as many as one-third of micropremie infants. Although an association has been noted between the incidence of IVH and fluctuations in blood pressure, it is difficult to confirm any causal relationship. The severity of IVH, as defined by head ultrasound, is graded as follows:
Grade 1: hemorrhage limited to the germinal matrix
Grade 2: hemorrhage extending into the ventricular system
Grade 3: hemorrhage into the ventricular system and with ventricular dilatation
Grade 4: hemorrhage extending into brain parenchyma.
Although micropremie infants with grade 3 or 4 IVH are more likely to exhibit severe long-term neurocognitive sequelae, even micropremie infants with grade 1 and 2 IVH display poorer neurodevelopmental outcomes compared with those without IVH. Early onset of IVH appears during the first day of life. Risk factors include fetal distress, vaginal delivery, reduced Apgar scores, metabolic acidosis, severe hypercapnia, and the need for mechanical ventilation. Late onset of IVH appears days to weeks after birth with contributing factors including RDS, seizures, pneumothoraces, hypoxemia, acidosis, severe hypercarbia, and the use of vasopressor infusions. Lack of autoregulation leading to rapid fluctuations in cerebral blood flow, cerebral blood volume, and cerebral venous pressure, as well as fragile cerebral blood vessels, appear to play a role in the development of IVH. Factors that may decrease the incidence and severity of IVH include administration of antenatal glucocorticoids or indomethacin. Indomethacin helps to blunt the hyperemic response to hypoxia, improve cerebral autoregulation, and promote microvessel maturation of the germinal matrix. Although indomethacin decreases the incidence and severity of IVH, there is no evidence that long-term outcomes are improved. Corticosteroids produce vasoconstrictive effects on fetal cerebral blood flow, protecting the fetus against IVH at rest and when challenged by conditions causing vasodilatation such as hypercapnia, leading to a significant reduction in IVH.
The micropremie is very susceptible to hypothermia. Heat loss occurs by four possible routes: radiation (39%), convection (34%), evaporation (24%), and conduction (3%). In the micropremie, evaporative heat loss and insensible fluid loss are increased because the epidermis has less keratin. Conductive and convective heat losses are also increased because the micropremie has little subcutaneous fat for insulation and a large surface area/mass ratio. Thermal regulation is not well developed in the micropremie. Even full-term neonates do not have the capability to shiver or sweat, relying instead on nonshivering thermogenesis. Nonshivering thermogenesis, which depends on brown fat stores (which do not develop until 26–30 weeks gestation), is decreased in the micropremie and regulation of skin blood flow is less efficient. During anesthesia, measures should be undertaken to minimize radiation and convective heat loss by warming the operating room (OR) to 80°F to 85°F (26.7°C–29.4°C) before the neonate arrives, and minimizing convective heat loss during transport (i.e., use a thermoneutral incubator or a warming mattress). The most effective means to maintain normothermia and to warm the micropremia is a forced-air warmer. Other strategies that may be useful to maintain normothermia include use of a warming pad on the operating table to reduce conductive heat loss, use of overhead heat lamps to reduce radiant heat loss, and keeping the skin dry to reduce evaporative heat loss. Additional strategies to reduce heat loss include using humidified gases in the ventilator circuit, covering the head, and warming IV and irrigation fluids before they are used. Temperature should be carefully monitored as overheating the infant may readily occur.
The kidneys are not fully developed at birth. Full-term neonates have a glomerular filtration rate (GFR) that is only 30% of normal adult rates owing to fewer nephrons and smaller glomerular size. In fact, the GFR does not reach normal adult values until approximately 1 year of age (see Figs. 7.11 and 7.12 ). Maternal transplacental transfer of creatinine in utero increases the creatinine level in the neonate for the first few days of life. The baseline plasma concentrations of creatinine increase with increasing prematurity and remain increased until approximately 3 weeks of age because of immature renal function and the consequent lower creatinine clearance compared with full-term infants. These factors affect the metabolism of many drugs in the neonate. The renal excretion of medications such as penicillin, gentamicin, and some neuromuscular blocking drugs (NMBDs) such as pancuronium may be prolonged, resulting in increased duration of action or the development of high blood concentrations. This effect is particularly important when administering medications to an extremely premature infant. Thus the use of NMBDs that do not require renal function are most advantageous (e.g., cisatracurium).
Very premature infants easily become hyponatremic because of reduced proximal tubular reabsorption of sodium and water and reduced receptors for hormones that influence tubular sodium transport. As many as one-third of ELBW neonates develop hyponatremia. Frequent assessments of the serum concentration of sodium and free water requirements are important during critical illness. Increased serum concentrations of potassium occur in premature infants during the first few days after birth. The increase results from a shift in potassium from the intracellular to extracellular spaces. These increases are greater as gestational age and birth weight decrease. Reduced cardiac output and urine production may further increase serum concentrations of potassium and predispose to cardiac arrhythmias.
The total body water content in neonates is greater than in infants, children, and adults. In a term infant, 70% of the body weight is water (see also Figs. 7.7 and 7.8 ). By 6 to 12 months of age, 50% to 60% of the body weight is water. In the premature infant 75% to 85% of the body weight is water. In general, the smaller the PCA of the neonate, the greater the percent of water present. Differences among the total body water, renal maturity, and serum protein concentrations in a neonate affect the volume of distribution of many medications. Because the volume of distribution of drugs confined to the extracellular fluid is increased, the initial doses of some medications (e.g., NMBDs, aminoglycosides) may be greater on a weight basis in neonates than adults to achieve the desired blood concentration. In contrast, because of immaturity of renal function, the interval between doses of these drugs must be increased.
The basic principles of fluid maintenance in neonates are similar to those in older children and adults. The highly variable body fluid composition, degree of renal maturity, neuroendocrine control of intravascular fluid status, and insensible fluid loss with age make precise estimates of fluid requirements in neonates challenging. Urine volume and concentration may be difficult to determine intraoperatively and may not always correlate with volume status. Moreover, blood pressure and heart rate may not correlate with intravascular volume status in premature infants, and anesthetics may mask subtle cardiovascular changes that occur with changes in intravascular volume. Increased insensible fluid loss, which often occurs in the OR environment, requires judicious titration of IV fluids. Congenital abnormalities (e.g., gastroschisis, omphalocele) may markedly increase insensible fluid loss through exposure of large mucosal surfaces. The use of humidified gas mixtures reduces insensible fluid loss through the respiratory tract. However, overzealous intraoperative administration of fluids can result in pulmonary complications and worsened third-spacing of fluids. It is recommended to use volume-controlled devices for fluid management, such as a Buretrol or an IV infusion pump, to ensure accurate fluid administration.
During the third trimester, calcium is delivered to the fetus from the mother via placental transfer, resulting in fetal hypercalcemia. At birth serum calcium concentrations decrease with the abrupt loss of maternal calcium and reach a nadir at 2 days. By the third day of life, the combination of parathyroid hormone (PTH) secretion, dietary calcium intake, renal calcium reabsorption, skeletal calcium stores, and vitamin D allow the serum calcium concentrations in the full-term neonate to return to normal.
Infants who are born prematurely do not benefit from the transfer of maternal calcium and are at greater risk for hypocalcemia after birth. In addition, premature infants experience hypocalcemia owing to hypoalbuminemia (reduces serum but not ionized calcium), limited oral intake, impaired secretion and response to PTH, increased calcitonin levels, and increased urinary losses as a result of increased renal excretion of sodium. Hypocalcemia has also been observed in nearly 40% of critically ill neonates. Causes of hypocalcemia in the latter population include PTH insufficiency and peripheral resistance to PTH, inadequate calcium supplementation, and altered calcium metabolism caused by transfusion with citrated blood products, bicarbonate administration, or diuretics (e.g., furosemide).
Calcium exists in the serum in three fractions: protein bound, chelated to bicarbonate, phosphate, and citrate, and free or ionized calcium (iCa 2+ ). The ionized fraction is the physiologically active component; however, there is not always a clear relationship between total serum calcium and iCa 2+ . The correlation is poor with hypoalbuminemia or acid-base disturbances, as seen in premature and critically ill neonates. Hypocalcemia is defined as a total serum calcium concentration less than 8 mg/dL (2 mmol/L) in full-term infants and less than 7 mg/dL (1.75 mmol/L) in premature infants. An iCa 2+ less than 4 mg/dL (1 mmol/L) defines hypocalcemia in both populations.
Hypocalcemia may be asymptomatic or accompanied by nonspecific symptoms such as neuromuscular irritability (myoclonic jerks, exaggerated startle, or seizures), tachycardia, prolonged QT interval, and decreased cardiac contractility. Diagnosis rests on the determination of total and iCa 2+ levels. Neonatal hypocalcemia is a feature of DiGeorge syndrome (chromosome 22q11.2 deletion), also known as velocardiofacial syndrome, secondary to underdeveloped or absent parathyroid glands. The syndrome also involves abnormal facial characteristics, cardiac defects, thymic hypoplasia, and cleft palate.
Symptomatic hypocalcemia may be treated with 90 mg/kg calcium gluconate or 30 mg/kg calcium chloride by slow IV infusion over 5 to 10 minutes while monitoring the electrocardiogram, as bradyarrhythmias may develop in response to rapid increases in the serum concentration of calcium. The IV site must also be closely monitored for extravasation of a calcium gluconate infusion, as it may cause tissue necrosis and subcutaneous calcification deposits. Alternatively, if calcium chloride is administered, it should be infused through a central IV line. If using an umbilical venous catheter (UVC), caution must be taken to ensure the tip of the catheter is in the inferior vena cava (IVC) because direct infusion into the portal system can cause hepatic necrosis. Maintenance calcium gluconate dosing is administered at 80 mg/kg per day for the first 48 hours, followed by 40 mg/kg per day for the next 24 hours, and then discontinued. The clinical response and serum iCa 2+ concentrations should be monitored. Treatment of hypocalcemia is not effective in the presence of hypomagnesemia. In such a situation, parenteral administration of supplemental magnesium and calcium and treatment of the underlying cause of hypocalcemia are necessary. Persistent hypocalcemia necessitates determination of magnesium, phosphorus, PTH, and vitamin D concentrations.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here