Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Physically challenged, physically disabled, and “disabled” athletes are terms often used to collectively refer to all groups of athletes competing in international competitions such as Paralympics and have an impairment that limits their ability to participate in athletic arenas within a manner considered “normal” for regulated sport. The impairment is not a “disability” in their selected sport, as these athletes have tremendous ability yet require adaptions to the sport regulations to compete with their impairment.
Impairment: any loss or abnormality of psychological, physical, or anatomic structure or function
Disability: any restriction imposed from an impairment that limits an individual’s ability to perform an activity within a manner considered “normal” for an able-bodied individual
Handicap (as defined by the World Health Organization): a disadvantage resulting from an impairment or disability that interferes with a person’s efforts to fulfill a role that is normal for that person; handicap is a social concept, representing social and environmental consequences of a person’s impairments.
Over 61 million disabled people in the United States.
Over 250,000 people in the United States with spinal cord injury (SCI).
Includes traumatic and nontraumatic.
A reported 17,000 new injuries per year; average age at injury is 43 years.
Sixty percent tetraplegia, 40% paraplegia.
Over 1,540,000 million people in the United States with limb loss.
Incidence of congenital limb deficiency is 60 per 100,000 live births.
People older than 65 years account for 19.4 per 1000 of those with limb loss.
Common comorbidities: diabetes, vascular, and malignancy.
Incidence:
Lower extremity amputation (LEA), diabetes, and younger than 30 years: 7.2%.
LEA, diabetes, and older than 30 years: 9.9%.
Dysvascular disease: 46.2 per 100,000 with limb loss.
Multiple sclerosis: 400,000 cases diagnosed in the United States each year.
Muscular dystrophies: new cases estimated at 250,000 each year in the United States; Duchenne muscular dystrophy (DMD) is one of nine types of muscular dystrophy.
First sports event for disabled athletes: 1888, Sport Club for the Deaf; Berlin, Germany.
First international competition: International Silent Games, 1924.
First international sports competition for people with various physical impairments: Stoke Mandeville Games for the Paralyzed, 1948.
Youth divisions, in addition to adult, for athletes with physical impairment: 1950s.
Physical impairment cannot require changes in rules of a sport, lowering of standards for achievement, or modification of a defined sport to accommodate athletes at the interscholastic, collegiate, or professional level.
Neither adaptive equipment nor physical impairment can impart danger or an advantage to athletes or others competing in that sport.
Football:
Since 1978, athletes with below-knee amputation (BKA) may participate in high school football with prosthesis.
Upper extremity amputation (UEA) is also allowed: if a UEA is a ball carrier and the prosthesis comes loose, the play is stopped immediately.
Check for final rules, as variance in application and competition governance.
National Federation of State High School Associations’ rules concerning contact sports:
Metal hinges restricted to lateral and medial; require covering.
No metal in front of knee unless appropriately padded.
Prosthesis wrapped with minimum of half-inch foam rubber or appropriate polyurethane.
Approval of physician associated with amputee care recommended.
Wrestling
Athletes with hearing loss have successfully competed with normal-hearing athletes; if hearing loss is >55 decibels in the better ear, qualifies for physically challenged.
Those with limb loss must weigh in with prosthesis, if used.
Paralympics
Includes athletes with 10 eligible impairment types: impaired muscle power, impaired passive range of motion, limb deficiency, leg length difference, short stature, hypertonia, ataxia, athetosis, vision impairment, and intellectual impairment.
Each Paralympic sport defines which impairment groups they allow for participation.
Athletes must meet minimum disability criteria to compete.
Systems used for athlete evaluation to allow for equitable competition using objective methods.
Sport-specific and may differ at international and local competitions.
May be through medical diagnosis or functional measurements.
Sport class: Paralympic classification system unique to each sport, with determination of impact of disability on their sport.
Athletes may reclassify during their career if disability progresses.
Adult: management of comorbid medical conditions, social isolation, functional status, and independence.
Youth: peer interaction, relationships, cognitive and coping skills, school accommodations.
Missed social/peer opportunities.
Constant change in size/fit of adaptive equipment.
Resource limitations: insurance benefits and Medicaid limits.
Counseling: assist athlete in redesigning athletic or career goals.
Financial needs: insurance coverage, equipment needs, cost of accessibility, changes to home.
Physical office facilities: Americans With Disabilities Act (ADA) criteria for accessibility.
Adjustable-height examination table.
Collaboration with other healthcare professionals (e.g., neurosurgeon, physiatrist, therapist, vocational rehab, psychologist, primary care physician, prosthetist, or orthotist).
Several US and international organizations address the needs of physically challenged athletes, for example, Move United ( https://www.moveunitedsport.org/ ).
Joint effort of Disabled Sports USA and Adaptive Sports USA with over 150 local chapters.
In addition, many cities have local organizations that provide athletic opportunities for disabled athletes.
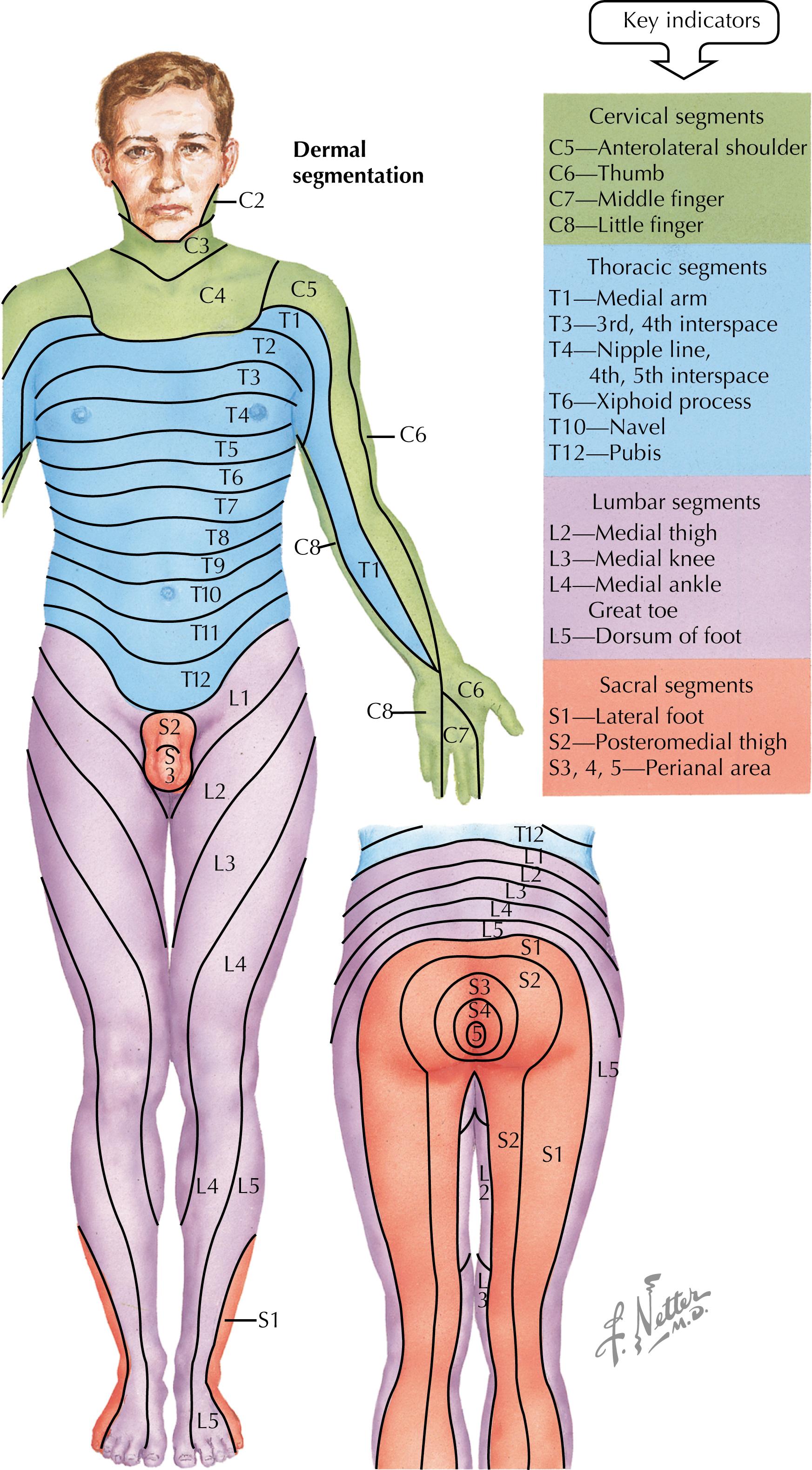
The American Spinal Injury Association (ASIA) has developed the ASIA Impairment Scale (AIS) assessment used to classify the severity of SCI ( Fig. 14.1 ).
Based upon the Frankel scale, ranging from A (complete) to E (return of normal function) measuring motor and sensory function at each neurologic level.
Cardiovascular changes:
Possible blunting of heart rate in response to exercise.
Cardiac repolarization abnormalities.
Decreased total peripheral resistance (increased vasodilation).
Decreased venous return, consequent decreased ability to respond to exercise stress.
Decreased reflexive regulation of blood flow.
Increased peripheral pooling.
Decreased oxygenated blood to exercising muscle.
Fatigue, limited aerobic endurance.
Pulmonary changes:
Limited pulmonary capacity, generally restrictive type (because of respiratory muscle weakness).
Paraplegics and people with high-level SCI can increase VO 2 max with exercise.
Dependent on intensity, frequency, and duration.
Musculoskeletal changes:
Kinetic chain disruption: loss of ground reactive force from lower extremity.
Stabilizing muscles become prime movers.
SCI level and completeness; chronicity, type, and etiology.
Medical history:
Concurrent with injury (e.g., traumatic brain injury [TBI], amputation, polytrauma).
Related to impairment (e.g., pressure sores, neurogenic bowel/bladder, neuropathic pain, spasticity, recurring urinary tract infection [UTI]).
Comorbid conditions: individuals with SCI have lower levels of physical activity and earlier onset of many chronic diseases (e.g., diabetes, hyperlipidemia, cardiovascular disease).
Surgical history: spinal fusion, muscle, tendon, or nerve transfers, surgically implanted medical devices.
Medications: antispasmodics, antiepileptics, tricyclic antidepressants, anticholinergics, baclofen pumps, pain medications, and bowel medications.
Level of functional independence: transfers, mobility, personal hygiene, bowel/bladder programs.
Equipment needs: sport-specific or general mobility.
Defined by uncontrolled hypertension with a systolic increase of greater than 20 mmHg, can be associated with bradycardia, flushing of the face, sweating, and/or nasal congestion.
May also be asymptomatic.
Medical emergency; typically occurs in patients with AIS level of injury at the sixth thoracic level (T6) and above.
No supraspinal inhibition.
Common causes include distended bowel or bladder, UTI, skin injury, fracture, tight clothes, or heterotopic ossification.
Treatment: sit patient up, treat blood pressure with fast-acting agent, and evaluate for and remove offending stimulus ( Box 14.1 ).
Sit person up, lower legs
Loosen clothing or constrictive devices
Check for and remove offending stimulus—bladder distension is most common
Bladder catheterization: 2% topical lidocaine jelly helpful
Check blood pressure every few minutes until patient stabilizes
1–2 inches of topical Nitropaste or immediate-release nifedipine 10 mg, bite and swallow
Repeat medicine in 15 minutes if no improvement
Continue to monitor blood pressure and symptoms for 2 hours after episode
If offending stimulus still present, recurrence of autonomic dysreflexia possible
Boosting: dangerous performance-enhancing technique used to purposefully induce autonomic dysreflexia (AD) during competition.
Performance enhancement through increased release of catecholamines.
Resulting from venous pooling in lower limbs.
Risk factors: recent SCI, obesity, trauma to pelvis and lower extremities, congestive heart failure, malignancy, tight garments below level of the lesion, and previous thromboembolism.
Prevention: passive stretching of limbs, graded pressure stockings, pharmacologic methods.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here