Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Management of ulnar nerve injuries is challenging given the distance required to reach the distal innervation targets of the ulnar nerve in the hand. Tendon transfers are indicated for patients with motor deficits without expected muscle endplate recovery. If growing axons are not expected to reach the endplates by 18 months after injury or muscle targets have been de-innervated for 1 year or longer, tendon transfers should be considered.
Common etiologies include delayed or failed ulnar nerve repair and chronic compression of the ulnar nerve at the wrist or elbow.
Procedures are tailored to individual patients and directed toward improving hand posture, alleviating clawing, strengthening key pinch, correcting small finger abduction, and improving grip by improving small and ring finger flexion at the distal interphalangeal (DIP) joint ( Table 65.1 ).
| Deformity/Problem | Surgical Procedure | Features |
| Claw hand deformity | FDS transfer to correct claw deformity |
|
| Claw hand deformity | FDS–lasso procedure |
|
| Claw hand deformity | MCP capsuloplasty/volar plate advancement |
|
| Claw hand deformity | Bony MCP joint arthrodesis |
|
| Weak thumb adduction | Long finger FDS-to-adductor transfer to restore thumb adduction Thumb adduction with ECRB with free tendon graft |
|
| Instability of the thumb IP joint | Partial FPL-to-EPL tenodesis stabilization |
|
| Loss of ring and little finger flexion | Extrinsic finger flexors—FDP side-to-side transfer |
|
| Instability of index finger | Index abduction-APL transfer using tendon graft |
|
With an ulnar nerve palsy, the hand assumes an “intrinsic minus” posture consisting of interphalangeal (IP) joint flexion and metacarpophalangeal (MCP) joint hyperextension. The deformity results from weakness of the intrinsic muscles in the setting of intact extrinsic finger extensors (innervated by the radial nerve) and flexors (flexor digitorum superficialis [FDS] innervated by the median nerve). Clawing is more pronounced in patients with low ulnar nerve injuries in which the flexor digitorum profundus (FDP) to the ring and small fingers remains innervated. Similarly, clawing may worsen among some patients with high ulnar nerve injuries that experience recovery as the innervation to the FDP of the ring and small fingers improves.
Clawing results in difficulty with grip because the coordination of joint flexion between the MCP and IP joints is lost. Clawing may be corrected using either dynamic techniques to establish MCP joint flexion in conjunction with proximal interphalangeal (PIP) joint extension or static techniques to reposition the MCP joint in flexion, depending on the competency of the extensor mechanism ( Fig. 65.1 ).
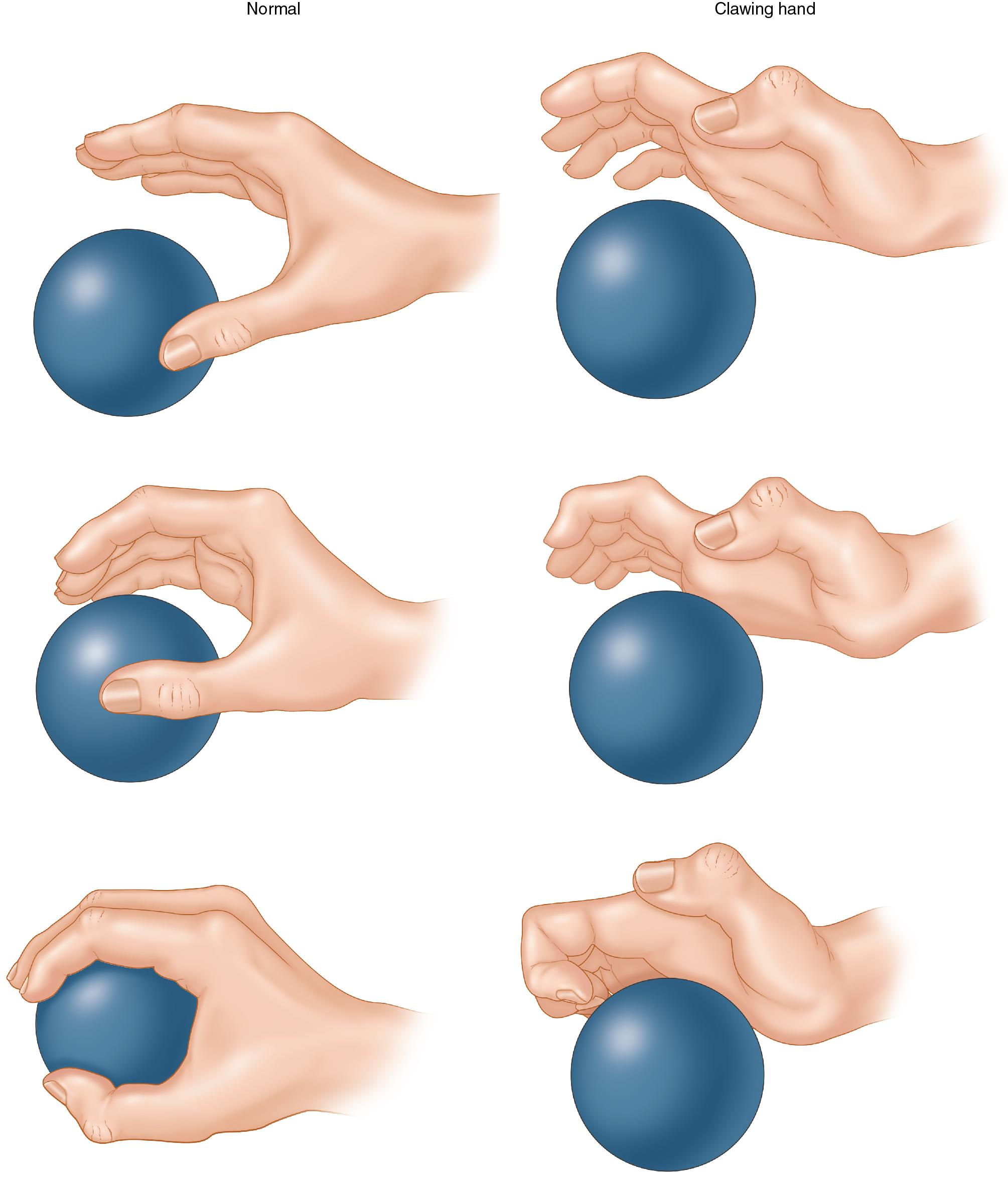
In general, a dynamic transfer using the FDS if preferred whenever possible. Static procedures are reserved for those patients for whom FDS is not available (e.g., high median nerve injury) or if the FDS is needed for reconstructive goals of greater priority. Other than fusion of the MCP joints of the fingers, static transfers may not be able to overcome the force of MCP hyperextension and invariably these static procedures will stretch out over time.
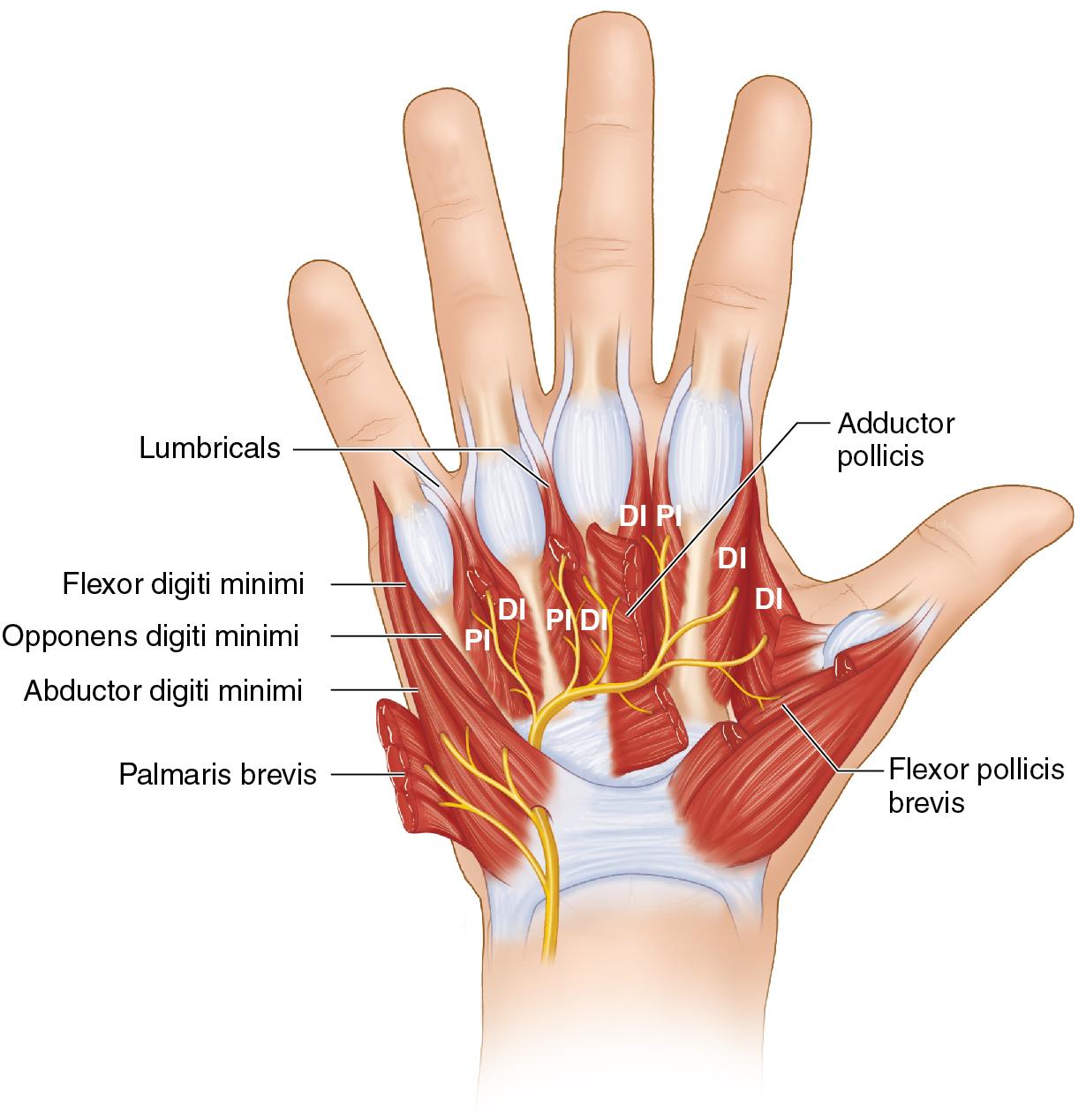
Key and tip pinch are weakened in patients with ulnar nerve palsy because of denervation of the adductor pollicis, flexor pollicis brevis (FPB), and first dorsal interosseous, and can be improved by transferring the extensor carpi radialis brevis (ECRB) augmented with a tendon graft to the thumb adductor.
Stability of the thumb IP joint can be created by either joint arthrodesis or by a split flexor pollicis longus (FPL), which regain pulp pinch to the side of the index finger.
Among patients with high ulnar nerve injuries, transfer of the median nerve innervated FDP tendon to the long finger can augment grip strength, which is weakened from denervation of the ring and small finger FDP.
Static procedures reposition the MCP joint in flexion to promote the extrinsic extensors to extend the PIP joint, and include volar plate advancement, FDS lasso around the A1 pulley, or MCP arthrodesis. Static procedures are conceptually simpler compared with dynamic procedures; however, volar plate advancement may stretch over time, with recurrence of clawing. MCP arthrodesis is typically reserved for patients with high median and ulnar nerve injury in which there is a lack of donor tendons, and it is technically demanding to achieve fusion of all four digits. Therefore, when possible, dynamic procedures are preferred and are described here.
Restoring thumb adduction power is frequently beneficial to patients. Augmenting index finger abduction, however, may only be selectively required. Frequently, patients can use the remaining digits to support the index finger as a post for pinch.
Stabilization of the thumb IP joint should be tailored to individual patients. A heavy manual laborer may benefit from additional strength, but many patients may need to flex their thumb IP joint during daily activities, such as when using a mobile phone.
Persistent joint contractures are a contraindication to tendon transfers. Patients must have full passive mobility of their fingers and thumb before surgery for transfers to be successful.
The extremity must be free from edema and the planned tendon routes should be without significant skin and subcutaneous scarring.
Tendon transfer should not be undertaken if there is pre-operative weakness of donor motor muscles. Donor muscles must be British Medical Research Council (BMRC) grade 4 or 5 before surgery, and loss of one strength grade is typical after transfer.
Progressive neurologic disease may preclude tendon transfer because the patient may continue to lose additional muscle function.
Patients that may be uncooperative with the postoperative immobilization and rehabilitation should not undergo surgery.
Common deficits among patients with ulnar nerve palsy include claw hand deformity, weak thumb key pinch, small finger abduction deformity, and loss of ring and small finger DIP joint flexion. Weak thumb key pinch is caused by adductor pollicis and first dorsal interosseous muscle denervation. The small finger is held in abduction because of intrinsic muscle paralysis that is overpowered by the extensor digiti minimi, which tends to extend and abduct the little finger because of the eccentric tendon insertion site, innervated by the radial nerve.
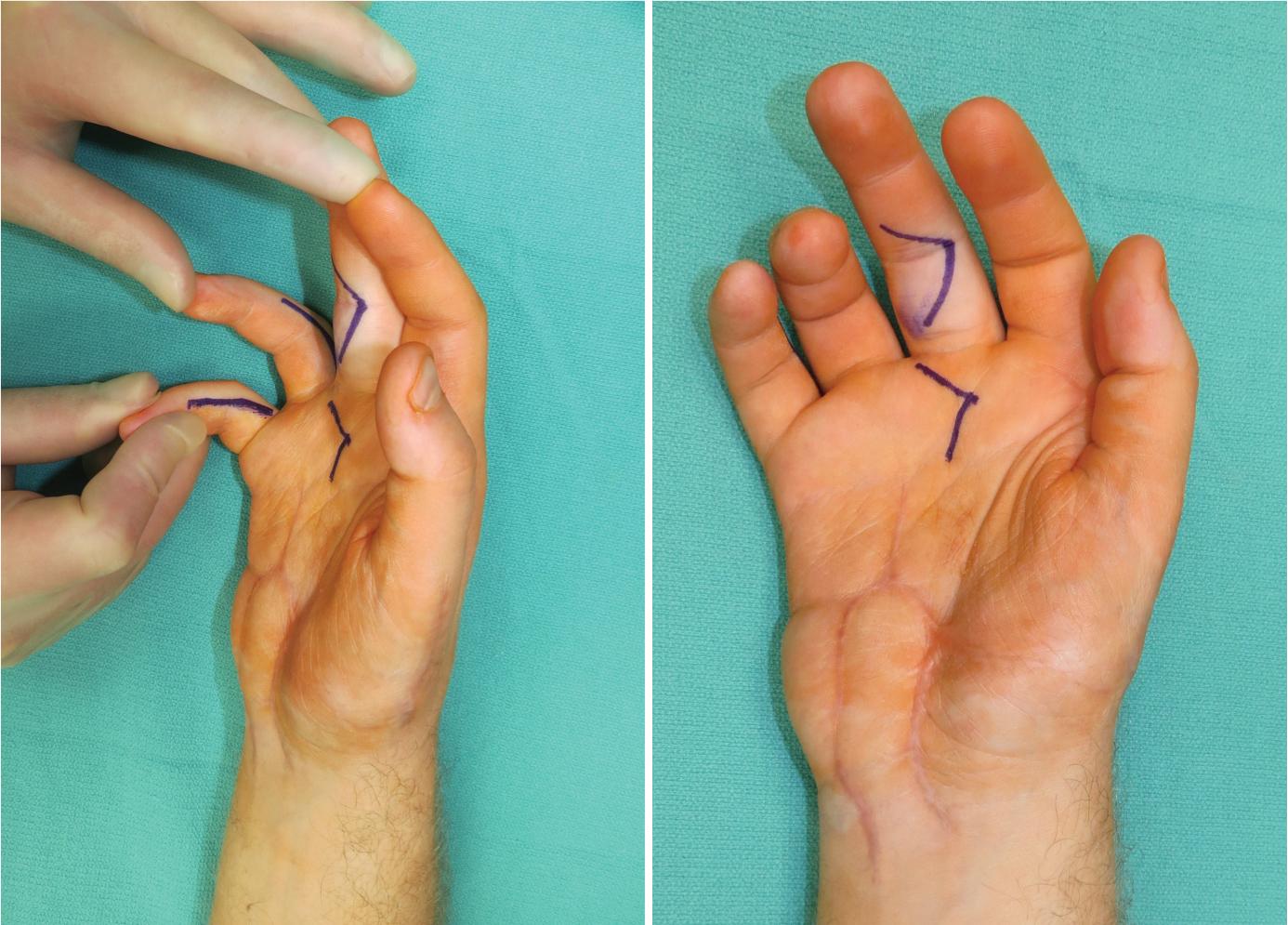
The Bouvier test examines the integrity of the extensor mechanism and is a critical guide when selecting tendon transfer procedures to correct clawing. To perform this test, the MCP joints are blocked in flexion, and the patient is asked to extend their fingers. If the extensor mechanism, specifically the central slip, is intact, the patient can actively extend the PIP and DIP joints (positive test). The test is negative if the patient is unable to extend the digits at the PIP and DIP joints with the MCP joints held in flexion ( Fig. 65.2A–C ).
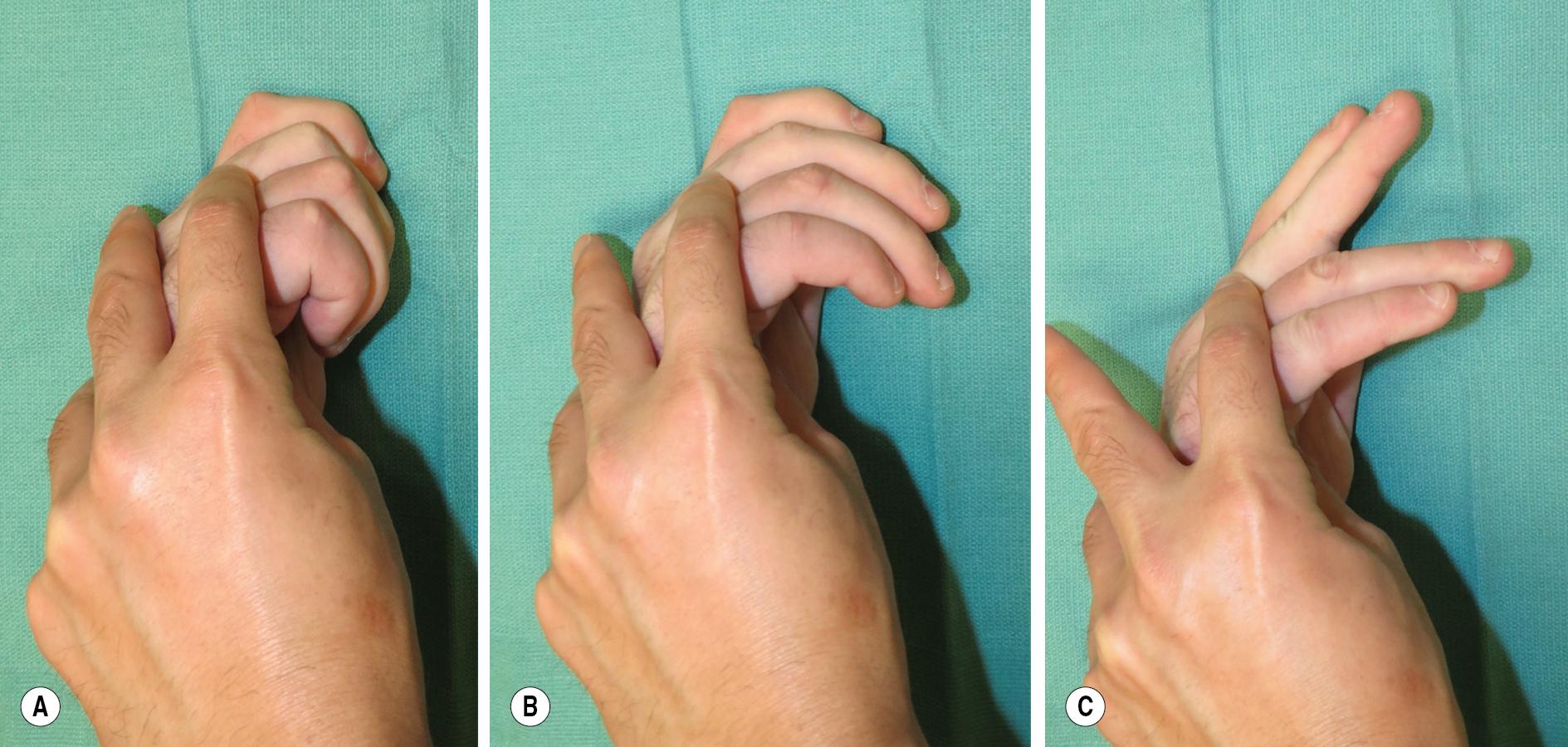
Patients with a positive Bouvier test (full extension at the PIP joints with the MCP joints flexed) are candidates for static procedures to correct MCP joint position. Patients with a negative Bouvier test but full passive extension with the MCP joint flexed require dynamic procedures to achieve PIP joint extension, given that the extensor mechanism is not competent. If possible, we prefer to perform the tendon transfer procedures regardless of the Bouvier test results.
Patients with PIP joint stiffness are not candidates for tendon transfer because passive joint flexibility is crucial to tendon transfer success. For these patients, joint contracture release and tenolysis should be performed first to achieve a mobile joint before the tendon transfer procedures.
Radiographs should be obtained to determine the presence of arthrosis at the MCP or PIP joints that may preclude full passive range of motion (ROM).
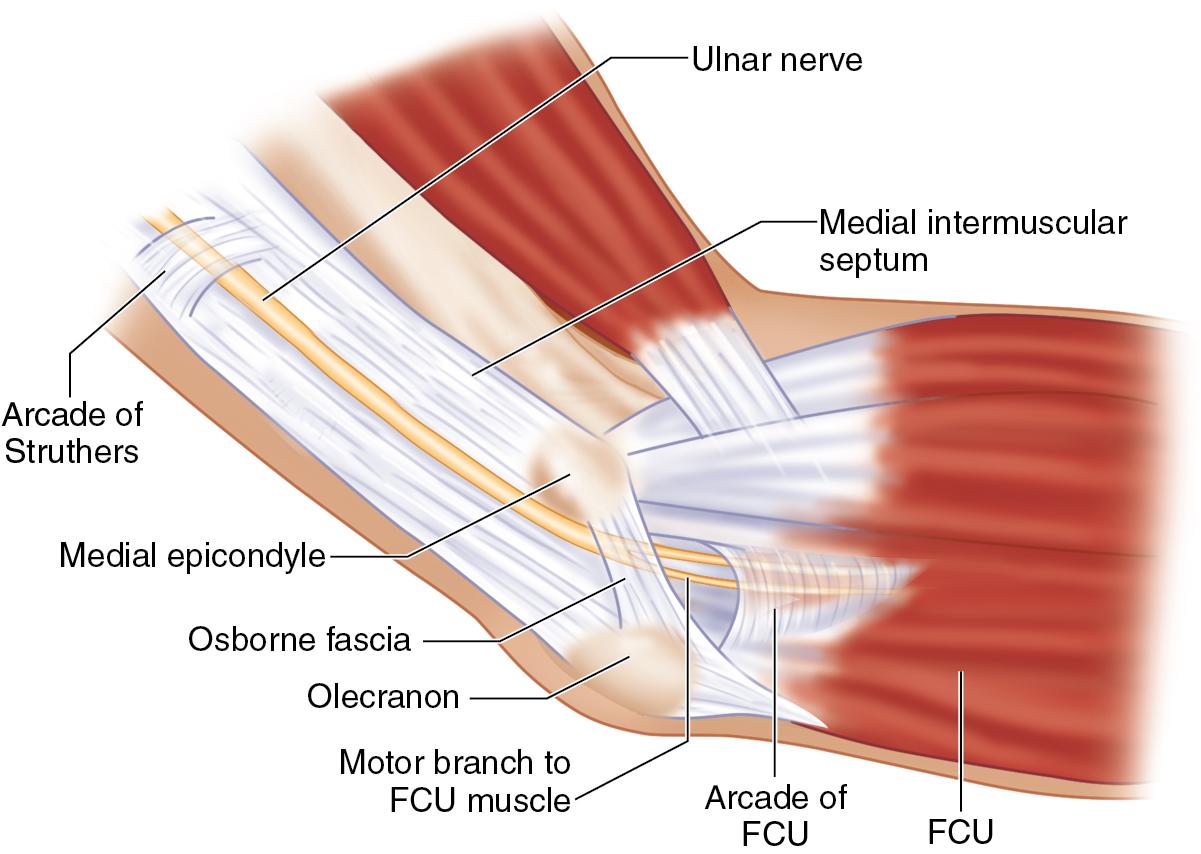
The ulnar nerve is the terminal branch of the medial cord. It courses subfascially through the upper arm in the bicipital groove posteromedial to the brachial artery. It pierces the intermuscular septum at the arcade of Struthers 8 cm proximal to the medial epicondyle to travel posteriorly around the elbow in the cubital tunnel ( Fig. 65.3 ). In the forearm, the ulnar nerve gives off the motor branches to the flexor carpi ulnaris (FCU) and to the FDP to the ring and little fingers just distal to the elbow, after the outlet of the cubital tunnel. These two muscles are affected in high ulnar nerve palsy patients only. The dorsal cutaneous branch arises approximately 5 cm proximal to the ulnar styloid and travels deep to the FCU to give sensation to the dorsoulnar hand. The palmar cutaneous sensory branch diverges from the ulnar nerve just proximal to the ulnar nerve entry into the Guyon canal. In the Guyon canal, the ulnar nerve divides into superficial sensory and deep motor branches. The motor branch controls the hypothenar muscles, the two ulnar lumbricals, the dorsal and palmar interossei, and the APB and gives partial innervation to the FPB ( Fig. 65.4 ).
The FDS is innervated by the median nerve and is commonly used for dynamic transfer to correct clawing.
Tendon transfer procedures are performed under tourniquet control, and the patient is positioned supine with the affected extremity extended on a hand table.
A Bruner zigzag incision is designed on the volar middle finger over the PIP joint for access to the FDS tendon. In addition, a midpalmar incision is made over the flexor tendons of the long finger, just proximal to the distal transverse palmar crease. Radial-sided midaxial incisions are designed over the ring and small fingers to access the common radial intrinsic tendons ( Fig. 65.5 ).
To correct clawing of the ring and small fingers, the FDS tendon of the middle finger, which is innervated by the median nerve, is selected for transfer. Skin incisions are made to expose the volar aspect of the PIP joint of the middle finger, and the skin and subcutaneous tissue are elevated above the flexor tendon sheath along the flaps designed using Bruner-style incisions.
The digital neurovascular bundles are identified using blunt dissection. While protecting them, the flexor tendon sheath is identified, and the pulley system is exposed ( Fig. 65.6 ). The tendon sheath is entered at the A3 pulley, and the FDS tendon is identified ( Fig. 65.7 ).
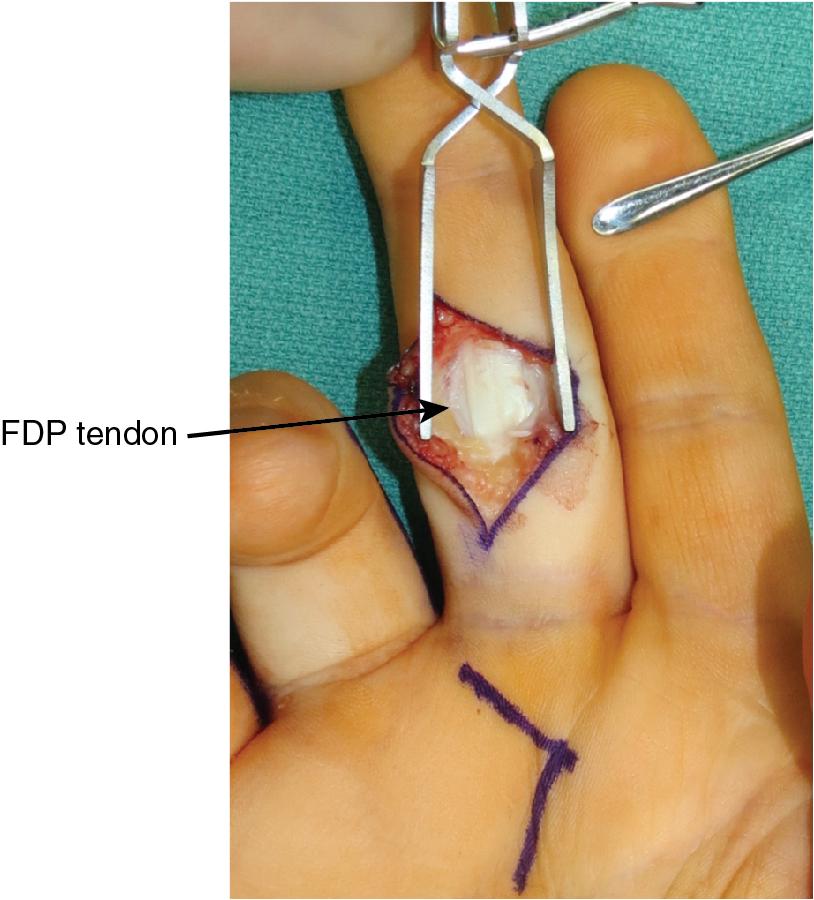
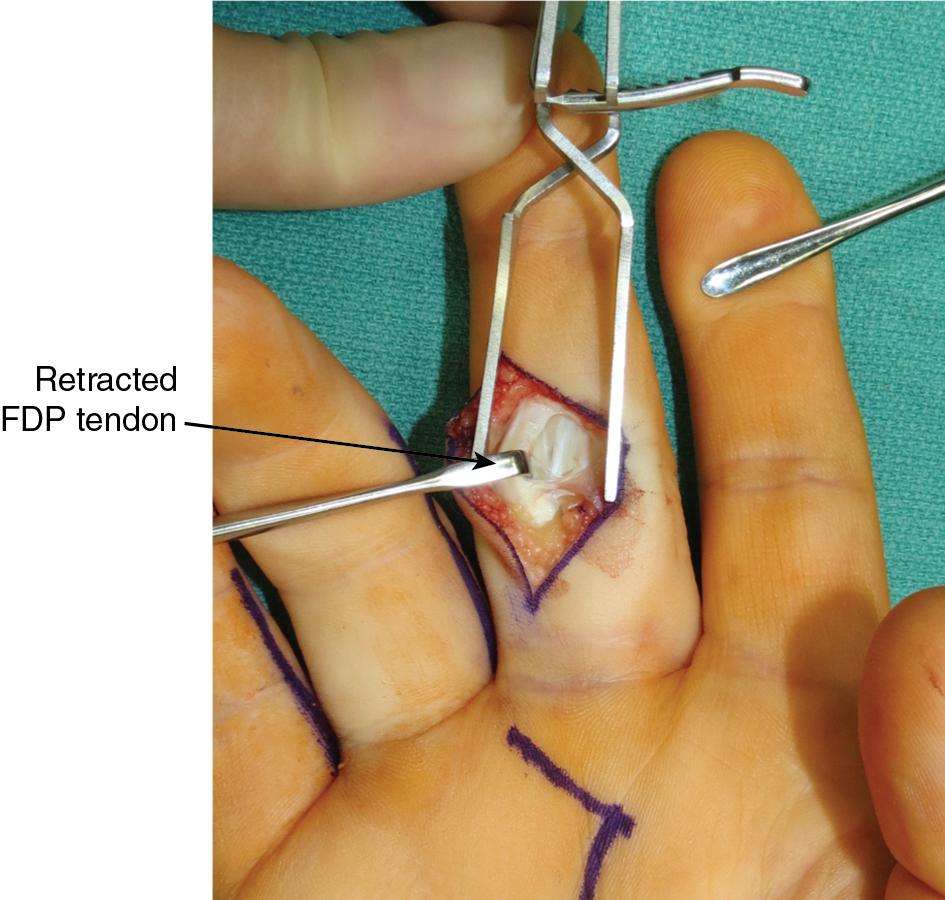
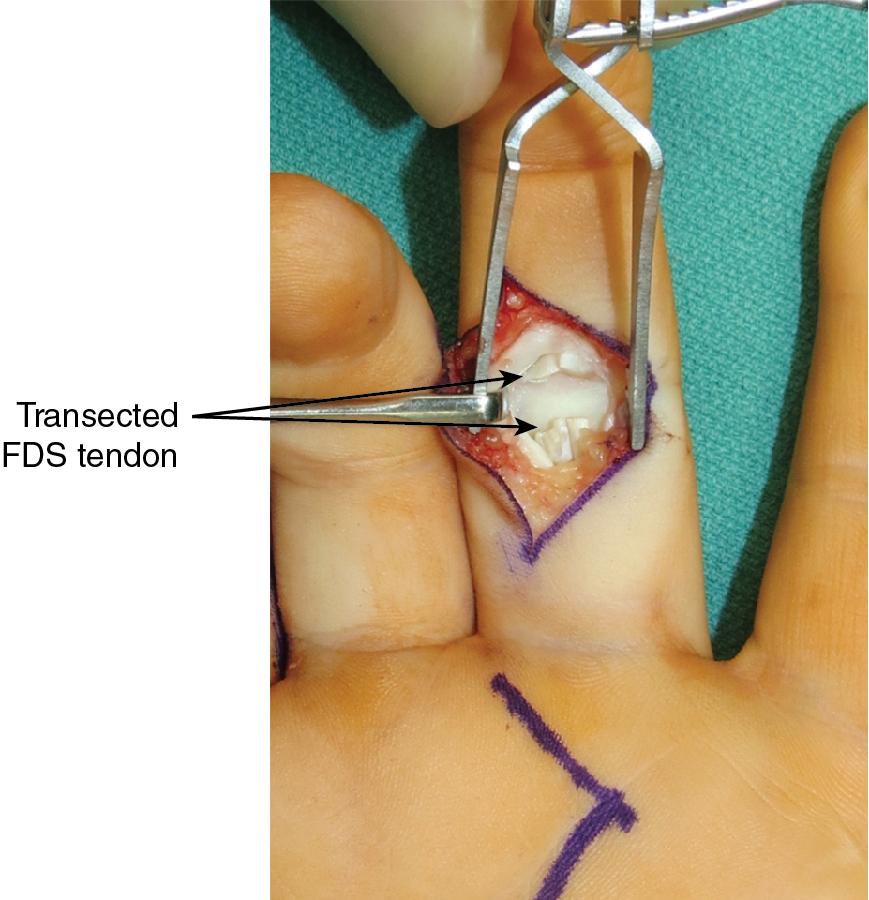
The FDS tendon of the middle finger is located at the level of the decussation under the FDP tendon and transected as distally as possible from its insertion on the middle phalanx ( Fig. 65.8 ).
The harvested FDS tendon is brought out of the palmar incision ( Fig. 65.9 ).
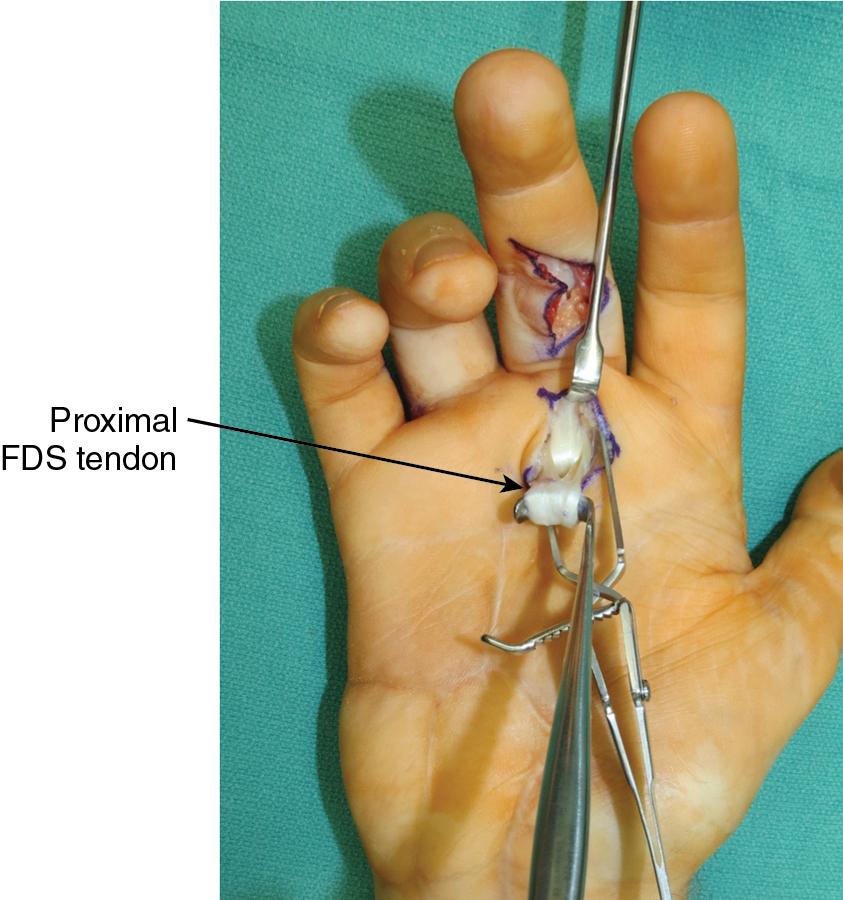
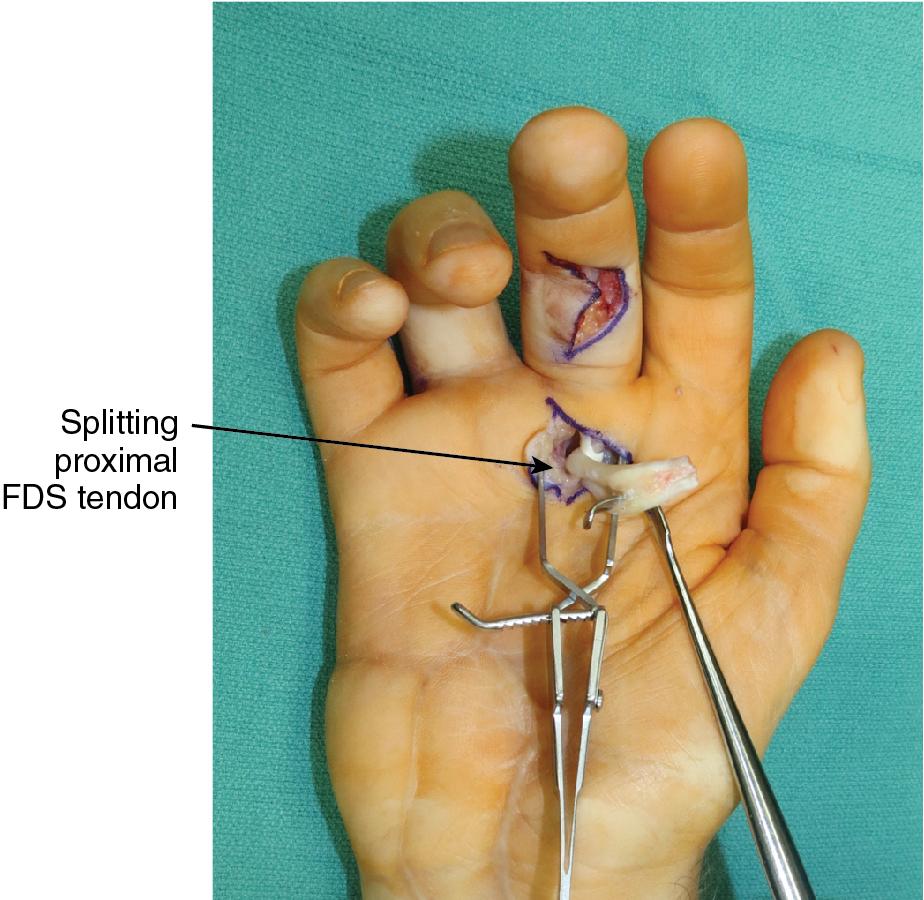
The two slips of FDS are then separated proximally starting at the chiasm to provide two separate donor tendons for transfer ( Fig. 65.10 ).
Using the FDS to correct clawing obviates the need for tendon grafts, which are typically required if wrist extensors are used as tendon donors.
To correct claw deformity of four fingers, the FDS tendon of the ring finger can also be harvested for transfer, in which the long finger FDS is transferred to the index and long fingers, and the ring finger FDS is transferred to the ring and little fingers. Alternatively, the FDS of the long finger can be used as the sole motor, augmented with tendon grafts that provide more tendon substance to power all four fingers.
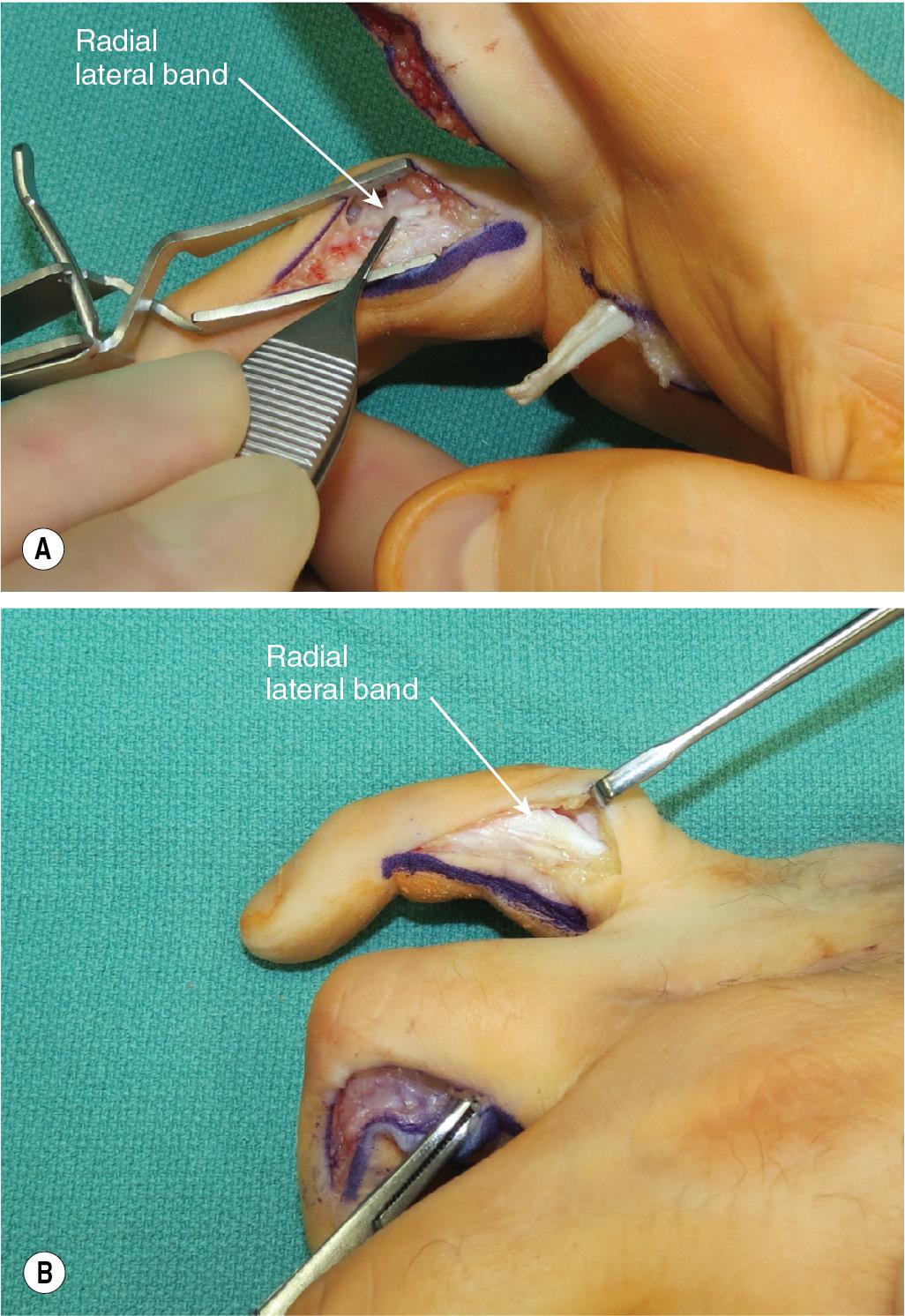
Midaxial incisions along the radial aspect of the ring and small finger at the level of the PIP joint are made and blunt dissection is used through the subcutaneous tissue to identify the radial lateral band. Care is taken not to dissect volarly and risk injury to the neurovascular bundle ( Fig. 65.11A–B ).
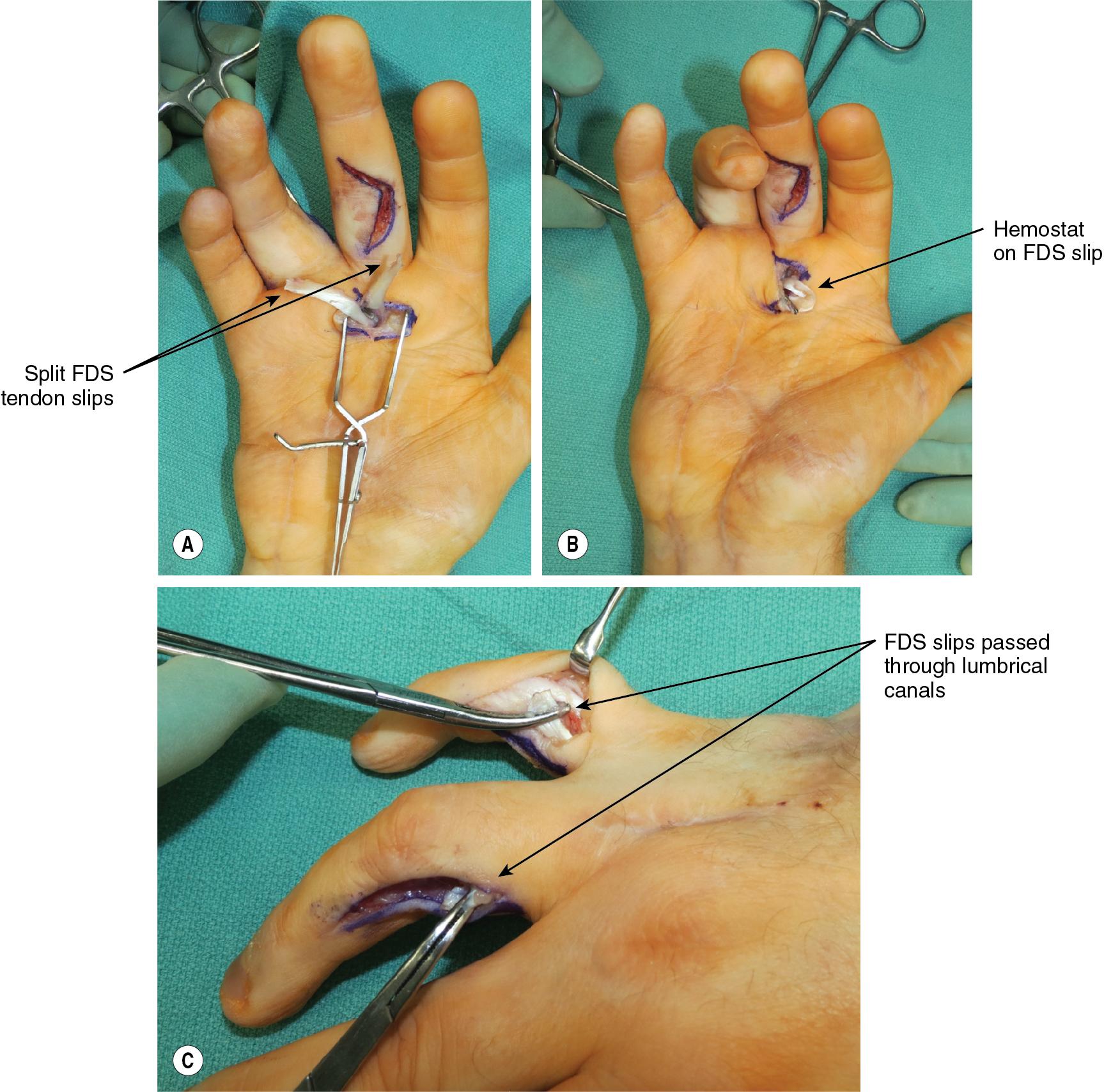
A small hemostat is used from distal to proximal to create a subcutaneous tunnel, and the donor FDS tendon slips are tunneled volar to the deep transverse metacarpal ligament through the lumbrical canal to reach the small and ring finger midaxial incisions ( Fig. 65.12A–C ).
Using a sharp Pulvertaft tendon weaver, the FDS tendon is woven to the lateral band and secured using 4-0 Ethibond suture with sufficient tension to flex the MCP joint and extend the IP joints. The tension is set with the wrist in neutral and the MCP joints in 70 degrees of flexion. Care must be taken not to capture the joint capsule, lateral collateral ligaments, or the central slip with these sutures to prevent adhesions and subsequent loss of motion ( Fig. 65.13A–B ).

The wrist is then passively flexed and extended to assess the tension of the transfer. With wrist flexion, the MCP joints should be extended, given the laxity of the FDS donor tendons. With wrist extension, the tension over the tendon should flex the MCP joints and extend the PIP joints. In practice, one should suture the tendons to the lateral bands in maximum tension because the tension is invariably not strong enough to achieve an intrinsic plus posture.
If the wide-awake, local anesthetic, no tourniquet (WALANT) technique is used, the patient is asked to flex and extend their fingers and ensure adequate tension of the transfer. This can be done after the first suture has been placed in the Pulvertaft weave and any needed adjustment should be made before securing the entire transfer.
The hand is placed in an intrinsic plus volar resting splint and is maintained in immobilization for 4 weeks. After 4 weeks, active and passive ROM exercises are initiated.
A longitudinal incision along the ulnar border of the thumb within the first webspace is used to expose the adductor tendon insertion to the proximal phalanx.
A longitudinal incision over the dorsal wrist is made to expose the ECRB, which inserts on the base of the long finger metacarpal.
A dorsal zigzag incision is made between the head of the long and ring finger metacarpals within the third intermetacarpal space by which the tendon graft is routed to the thumb.
A series of transverse volar incisions in the midline of the forearm are used to harvest the palmaris longus (PL). Alternatively, a short, longitudinal incision is created posterior to the lateral malleolus to harvest the plantaris tendon if the PL is not available. It is quite possible that the ECRB tendon is split in its midline as proximally as possible to flip over to its end to augment its reach. The distal juncture is prevented from splitting by multiple sutures.
The dorsal wrist incision is created, and blunt dissection is carried down through the subcutaneous tissues. The extensor pollicis longus (EPL) tendon is identified, protected, and retracted radially to expose the second extensor compartment. The ECRB tendon lies ulnar to the ECRL and inserts on the base of the long finger metacarpal. The ECRB is divided as distally as possible. It is withdrawn through the extensor retinaculum proximally.
An incision is made along the ulnar border to the thumb to identify the adductor tendon at its insertion on the proximal phalanx. Care is taken to protect the neurovascular bundle, which lies volar to the adductor insertion.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here