Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Tendon transfers are indicated for patients with radial nerve injury who have failed to regain sufficient motor function. Critical deficits for patients with radial nerve injury include wrist extension, finger extension, and a combination of thumb extension and abduction.
High radial nerve palsy is defined as an injury above the elbow; in a low radial nerve palsy (below the elbow), innervation to the upper arm muscles (triceps, brachioradialis [BR], and extensor carpi radialis longus [ECRL]) remains intact.
Common tendon transfers for radial nerve palsy include pronator teres (PT) to extensor carpi radialis brevis (ECRB) to restore wrist extension, flexor carpi radialis (FCR) to extensor digitorum communis (EDC) to restore finger extension, and palmaris longus (PL) to extensor pollicis longus (EPL) to restore thumb extension. If the PL is not present, the flexor digitorum superficialis (FDS) tendon of the long finger is used to restore thumb and index finger extension. We do not take the ring finger FDS tendon to preserve the power grip that is a critical function. The FDS tendon from the long finger is strong enough to power the thumb and index finger simultaneously for coordinated extension of these two digits during pinch.
Restoring wrist extension helps stabilize the hand during finger flexion, which permits a powerful grip. Stabilizing the wrist should be done first in the sequence of tendon transfer procedures. Once the wrist transfer tension is set, then the finger tendon can be modulated based on the tenodesis effect of a normal wrist arc.
Although there are several wrist extensor tendons, the first choice as a recipient for wrist extension is the ECRB. Because it inserts along the long finger metacarpal, it provides effective wrist extension without ulnar or radial deviation.
Early end-to-side transfer of the PT to ECRB for high radial nerve palsy patients can be considered at the time of initial nerve repair to act as an internal splint and facilitate activities of daily living while nerve recovery is anticipated.
In a low radial nerve (or posterior interosseous nerve [PIN]) palsy, active wrist extension is maintained. In these patients, only transfers to restore finger and thumb extension are indicated.
Persistent joint contracture is a contraindication to tendon transfers. Patients must have full passive mobility of their wrist, fingers, and thumb before surgery for transfers to be successful.
The extremity must be free of edema and the planned tendon routes should be without significant skin and subcutaneous scarring. If the path of the transfer is scarred or is covered by skin grafts, one must excise these unyielding tissues and cover them with a pliable skin flap.
Tendon transfer should not be undertaken if there is preoperative weakness of donor motor muscles. Donor muscles must be British Medical Research Council (BMRC) grade 4 or 5 before surgery because loss of one strength grade is typical after transfer.
Progressive neurologic disease may preclude tendon transfer because the patient may continue to lose additional muscle function.
Patients who may be uncooperative with the postoperative immobilization and rehabilitation should not undergo surgery.
Examination of the wrist and digits should demonstrate passive range of motion (ROM) and ensure that no contractures are present.
The muscles affected in patients with high radial nerve palsy include the triceps, BR, ECRL, ECRB, supinator, extensor carpi ulnaris (ECU), extensor digiti minimi (EDM), abductor pollicis longus (APL), EPL, extensor pollicis brevis (EPB), and extensor indicis proprius (EIP). Each should be tested independently to determine the level of injury and reconstructive needs.
The presence of the PL tendon can be confirmed by having the patient touch the thumb and little finger with the wrist in flexion. The PL tendon is usually palpable on the palmar aspect of the wrist, on the ulnar side of the FCR tendon.
The pathway and branches of the radial nerve are noted in Chapter 59 .
Patients with low radial nerve palsy present with preserved wrist extension because of the proximal innervation of the ECRL. Low injuries proximal to the PIN will result in wrist extension with radial deviation stemming from unbalanced action of the intact ECRL because the innervations to the ECRB and ECU are lost. Injuries distal to the PIN will have preservation of ECRB and ECU innervation and thus will present with balanced wrist extension.
Tendon transfers are performed with the patient placed in a supine position with an upper arm tourniquet and a regional block, or under general anesthesia.
Surgeons comfortable with the WALANT (wide awake, local anesthesia, no tourniquet) technique may choose to perform the surgery using local anesthesia; a large volume of local anesthetic may be needed to adequately infiltrate every planned incision.
The upper extremity is outstretched on a hand table.
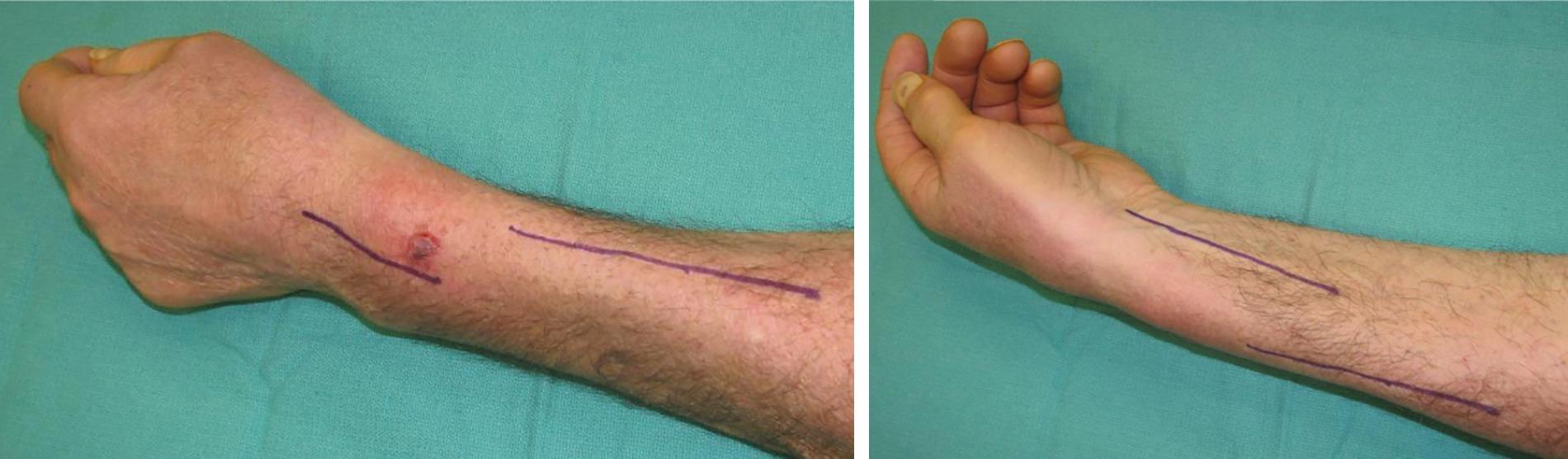
Three separate incisions are used: (1) on the radial forearm, (2) on the volar forearm, and (3) over the proximal dorsal wrist. A 6-cm incision along the radial aspect of the midforearm provides access to the insertion of the PT, as well as the BR, ECRL, and ECRB ( Fig. 66.1A–B ). A 4-cm longitudinal incision is made over the dorsal wrist just ulnar to the Lister tubercle to expose the third and fourth extensor compartments. A 6-cm longitudinal incision is made over the volar aspect of the distal forearm beginning at the proximal wrist to expose the FCR, PL, and FDS to the long finger. A 2-cm longitudinal incision is made over the dorsal aspect of the thumb metacarpophalangeal (MCP) joint.
The EPL tendon can be exposed and delivered through a small incision on the dorsal thumb by identifying the Lister tubercle.
Exposure and harvest for all planned transfers may be performed before the first transfer is completed. The most robust transfer (PT to ECRL) should be tensioned and secured first before moving on to more delicate transfers (e.g., PL to EPL).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here