Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
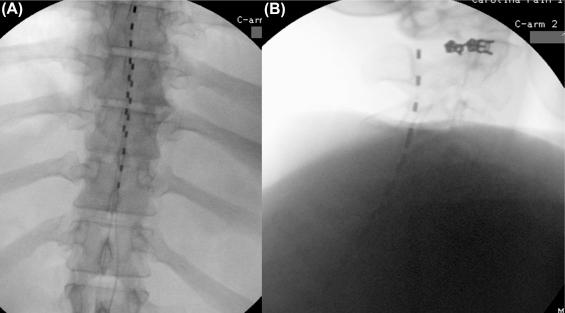
One of the major technological advancements over recent years in spinal cord stimulation (SCS) therapy comes from the introduction of a novel 10 kHz high-frequency (HF) waveform to treat severe chronic pain with seemingly greater effectiveness than traditional paresthesia-producing SCS, providing broader applicability of this treatment. While traditional low-frequency SCS has been proven as a safe, effective, and cost-effective treatment, wider acceptance of this therapy is still modest, mainly because of only moderate long-term improvements in pain scores and the presence of frequently unpleasant and unwanted paresthesias. Indeed, 49%–71% of patients find paresthesias produced during traditional SCS unpleasant, caused either by a significant increase in the stimulation intensity or sudden surges and shocks that would become less tolerable over time ( ). Moreover, 10 kHz HF SCS therapy may provide a rescue treatment for patients who have previously failed surgical and less invasive therapies, including traditional SCS ( ). Pain control is achieved with 10 kHz SCS by anatomic placement of leads ( Fig. 54.1 ) without the need to induce paresthesias, negating the requirement for paresthesia mapping of the patient’s painful areas for pain relief, as is necessary with traditional SCS.
Current indications for 10 kHz SCS, supported by clinical evidence, include chronic low back pain (CLBP) and chronic leg pain. Preliminary data has emerged on a similar degree of pain relief that is seen with CLBP and chronic leg pain and an improvement in function when 10 kHz SCS is trialed for chronic upper-extremity and neck pain as well as peripheral neuropathy ( ).
Basic science and mechanisms of action that pertain to 10 kHz SCS are discussed in Chapter 29 . This chapter focuses on the discussion of data from clinical studies.
The first human short-term feasibility clinical study on 10 kHz SCS was completed in 2008 ( ). This study documented a significant improvement in back and leg pain scores during a 28-day paresthesia-free trial stimulation period, via two temporarily placed octapolar leads. The results showed that 10 kHz SCS provides better control of CLBP and chronic leg pain than traditional low-frequency SCS, with 88% (21/24) of patients preferring the former therapy over the latter ( ).
This initial evidence was followed by much larger clinical studies. A multicenter prospective European study provided, for the first time, evidence for longevity and robustness of 10 kHz SCS in a cohort of patients with CLBP and chronic leg pain ( ). In an uncontrolled multicenter cohort study on 83 subjects with severe CLBP and chronic leg pain, 10 kHz SCS provided greater than 50% pain relief at 6 months in nearly three-fourths of the patients, along with significant improvements in disability and sleep and reduced medication use ( ). The same group of researchers reported 2-year data from the same study demonstrating sustained relief of CLBP and chronic leg pain, functional and sleep improvements, and opioid use reduction ( ). Very few therapy-related side-effects were reported, and those few were in line with already reported complications of traditional SCS ( ).
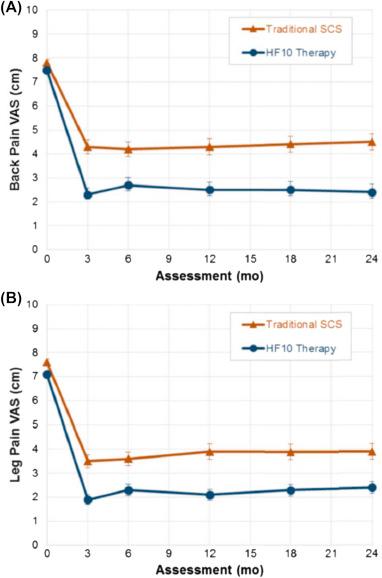
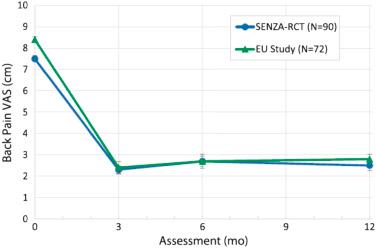
Therapeutic success of 10 kHz SCS in this uncontrolled single-cohort study in Europe was followed by a multicenter prospective randomized controlled trial (RCT) in the United States. The study (SENZA-RCT) was designed with United States Food and Drug Administration (FDA) input, and led to FDA approval of this therapy in May 2015. This RCT evaluated efficacy of 10 kHz SCS as compared to traditional low-frequency SCS in subjects with severe (≥5 cm in visual analog scale) CLBP and chronic leg pain ( ). A total of 198 subjects were randomized in 10 different clinical research centers in a 1:1 ratio to two treatment groups, consisting of traditional SCS (Precision Plus System, Boston Scientific) and 10 kHz SCS (Nevro Corp.); of the 189 subjects who underwent and passed a temporary trial with significant pain relief (≥40% pain relief), 171 were implanted with one or the other SCS system. The primary outcome of this study was the proportion of responding subjects at 3 months follow-up with ≥50% of CLBP reduction and absence of stimulation-related adverse events (AEs) (Kapural et al.). In the 10 kHz SCS group 84.5% and 83.1% were back pain and leg pain responders, respectively. In the traditional SCS group 43.8% of the subjects were back pain responders and 55.5% were leg pain responders ( P < .001). Sustained superior responses of 10 kHz SCS were observed through 12 and 24 months ( P < .001) ( ). At 24 months 76.5% of patients had more than 50% of CLBP relief using 10 kHz SCS versus 49.3% of the responders using traditional SCS. Similarly, 72.9% of patients in the 10 kHz SCS treatment group had more than 50% leg pain relief versus 49.3% in the traditional SCS group ( P < .001 for noninferiority and P = .003 for superiority) ( ) ( Figs. 54.2 and 54.3 ). The most commonly reported study-related AEs were uncomfortable paresthesias in the traditional SCS patient group (11.3%), as compared to none in the 10 kHz SCS treatment group. Nearly half the study subjects (46.5%) in the traditional SCS group claimed their paresthesias were unpleasant ( ).
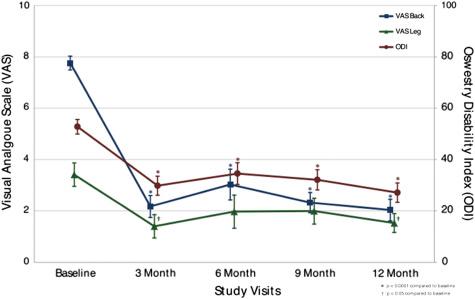
This sustained long-term data from two clinical studies on intractable CLBP using 10 kHz SCS has prompted the idea that the therapy could be beneficial for a group of patients who had no prior back surgery, as well. In SENZA-RCT, 13% of the 10 kHz SCS subjects had no prior back surgery and had an 83.3% back pain responder rate at 24 months ( ). Recently, data from a single-center case series in a cohort of 21 surgically naıve patients suffering from chronic medically refractory, predominantly axial CLBP unsuitable for surgical intervention has been reported ( ). The 10 kHz SCS therapy significantly reduced pain intensity by 73%, the Oswestry Disability Index (ODI) showed a 48% reduction, and opioid medication usage was reduced by 64% at 12 months postimplant when compared to baseline. Consequently, health-related quality of life (EQ-5D) scores improved from 0.16 to 0.47 and four out of eight unemployed patients were able to return to work. This data supports the hypothesis that 10 kHz SCS could be beneficial for a group of patients with CLBP who have not undergone surgery for the problem, and may prompt further comparison studies ( ; Fig. 54.4 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here