Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Syringomyelia, or cavitation within the substance of the spinal cord without an ependymal lining, has been recognized for more than 300 years as a pathologic entity. Etienne is credited for the first pathologic description in 1564 in La Dissection du Corps Humain ; he described a cystic lesion in the spinal cord that contained a “fluid, reddish, like the fluidity of that of the ventricles.”
Portal, in 1804, first appreciated and connected the clinical syndrome of an intramedullary cyst with the pathologic changes of the spinal cord. Ollivier then coined the term “syringomyelia,” combining the Greek words for “tube or pipe” and “marrow.” He documented a connection between the fourth ventricle and this cystic structure, which he believed to be a congenital anomaly.
The classic clinical description of syringomyelia is described as a dissociated, suspended segmental sensory loss, consisting of loss of sensation to pain and temperature and preservation of sensation to proprioception and light touch. Slowly progressive distal motor dysfunction may also occur. A syrinx may extend to the medulla and cause lower brain stem and cranial nerve dysfunction, termed syringobulbia.
Those ependymal-lined cavities that appeared to be pathologic dilatations of the central canal were termed hydromyelia. Some authors viewed hydromyelia, in which the central canal was dilated but preserved, and syringomyelia, with or without a connection to the central canal, as stages of a common process. Unification of the terms resulted in the concept of syringohydromyelia or hydrosyringomyelia.
In 1973, Barnett published the first English-language monograph on syringomyelia. He proposed a classification based on a variety of clinical and experimental observations and studies. The classification scheme consisted of two broad categories: (1) communicating syringomyelia (e.g., Chiari I malformation, Chiari II malformation, basilar arachnoiditis) and (2) noncommunicating syringomyelia (e.g., occurring with spinal dysraphism, spinal cord trauma, spinal cord tumor, spinal arachnoiditis; Box 94.1 ).
Over the last 20 years, experimental and clinical work, including that of Oldfield and Milhorat and their colleagues, has helped to clarify the pathophysiology and treatment of this complex syndrome. Nevertheless, a definite understanding of the etiology of syringomyelia has yet to be clarified.
Although the pathophysiology of syringomyelia has not yet been completely defined, the association between syringomyelia and congenital abnormalities was appreciated long ago. Baulmer was credited initially for establishing this relationship in 1887. Schlesinger further substantiated this association in 1895 by noting congenital abnormality in one-third of the cases of syringomyelia that he had reviewed.
Ollivier d'Angers formulated and Leyden further refined the developmental theory of syringomyelia formation. These authors stated that syringomyelia must be considered a congenital disorder associated with embryonic maldevelopment, specifically, incomplete occlusion of the primitive fold. This improper fusion of the two folds of the primitive medullary groove allowed the abnormal lining of germinal cells to persist, resulting in simple hydromyelia.
Another theory implicates environmental fetal exposure in the pathophysiology of syringomyelia. Kahler and Pick in 1879 theorized that chronic intrauterine inflammation resulted in gliosis and aberrant development of the spinal cord that subsequently led to syrinx formation. On the other hand, in 1910, Haener proposed that events during the act of birth (e.g., trauma) may arouse neural activity in abnormally enclosed tissue, with resultant syrinx formation. None of these claims were formally substantiated in case series.
In a series of landmark papers, W.J. Gardner expounded his hydrodynamic theory of the pathophysiology of syringomyelia. Gardner's theory was the first among three prominent current theories. He based his theory on three observations: (1) dye injected into the ventricular system was recovered from the syrinx at operation, (2) fluid withdrawn from the syrinx at operation strongly resembled cerebrospinal fluid (CSF) found in the ventricular system, and (3) experimental hydrocephalus produced by obstruction of the normal outflow of CSF from the fourth ventricle resulted in the formation of syringomyelia that was in communication with the ventricular system.
Syringomyelia could be explained by failure of the embryonic rhombic roof to fenestrate during a critical period of development. The inability of CSF in the fourth ventricle to gain the usual access to the subarachnoid space during the 6th to 8th weeks of embryogenesis forced the hindbrain to herniate through the foramen magnum. A Chiari malformation was thereby created, and the failure of the CSF to expand the subarachnoid space resulted in communicating hydrocephalus. Gardner believed that the effect of the hindbrain malformation was to increase the obstruction to outflow at the foramen of Magendie and deflect the pulse wave of CSF into the opening of the central canal at the obex.
The pulse wave effect of the diverted CSF acted as a water hammer, gradually dilating the central canal or dissecting the substance of the spinal cord around the canal and creating a syrinx. From the perspective of Gardner, a congenital hindbrain defect that obstructed the CSF flow from the fourth ventricle to the subarachnoid space was the sine qua non of syringomyelia. Ball and Dayan and West and Williams questioned Gardner's theory and the necessity of a direct communication to the fourth ventricle for production of a syrinx. To support this statement, Milhorat and colleagues demonstrated in large autopsy studies that the majority of syrinxes did not communicate with the fourth ventricle and that the central canal was not patent in most normal adult patients.
Williams proposed an alternative theory to explain syrinx formation and speculated that a partial block of the spinal subarachnoid space produced a pressure differential between the ventricular system and the spinal subdural space during Valsalva-type maneuvers. He explained that venous distention associated with these maneuvers produced an increased intracranial pressure that was not evenly distributed to the lumbar subarachnoid space because of a more proximal subarachnoid block. This pressure difference was labeled craniospinal pressure dissociation , and the lower pressure in the lumbar theca caused fluid to be drawn into the syrinx. This phenomenon was termed suck .
Williams also believed that the cavity enlarged after its initial formation as the result of compression of the lower end of the cavity with the rapid filling of the epidural venous plexus during a cough or sneeze. The fluid in the syrinx was then propelled rostrally, dissecting the central canal or pericentral parenchyma of the spinal cord. Williams applied the term slosh to this part of his theory to explain syrinx extension.
Oldfield and colleagues used magnetic resonance imaging (MRI) with and without cardiac gating, intraoperative ultrasonography, and direct intraoperative observation of the exposed hindbrain and documented the downward movement of the cerebellar tonsils during systole. This group interpreted the data as obviating the necessity of a direct communication with the fourth ventricle, as advocated by Gardner. Moreover, they observed that the syringomyelic cord did not enlarge with Valsalva maneuver and that venous pressure had little to do with syrinx elongation, disputing the Williams suck and slosh theory. These authors proposed that the abnormal pulse wave in the spinal subarachnoid space, caused by the partial obstruction by the hindbrain, placed pressure on the spinal cord and dissected the central canal, causing the cyst to enlarge.
The ingress of CSF within the spinal cord parenchyma has recently been suggested to enter through dilated Virchow-Robin spaces. The blockage of flow creates eddylike currents analogous to a boulder in a rapidly flowing river. These forceful currents enter the cord parenchyma and first create microscopic changes (i.e., myelomalacia). They later develop into more confluent macrocystic cavities by dilation of the central canal and/or peripheral areas of the spinal cord.
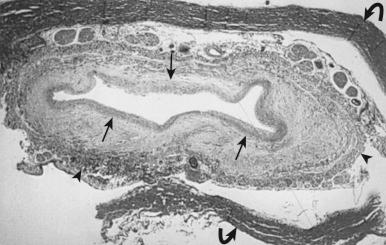
Milhorat and colleagues proposed that normal CSF flow was from the spinal subarachnoid space through the parenchyma of the spinal cord into the central canal. The CSF then flowed into the fourth ventricle outlet at the obex. Their theory was supported with a rodent model of syringomyelia. They injected kaolin into the central canal of rats, causing stenosis of the proximal central canal through an inflammatory reaction. A resultant syrinx was formed. These authors suggested that syrinx formation was due to disruption of normal CSF flow by the inflammatory stenosis ( Fig. 94.1 ).
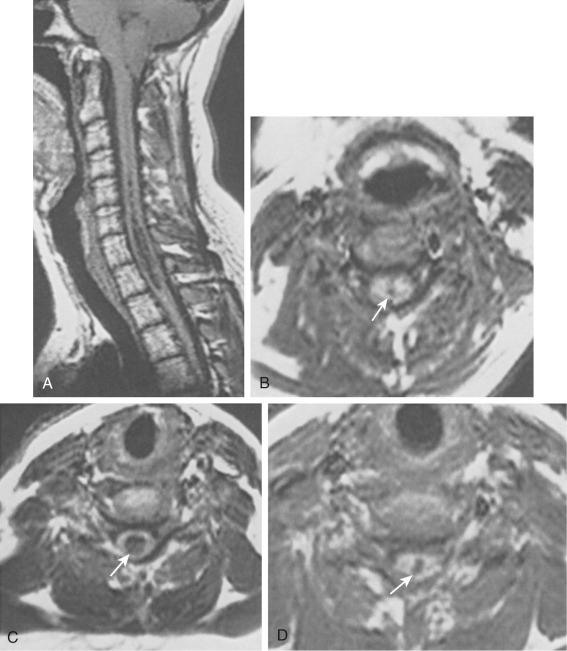
In 1896, Chiari published an addendum to an earlier work in which he described anomalies associated with hydrocephalus. In this latter publication, there were descriptions of patients with hydromyelia. Gardner and Goodall found that a majority of patients undergoing surgical decompression for symptomatic Chiari I malformation had a concurrent syringomyelia ( Fig. 94.2 ). Gardner and colleagues demonstrated, at operation, communication between the syrinx of the upper cervical cord and the ventricles in patients undergoing suboccipital craniectomy and cervical laminectomy for decompression. Indigo-carmine was injected into the patient's lateral ventricle, and colored CSF was recovered by direct puncture of the cervical syrinx.
Appleby and colleagues established that a “communicating” type of syringomyelia could also be acquired from chronic arachnoiditis involving the basal cisterns and obstructing the outflow of CSF from the fourth ventricle.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here