Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Midshaft clavicle fractures which require reduction and internal fixation can be managed using two primary approaches. Open reduction and internal fixation with one or more plates is one approach and intramedullary (IM) fixation is another option. IM fixation may be performed percutaneously or through a limited open approach. This chapter reviews the indications, techniques and potential complications of IM and percutaneous fixation of midshaft clavicle fractures.
Keywords: Clavicle Fracture, Intramedullary Fixation, Midshaft Clavicle, Percutaneous Pinning
This chapter is adapted from Basamania CJ, Rockwood CA Jr. Fractures of the clavicle. In: Rockwood CA Jr, Matsen FA, Wirth MA, Lippitt SB, Fehringer EV, Sperling JW, eds. Rockwood and Matsen’s The Shoulder . 5th ed. Philadelphia: Elsevier; 2017.
Intramedullary (IM) pinning of clavicle fractures is a long-practiced technique with reported advantages over plate fixation, including reduced periosteal stripping, smaller skin incision, less risk to supraclavicular nerves, less bleeding, shorter surgical times, and healing via endochondral ossification (callus), which can be more easily assessed radiographically than direct bone healing (intramembranous ossification). A recent meta-analysis reported that IM fixation of midshaft clavicle fractures could achieve similar union rates and shoulder scores with superior surgical outcomes including significantly less time to union than plate fixation ( ). These findings remained constant when conducting subanalyses in only randomized controlled trials (RCTs). Significantly less blood loss, shorter operative time, smaller surgical wounds, and fewer complications in the IM group were also reported ( ).
Many surgeons may be reluctant to use IM clavicle fixation given past reports of major complications and perceived risk of pin migration. Randomized studies and a recent meta-analysis have reported both similar complication rates, as well as significantly lower overall and major complications with IM pinning versus plate fixation ( ). Nevertheless, there are numerous reports of IM device migration in clavicle fixation ( ). Skin and soft tissue irritation resulting from migration, telescoping, or hardware protrusion represents one of the chief complications with IM fixation ( ). The dilemma of IM fixation, unlike plate fixation, is that nail removal is often intended after the fracture has healed. The challenge with this is that the device needs to have a low profile so it does not cause irritation, but it must be prominent enough to be easily retrieved. Unlike plate and screw constructs, IM fixation can be removed under light sedation and local anesthesia. With current techniques and implants, IM devices are reported to have a low rate of unplanned revision surgery and to be a safe and effective form of fixation ( ).
Construct rigidity is a concern particularly when treating contact athletes who are at risk for refracture. In the setting of comminution, the cantilever effect for a pin extends to the medial-most portion of the pin, thereby providing fixation in bending loads. It also allows axial compression, which should enhance healing. However, reported superior biomechanics to bending and torsional forces with plate versus IM fixation in a cadaveric midshaft clavicle fracture model ( ). In contrast, reported that failure torques of IM repair and plate repair were not significantly different; however, failure torque after IM device removal was significantly greater than after plate removal ( ). Nevertheless, IM pinning is a viable fixation option in athletes, particularly considering recent data that suggest shorter time to union and lower rate of complications.
The management of midshaft clavicle fractures should be individualized to the patient’s goals and activity level. The primary surgical indications for open reduction internal fixation of midshaft clavicle fractures include shortening greater than 2 cm, 100% or greater fracture displacement, and fracture comminution ( ). In athletes, prolonged recovery and deficit in shoulder strength are often poorly tolerated, making surgery the typically preferred treatment. For most midshaft fractures that do not have excessive comminution or obliquity to the fracture planes, IM fixation is an excellent option to minimize fragment stripping, avoid supraclavicular nerves, achieve relative stability, and improve cosmesis. Complex, comminuted fractures, however, are not appropriate for IM nailing, with reported difficulties achieving and securing accurate reduction ( ). In such cases, surgeons should consider plate fixation. The primary IM options include smooth, threaded, and partially threaded devices. These can be rigid or flexible and, in the case of hybrid fixation, can have flexible and rigid components. Despite having less risk of migration than smooth devices, fully threaded devices are seldom used because of the risk of gapping at the fracture site, which can impede healing ( ). There are numerous reports of migration of smooth devices used in clavicle fixation ( ). If these devices are used, they need to be followed closely for any radiographic signs of migration. Although smooth pin fixation has declined in popularity, the use of smooth titanium elastic nails (TENs) gained popularity in the 2000s in treating clavicle fractures ( ). One of the primary advantages in using a flexible nail is that it allows considerable length of fixation as compared with a rigid device. Despite this, there remains the risk of implant migration, and some studies show a rate of loosening or migration of 4% to 25% ( ). The addition of a hybrid fixation has alleviated many of the problems associated with IM pinning with improved length and rotational control over other IM devices and the ability to place an interlocking screw for increased rigidity and rotational control ( ).
Two important determinants of IM fixation are the diameter of the IM canal and the length of fixation. The IM canal determines the maximum size of the device. For the pin to travel the most effective length, it makes three-point contact with the walls of the canal: anterolaterally, then posteriorly at the apex of the posterior curve, and then again anteromedially when it contacts the anteromedial curve. An important relationship exists with a larger diameter IM fixation, whether it is a screw, pin, or smooth wire; namely, it will be stiffer but potentially allow less fixation length. There will also be greater stresses with short fixation, which could lead to increased risk of loosening, failure of the fixation, and healing. Significantly increased length of fixation with significantly more fixation in the lateral fragment has been reported using a 3.2-mm pin compared with a 4.0-mm pin ( ). Another consideration in the diameter of pin fixation is that pin stiffness is directly proportional to the fourth power of the pin radius (I = πr 4 /4). In other words, as the pin becomes larger, its stiffness increases considerably. Some micromotion is preferred to enhance endochondral bone formation. If the pin is too large, it will be excessively stiff, which may inhibit bone healing. Therefore the surgeon should pick the smallest pin that has stable fixation within the bone. In our experience, most midshaft clavicle fractures in female patients can be stabilized with a 2.5-mm pin, and most male patients receive a 3-mm pin. Seldom do we use a larger pin except in very large patients or in older patients who have age-related increases in their canal diameters. Because the clavicle has very little soft tissue coverage, any type of IM fixation that protrudes from the bone can cause soft tissue problems. It is imperative that the portion of any IM device outside of the bone have the lowest profile possible.
Another point to consider with IM pinning is that these devices frequently cannot be statically locked, thereby providing less rotational and length stability compared with other fixation techniques ( ). However, there are implants now on the market that have an interlocking screw feature. Achieving good IM fit, typically achievable with a 3.0-mm pin, is desirable.
The advantage of this technique is restoring length, alignment, and rotation with minimal soft tissue stripping, minimal blood loss, and small incisions. The IM device allows compression at the fracture site and load sharing, which are advantageous in the healing of other long-bone fractures. All cases are performed in an outpatient setting under general anesthesia with local anesthesia supplementation.
The procedure can be performed in a supine or modified beach-chair position on a radiolucent operating table. We prefer the modified beach-chair position for easier access to the posterior aspect of the shoulder. The torso of the patient is typically at about 45 degrees relative to the floor. A bump is placed under the ipsilateral scapula to help extend the arm and reduce scapula protraction. A large C-arm greatly facilitates pin placement. The C-arm base is brought in from the injured side ( Fig. 14A.1 ). Standard prep and draping is performed, being mindful to include the entire shoulder girdle in the operative field all the way to the sternum. The arm should also be draped free, allowing movement of the arm to facilitate drilling of the lateral fragment and reduction of the fracture.
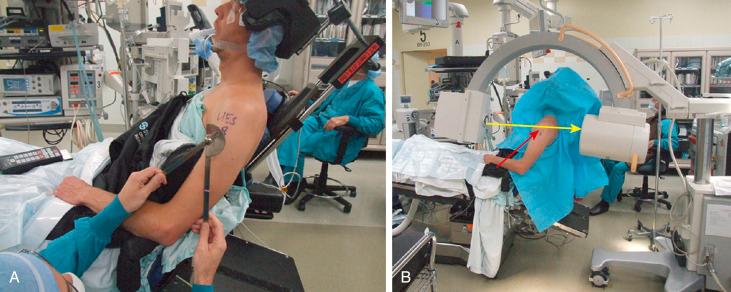
The patient’s torso should be approximately 45 degrees relative to the floor. The gantry of the C-arm should be situated such that the beam of the x-ray is parallel to the floor (see Fig. 14A.1 ). This gives the equivalent of a 45-degree cephalic tilt view of the medial clavicle, which allows the best view of the anterior curve of the clavicle. This orientation also gives a cephalic tilt view of the lateral fragment because placement of a retrograde IM fixation in the lateral fragment is crucial to obtaining anatomic reduction of the fracture. Furthermore, an “anteroposterior (AP) equivalent” view ( Fig. 14A.2, A ) can be obtained by extending the arm, and an “axillary equivalent” view can be obtained by forward flexing the arm ( Fig. 14A.2, B ). It should be noted that plain AP radiographs typically underestimate the length of the fracture because the clavicle is oblique to the x-ray beam.
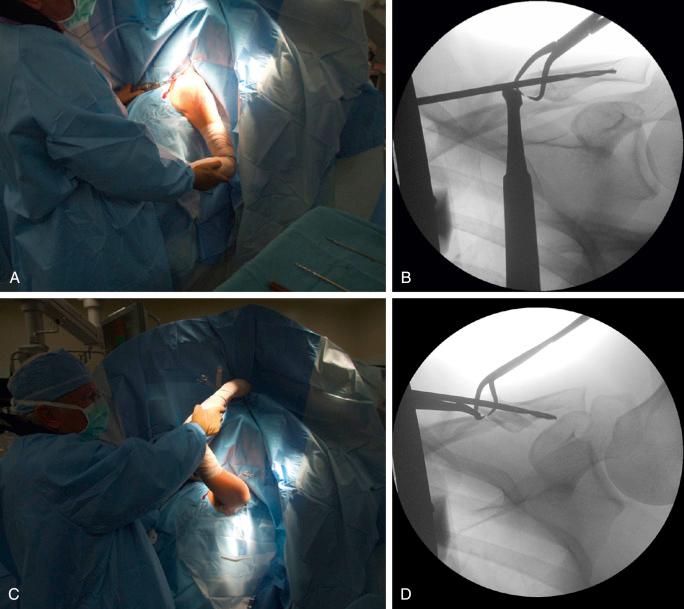
Because of metallic or radiopaque devices on the operative table, the beam of the C-arm may need to be oriented in a posterolateral to anteromedial orientation. In this situation, there may be significant underestimation of the length of the fracture or overlap of the fragments because the clavicle is obliquely oriented relative to the beam of the x-ray. This underestimation will be exaggerated if the C-arm is oriented in an oblique fashion relative to the torso. If necessary, the patient’s shoulder can be brought forward to obtain a better estimation of the true fracture length. It is also important that the entire length of the clavicle can be viewed in one position. After these points are accomplished, the entire case can be completed with the use of a foot pedal to activate the C-arm, thereby negating the need to have a radiology technician. As mentioned, the patient’s arm is draped free to allow movement during the case for better visualization and fracture reduction.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here