Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Because of their frequency and severity, hand infections are a surgical emergency. Despite being apparently benign, they should not be underestimated; they are the source of significant sequelae if treatment is not adequate and fast. Regular monitoring of the patient is essential to check the evolution towards recovery and to track the development of complications.
The purpose of this chapter is not to discuss antibiotic therapy, which should always be tailored to the local flora and the possibility of resistance development. Our purpose here is to list the different clinical presentations of hand infections and clarify their methods of treatment.
The hand is richly vascularized and becomes infected relatively infrequently considering the number of injuries and wounds it suffers in daily life. Infection usually results from direct inoculation of open wounds and rarely from disseminated causes. Irregardless, the principles of management remain the same.
Septic inoculation causes a host reaction that is characterized by inflammation and an immune response; this is known as the inflammatory phase. This immune response results in the release of enzymes and toxins against the offending pathogen. Edema and swelling, associated with infection, cause an increase in tissue pressure that can result in tissue necrosis; this is the purulent phase. The infection is initially contained within the fibrous capsular structures of the pulp septae and the synovial sheath, which correlates with the clinical presentation of specific types of hand infections. However, the proximity of these structures to each other can result in the rapid spread of infection. We note specific clinical signs in each location.
The bacterial inocula in hand infections are of a low volume, and general systemic symptoms are rare. Lymphangitis and lymphadenopathy may be encountered during the proximal spread of the infection. Fever and an elevation of C-reactive protein are not found in almost three-fourths of hand infections. These signs are associated with severe infection with bacteremia and are not required to be present for a positive diagnosis to be made. The initial evaluation should also include the tetanus immunization status of the patient, with an appropriate prophylaxis being administered based on the patient's immunization history.
We should always consider the velocity of the progress of clinical signs: hand infections are a surgical emergency. They can progress rapidly from the point of contamination to the presentation of infective symptoms and even to systemic involvement. Immediate care should then be administered because progression of infection will result in severe tissue necrosis.
The interaction between the host and the infectious agent will determine the severity and progression of infection. Immunodeficiencies, among them diabetes mellitus, predispose to infections of greater severity. In such patients, inflammatory signs are less marked, and thus infections are most often recognized and treated at a severe stage. Similarly the use of anti-inflammatory drugs, which transiently improve symptoms, can precipitate the massive spread of infection. Their indiscriminate use has been found in most cases of necrotizing fasciitis. Moreover, indiscriminate antibiotic therapy without surgical debridement can result in the development of chronic infection because it suppresses the clinical signs but does not necessarily lead to healing. Smoking massively reduces the blood flow in the hand, which can reduce the delivery of antibiotics as well as predisposes to the development of tissue necrosis. History of intravenous drug use and diabetes mellitus are strong predictors of polymicrobial infections. Finally, certain bacteria are characterized by significant virulence, such as Pasteurella multocida, some streptococci, and methicillin-resistant Staphylococcus aureus (MRSA), which are increasingly common.
The aims of initial surgical treatment are to reduce the bacterial inoculum and debride the necrotic tissue. Debridement should be thorough, ensuring that all unhealthy tissue is excised. This is important because relapses are related to a poorly performed first debridement. The post debridement wound may be tagged loosely over a drain or left to heal by secondary intention. Multiple intraoperative tissue cultures should be obtained, even for mild infections, as this helps to guide antibiotic treatment. Empirical antibiotics may be started after samples are obtained and should be optimised when the infectious agent is identified.
Close monitoring for the first 48 hours is advised in the treatment of hand infections. Wound inspection and palpation should be performed by the surgeon to determine an improvement in initial signs. If infection persists or inflammatory signs decrease slowly, redebridement should be considered. This would allow for further debridement and irrigation of the wound. Thereafter, the wound is best reevaluated after another 48 hours. Particular attention should be paid to cases of delay-treated pyogenic tenosynovitis and septic arthritis, because recurrences are common. The presence of pyogenic membranes decreases the effects of antibiotics in these cases, and sometimes the initial surgical debridement is not sufficiently extensive.
Early mobilization, dynamic splinting and rehabilitation reduces edema, stiffness and contractures and improves the final clinical outcome.
Paronychial infections include those involving the pulp. The pulp consists of fibrofatty tissue divided by vertical septae into multiple compartments. Following the inoculation of bacteria, inflammation and cellulitis lead to vascular congestion and increased pulp pressure that causes tissue necrosis and severe pain to develop. In 2–3 days, a paronychia forms, and surgical debridement is required. The most common infecting organism is S. aureus.
Periungual paronychia ( Fig. 19.1 ) is the most common. It can be a result of microtrauma from activities such as nail biting, penetrating wounds or a manicure. Determining the mechanism of injury is important to prevent an embedded foreign body from being missed. The invasive phase is characterized by minimal erythema, tenderness on palpation of the lateral nail fold and a non-fluctuant swelling. During the mature stage, often 48 hours after the onset of symptoms, the pain becomes significant, pulsatile, permanent and sometimes causes insomnia. Further clinical examination focuses on looking for complications from the spread of infection.
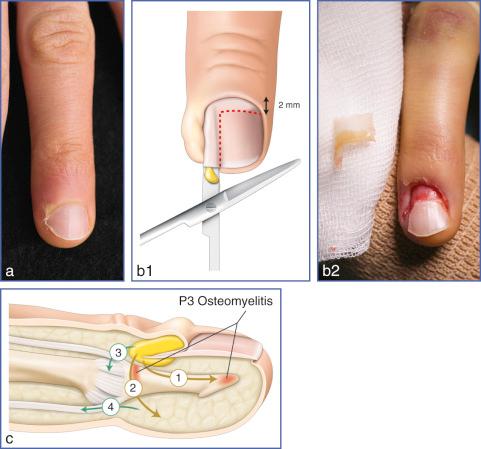
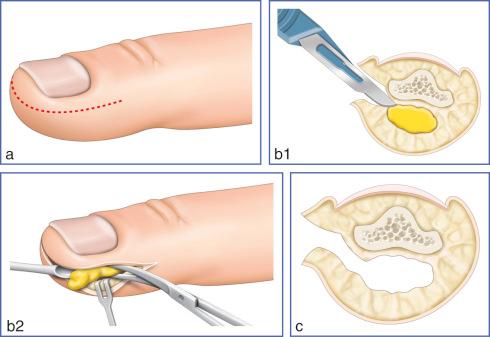
Felon ( Fig. 19.2 ) is less common and characterized by severe throbbing pain, tension and swelling of the entire pulp, whereas the periungual skin is unaffected. Pulp inoculation and the possibility of persistence of a foreign body need to be ruled out. Edema is less marked than compared to the dorsal forms due to the relative stiffness of the pulp septations and the limited space for expansion. A clinical situation resembling compartment syndrome forms, which can lead to rapid fat necrosis. Osteomyelitis of the distal phalanx and flexor tenosynovitis from the proximal extension of the infection can occur.
The differential diagnosis includes herpetic whitlow (ie, due to herpes simplex virus). A 2-week-long positive contact history and the presence of clear, fluid–filled vesicles are characteristic. Resolution is spontaneous after 3 weeks, with a 20% recurrence rate. Incision and drainage of herpetic whitlow is contraindicated so as to prevent bacterial superinfection. Further contact spread is prevented by placing simple dressings over the area.
The complicated presentations arise from neglected infections or partially treated infections with inappropriate use of antibiotics.
It is common to find a lateral or proximal nail bed injury in late-presenting cases of paronychia, reflecting the beginning of a dumbbell-shaped abscess. This form of paronychia occurs when there is lateral and pulp extension by a fistula. It should be routinely explored in all its dimensions during surgical debridement to prevent failure of treatment (see Fig. 19.2c ).
Tendon complications are serious. Volar extension of the infection can lead to development of pyogenic flexor tenosynovitis, and a careful clinical examination should be performed to determine this. If suspected, the sheath should be irrigated. Thereafter, the sheath is closed before debriding the paronychia. Necrosis of the extensor tendon insertion is rare; this can be complicated by septic arthritis of the distal interphalangeal (DIP) joint in an immunocompromised host. Treatment is difficult. The thinness of the extensor tendon makes reconstruction difficult, and arthrodesis is contraindicated in the context of the septic joint. Similarly, immobilization by a dorsal splint is uncomfortable and increases the risk of skin necrosis.
Osteomyelitis and DIP joint septic arthritis can occur in immunocompromised patients, especially in diabetics. Prolonged medical treatment, the use of nonsteroidal anti-inflammatory drugs (NSAIDs) and simple neglect can result in nail bed necrosis and osteomyelitis of the diaphysis of the distal phalanx. Radiologic evaluation is recommended in such a clinical context, and it is important to remember that paronychia can result in the need for a digital amputation. It is difficult to differentiate between proximal extension of the infection to involve the DIP joint and that of a tender paronychia. Therefore, symptoms of pain on lateral joint palpation and with active joint mobilization should be carefully evaluated (see Fig. 19.11a ).
Skin necrosis and fistula formation around the paronychial region represent the natural evolution of an untreated paronychia. The apparent improvement in symptoms observed from an improved paronychial fluctuance and an improvement in pain secondary to a decrease in pressure, should not delay the need for drainage and debridement. Indeed, reacutization is possible if the fistula hole collapses, and ongoing bacterial colonization could possibly lead to a chronic infection or recurrences.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here