Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In 1757 Hunter was the first to describe a patient with compression of the superior vena cava (SVC) by a large syphilitic aortic aneurysm leading to thrombosis. In 1954 Schechter reported a series of 400 patients with SVC syndrome of which 75% were due to malignant neoplasm, predominantly primary lung tumors.
Initial descriptions of surgical reconstruction of the SVC using polytetrafluoroethylene (PTFE), Dacron, or autologous conduits were published in the 1970s. Gladstone and colleagues were the first to report venous decompression using a segment of autogenous femoral vein, and Doty reported successful long-term treatment of SVC syndrome with autogenous spiral vein grafts in 1982.
Surgical treatment is considered for symptomatic patients with benign disease if endovascular treatment is not appropriate because of the extent of venous occlusion or if attempted endovascular treatment is unsuccessful or subsequently fails. Surgical reconstruction in the presence of malignant disease is indicated when curative tumor resection is possible.
Although tuberculosis and syphilitic mediastinitis or aortitis were frequently noted causes of SVC syndrome in the 19th century, lung cancer with metastatic mediastinal lymphadenopathy and primary mediastinal malignancies are now the most common etiologies of SVC syndrome. The most frequent primary mediastinal malignancies causing SVC syndrome include mediastinal lymphoma, medullary or follicular carcinoma of the thyroid, thymoma, teratoma, angiosarcoma, and synovial cell carcinoma. Non–small cell lung cancer is responsible for half of all SVC syndromes, whereas small cell lung cancer, lymphoma, metastatic cancer, germ cell tumors, and thymoma cause the remainder. Although mediastinal fibrosis, most frequently caused by histoplasmosis, was the most frequent cause of benign SVC syndrome in earlier studies, thrombosis because of central lines and pacemaker wires is now the most frequent cause of benign SVC syndrome. SVC syndrome occurs with an estimated prevalence ranging from 1:40,000 to 1:250 people after pacemaker insertion after a mean interval of approximately 48 months. The risk of SVC syndrome is also increased in patients with previous radiation to the mediastinum and in those with thrombophilia.
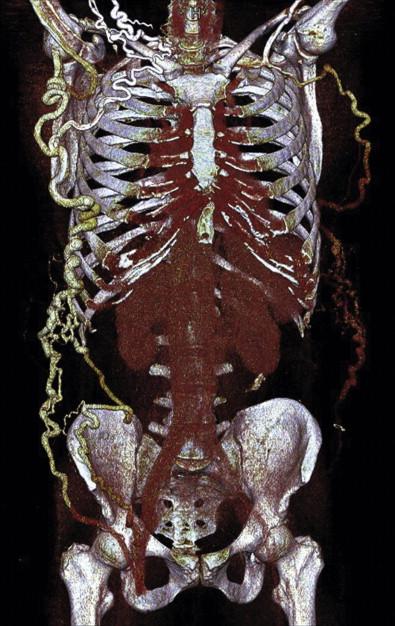
Signs and symptoms. Upper body venous congestion is suggested by the presence of swelling, bluish discoloration of the skin, and dilated veins of the head, neck, upper chest, and less frequently, upper extremities ( Fig. 55-1 ). Complaints include a sense of fullness in the head, headaches, and visual symptoms, which worsen when bending over, as well as dyspnea and dizziness. Sleeping on several pillows because of orthopnea when lying flat is common. Signs and symptoms of malignancy, such as weight loss, lethargy, fever, night sweats, and palpable lymph nodes, in addition to hemoptysis, hoarseness, or dysphagia, may be present.

Imaging studies. Preoperative chest radiography, computed tomography (CT) or magnetic resonance angiography is recommended to evaluate for the presence of benign or malignant disease, as well as to assess the extent of SVC occlusion, to determine the presence of venous collaterals, and to classify the severity of SVC syndrome. Duplex scanning of jugular veins may be helpful for endovascular treatment planning. If the SVC is not adequately visualized by CT ( Fig. 55-2 ) or magnetic resonance imaging, conventional venography should be performed.
Nonoperative measures. A measure of symptomatic relief may be obtained by using pillows to keep the head elevated when sleeping and by avoiding bending over or constrictive garments.
Acute SVC syndrome. Management of acute SVC syndrome includes anticoagulation with administration diuretics to decrease, at least temporarily, edema of the head and neck. Catheter-directed thrombolysis with or without stenting may be considered, followed by intravenous unfractionated or subcutaneous low-molecular-weight heparin and warfarin to prevent recurrence.
SVC syndrome secondary to malignancy. Chemotherapy, radiation therapy, or a combination of both may be used based on tumor histology for patients who have SVC syndrome because of mediastinal malignancy. The tumor shrinks and symptoms resolve in 80% of patients, with the remaining patients considered for endovascular treatment.
Bleeding complications. Bleeding can be excessive during the course of incising skin and subcutaneous tissue, as well as median sternotomy, because of extensive venous collaterals and elevated venous pressure.
Graft thrombosis. Patency grafts in the venous system are inferior because of low venous pressure, especially in patients with a network of collateral circulation, and poor inflow because of extensive venous occlusion. The frequent presence of thrombophilia may also contribute to graft failure, as well as delayed graft stenosis because of intimal hyperplasia or external compression.
Preoperative oral anticoagulation must be stopped at least 5 days before open surgical reconstruction. If bridging with subcutaneous low-molecular-weight heparin is needed, the last dose should be given at least 12 hours before surgical incision. Careful planning, thorough hemostasis, and rapid autotransfusion of blood products are helpful to decrease bleeding and correct blood loss. Finally, collaboration with thoracic or cardiac surgeons may be required in the presence of mediastinal malignancy, in redo median sternotomy, or in placement of the central venous anastomosis at the right atrium, as well as if a concomitant cardiac procedure is required.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here