Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Total Parathyroidectomy with Forearm Autograft for Patients with Advanced Secondary Hyperparathyroidism.
Total Parathyroidectomy with Forearm Autograft for Patients with Advanced Secondary Hyperparathyroidism: Usefulness of IONM.
Secondary hyperparathyroidism (SHPT) refers to the situation in which a derangement in calcium homeostasis leads to a compensatory increase in parathyroid hormone (PTH) secretion. SHPT requiring parathyroidectomy (PTx) occurs more commonly in progressive chronic kidney disease (CKD) but also may occur in long-term lithium therapy and certain disorders of gastrointestinal absorption, deficiency of vitamin D, liver disease, and pseudohypoparathyroidism. The term tertiary hyperparathyroidism (THPT) is associated with clinically persistent hypercalcemia in SHPT after successful renal transplantation (RTx).
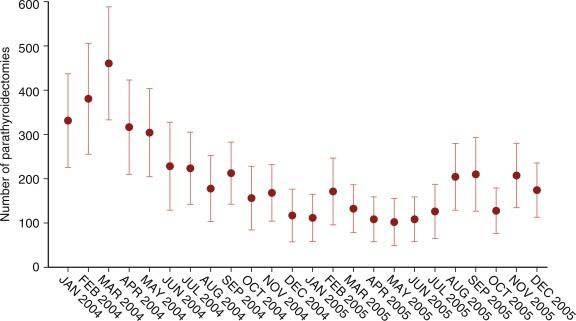
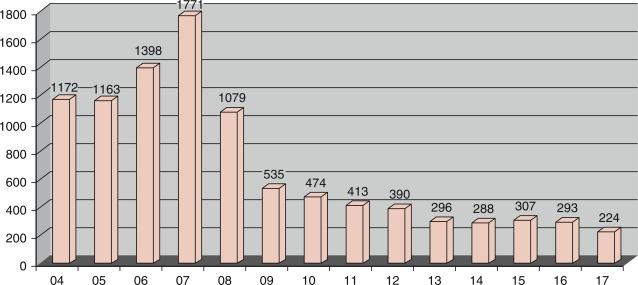
Multivariate analysis showed that younger age, female gender, white race, absence of diabetes, long duration of hemodialysis, use of intravenous vitamin D, previous RTx, and several other comorbid conditions represent risk factors for requirement of PTx in patients with SHPT. Mook et al. found an abrupt decline in the rate of PTx for SHPT over the past decade after introduction of cinacalcet, with stabilization of rates from 2006 to 2011. In hospitals, the mortality rate declined steadily over that timeframe, which suggests either improved surgical and perioperative medical care or an improvement in patient selection ( Figure 61.1 ). The Parathyroid Surgeon’s Society of Japan (PSSJ) has studied the annual number of PTx for SHPT. The annual number of PTx for SHPT increased until 2007, but the rate remarkably decreased when cinacalcet became available in Japan in 2008 ( Figure 61.2 ). The same clinical results have been reported in European countries through The Dialysis Outcome and Practice Pattern Study (DOPS). The overall cost and the cost utility of medical therapy (including cinacalcet) may, to some extent, limit the use of this new therapy; it may, in turn, influence the future rates of PTx in different countries. The Japanese Society for Dialysis Therapy (JSDT) reported that in Japan, the frequency of PTx was about 10% in patients who had had hemodialysis for more than 10 years, and about 30% among those being treated with hemodialysis for more than 20 years.
A summary of pathogenesis of SHPT due to CKD is presented in Figure 61.3 . The dominant etiologic factors are hypocalcemia, reduced renal production of 1,25-dehydroxy vitamin D, and hyperphosphatemia (through phosphate retention), which directly acts on parathyroid cells to stimulate PTH secretion, synthesis, and proliferation of parathyroid cells. Recently, a novel phosphaturic hormone fibroblast growth factor (FGF) 23 has been identified. FGF23 is secreted by osteocytes, and the serum level of FGF23 becomes progressively elevated in CKD. Furthermore, it has recently been shown that FGF23 directly acts on parathyroid cells and mediates secretion of PTH in the presence of Klotho as cofactor.
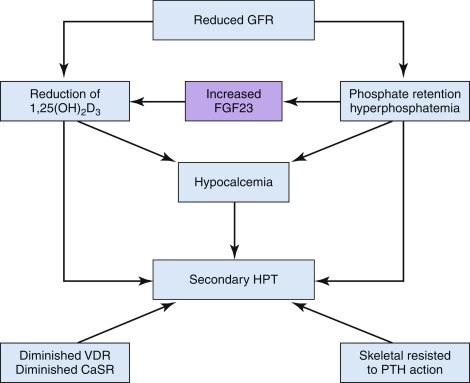
There are numerous derangements in calcium pathways in CKD, which are complex and not completely understood. It has been confirmed that there is diminished expression of calcium sensing receptor (CaSR) in parathyroid cells in patients with CKD. These patients also have skeletal resistance to PTH due to diminished expression of PTH/PTHRP receptor in osteoblasts.
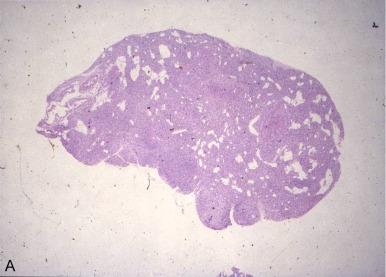
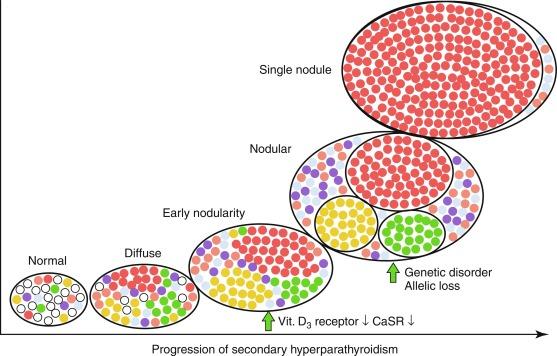
The characteristic histopathological findings of parathyroid glands in patients with CKD include varying degrees of asymmetric enlargement, nodularity, and increase in oxyphilic and transitional oxyphilic cells. Patterns of parathyroid hyperplasia in SHPT are classified into four categories (Tominaga’s classification). They include: (1) diffuse hyperplasia, (2) early nodularity in diffuse hyperplasia, (3) nodular hyperplasia, and (4) single nodular gland ( Figure 61.4 ). Almost all glands exceeding 500 mg display nodular hyperplasia. It has been hypothesized that in CKD patients have polyclonal diffuse hyperplasia which transforms into nodular hyperplasia. In these nodules, parathyroid cells proliferate monoclonally with high growth potential. It has been speculated that the different genetic events known to occur in sporadic primary adenoma may occur in nodular SHPT. The exact nature of these genetic changes and their role in this morphologic progression of SHPT is still unclear.
It has been confirmed that expression of vitamin D receptor (VDR) and CaSR is diminished in these clonal nodules; cells within these clonal nodules have resistance to calcitriol and hypercalcemia. It has therefore been hypothesized when at least one parathyroid gland progresses to nodular hyperplasia, SHPT may be refractory to medical treatments ( Figure 61.5 ).
A number of various medical treatment options exist to control SHPT ( Box 61.1 ).
Phosphate binders
Calcium carbonate, calcium acetate
Sevelamer hydrochloride
Lanthanum carbonate
Ferric contained binder
(Ferric citrate hydrare, sucroferric oxyhydroxide)
Active vitamin D sterols, vitamin D receptor activators
Calcitriol
22-Oxacalcitriol
Falecalcitriol
Alphacalcidol
Paricalcitol
Doxercalciferol
Calcimimetics
Cinacalcet HCl
Etelcalcetide
Evocalcet
First, calcium concentration in dialysate should be optimized. High (3.0 mEq/L), middle (2.75 mEq/L), and low (2.5 mEq/L) calcium dialysates are available (see Box 61.1 ). Calcium carbonate, calcium acetate, and calcium lactate have been prescribed for calcium replacement. This administered calcium acts on the parathyroid cell CaSR to increase inositol phosphate levels in parathyroid cells and increase intracellular calcium level; it serves to suppress PTH secretion as well as parathyroid cell proliferation. Calcium carbonate and calcium acetate are also phosphate binders and can induce ectopic calcifications.
Hyperphosphatemia is one of the causes of ectopic calcification, cardiovascular complication, and mortality. Therefore control of hyperphosphatemia is an essential element of treatment in CKD. Limitation of phosphate in diet and adequate hemodialysis and phosphate binders are fundamental for the treatment. Recently, new phosphate binders (without calcium content) have become available as high molecular polymer (Sevelamar hydrochloride), lantana carbonate, or ferric containing phosphate binders. GI symptoms are sometimes problematic side effects of these drugs.
Deficiency of active vitamin D is one of the main pathogenetic factors for SHPT. Calcitriol and alpha calcidol are common active vitamin D products; however, they induce hypercalcemia and hyperphosphatemia. It was hoped that maxacalcitol (OCT) and paricalcitol, new derivatives of active vitamin D, may allow suppression of PTH without hypercalcemia and hyperphosphatemia. It seems, however, that some degree of elevation of serum calcium and phosphate levels cannot be avoided.
Calcimimetics have been divided into two types: Type I, which mimic extracellular ionized calcium and directly stimulates the CaSR; and Type II, which are positive allosteric modulators.
Common calcimimetics include cinacalcet hydrobromide (a second generation Type II calcimimetic available since 2004), etercalcetide (a positive allosteric 3rd generation calcimimetic), and evocalcet (the most recently available calcimimetic), which has gastrointestinal (GI) symptoms comparable to cinacalcet. Cinacalcet hydrochloride acts on CaSR by allosteric action and enhances sensitivity to extracellular calcium and intracellular calcium signaling. This, in turn, serves to suppresses PTH section and parathyroid cell proliferation. Some patients complain of nausea and vomiting, which can limit cinacalcet compliance.
The majority of patients with SHPT can be managed by the medical treatments that are outlined in Box 61.1 . Kidney Disease Improving Global Outcome (KDIGO), an international workshop, recently proposed clinical practice guideline for CKD-related mineral and bone disease (CKD-MBD). The guideline recommends normalizing serum phosphorus levels. It also recommends that in patients undergoing hemodialysis intact PTH levels should be no higher than two to nine times the upper limits of normal levels for the given assay.
To control hypocalcemia, dialysate containing high calcium concentration usually is used and oral calcium containing phosphate binders (i.e., calcium carbonate or calcium acetate) are taken. Hyperphosphatemia is controlled by removal of phosphorous by adequate hemodialysis, limitation of dietary phosphate intake, and administration of phosphate binders. Treatment for lowering PTH include calcitriol, vitamin D analogues, and calcimimetics. VDR activators easily induce hypercalcemia and hyperphosphatemia and sometimes SHPT may be resistant to these medicines.
Based on existing clinical evidence, Kidney Foundation of the USA proposed the Kidney Disease Outcomes Quality Initiative (K/DOQI) clinical practice guideline for bone metabolism and disease. The guideline recommends in hemodialysis patients for whom serum calcium level is 8.4 to 9.5 mg/dL, serum phosphorus level is 3.5 to 5.5 mg/dL, calcium phosphorous product is less than 55, and intact PTH level is between 150 and 300 pg/mL. This is done to avoid ectopic calcification and cardiovascular complications.
Box 61.2 shows the clinical symptoms and findings of SHPT. Laboratory examination typically reveals remarkably high serum PTH level, hyperphosphatemia, and high bone metabolic markers (total alkaline phosphatase [Al-P], bone specific Al-P, and osteocalcin). Serum calcium level is usually low; however, it is easily influenced by medical treatment.
High turnover bone, osteitis fibrosa
Bone pain, arthralgia, bone loss, skeletal deformity, fracture
Ectopic calcification
Vascular and valvular calcification, tumoral calcinosis, calciphylaxis, calcification in lung, intestine, and stomach
Neuromuscular psychiatric symptoms
Muscular weakness, gait disturbance, irritability, sleeplessness, loss of concentration, depression, etc.
Anemia resistant to ESA, malnutrition, itching, cough
Heart failure (DCM like heart)
ESA,erythropoietin stimulating agent, DCM, dilated cardiomyopathy.
Neuromuscular psychiatric symptoms usually are more severe in SHPT than in primary hyperparathyroidism (PHPT). Patients frequently complain on muscular weakness, irritability, sleeplessness, itching, cough, and other symptoms. Ectopic calcification of vessels and heart valves induce cardiovascular complications and high mortality. Calciphylaxis, cutaneous necrosis induced by calcific uremic arteriolopathy, involves progressive skin necrosis and constitutes a condition of considerable mortality.
Skeletal abnormalities, most often caused by PTH-induced bone resorption, occur relatively early in patients with CKD. These bone disorders come in multiple forms, including classic osteitis fibrosa cystica. Patients often experience skeletal deformation and frequent fracture. Clinically, these patients may demonstrate subperiosteal resorption in digital pharynxes clavicular head, (salt and pepper skull), lumbar osteosclerosis, (rugger jersey spine), and skeletal cystic formation with brown tumor.
Percutaneous Ethanol Injection Therapy (PEIT) was established in Japan and is widely used. Selective PEIT has been used especially for patients with CKD. In the JSDT guideline, PEIT is recommended for patients who have only one enlarged nodular gland. After the enlarged gland is ablated by PEIT, aggressive medical treatment should be continued. After introduction of cinacalcet, the number of PEIT procedures remarkably decreased. If the patient suffers from advanced SHPT and concomitant cardiovascular disease, PEIT should be considered. Recurrent nerve paralysis and hemorrhage after the procedure should be kept in mind as complications of PEIT.
Surgical indications for SHPT are controversial especially after introduction of calcimimetics. Unfortunately, it is unclear as to which particular groups of patients might benefit best from cinacalcet-based medical therapy, and which patients are better treated by expeditious PTx (see Box 61.3 ). Some feel PTx is most optimal as an initial treatment, and cinacalcet therapy becomes an alternate therapy for patients where SHPT is difficult to manage after surgical treatment.
When SHPT is refractory to vitamin D or vitamin D analogues and long-term survival can be expected
When quality of life is highly impaired due to severe SHPT
When cinacalcet treatment cannot be continued due to adverse effects, poor compliance, or other reasons
When sufficient reduction in PTH cannot be achieved with cinacalcet administration
Thyroidectomy for thyroid disease, especially papillary thyroid carcinoma is required concomitantly
SHPT, secondary hyperparathyroidism, PTH, parathyroid hormone.
The surgical indications have been influenced by practical guidelines which vary geographically. All guidelines propose that surgery should be considered when severe SHPT is resistant to medical therapy. PTx for SHPT is a very beneficial treatment; it can stop the progression of cardiovascular complications and improve quality of life and survival.
Previously, surgical indications in SHPT have mainly been based on clear cut severe symptoms or evidence of bone disease. KDIGO guidelines define bone disease (MBD) as a pathologic entity, which includes certain laboratory findings, ectopic calcification, bone fracture. They term this constellation of findings CKD-MBD.
Currently, surgical treatment is seen in the context of the many new forms of medical treatment. VDR agonists, calcimimetics, and phosphate binders without calcium have been documented to suppress PTH secretion and bone turnover. One must, however, keep in mind that medical treatment may induce persistent hypercalcemia and/or hyperphosphatemia; the treatment may be associated with cardiovascular complications which can affect survival.
Although surgical guidelines vary geographically, they all tend to propose that surgery should be considered when SHPT is severe and resistant to medical therapy. PTx has been shown to demonstrate a beneficial effect on survival by reducing cardiovascular complications. PTx performed by expert surgeons generally results in marked sustained reduction in levels of serum calcium, and phosphate.
K/DOQI guidelines from the U.S. Kidney Foundation have proposed that PTx should be recommended in patients with severe SHPT (i.e., patients with persistent serum levels of intact PTH > 800 pg/mL), which is associated with hypercalcemia or hyperphosphatemia and refractory to medical therapy.
A European guideline of clinical algorithms for renal osteodystrophy recommends PTx when a high PTH level (> 50 pmol/L) has not decreased by more than 50% after 2 months of medical therapy, or when there are persistent clinical symptoms and the parathyroid gland diameters estimated by parathyroid imaging are over 1 cm.
JSDT guidelines for medical and surgical treatment for SHPT in 2006 and 2012 ( Box 61.4 ) recommend PTx for severe SHPT refractory to medical treatment and PEIT, if only one parathyroid gland is enlarged, and it is located at a site suitable. The guidelines propose that severe SHPT is present when intact PTH levels > 500 pg/mil is also levels if hyperphosphatemia and/or hypercalcemia are difficult to manage with medical treatment. These guidelines define severe SHPT when high serum PTH vales are present, but it is important to mention that PTH is modified by serum calcium level and influenced by VDR antagonists and calcimimetics.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here