Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Brain abscesses are mostly caused by hematogenous spread, contiguous spread, and trauma.
Contiguous spread is generally from a purulent frontoethmoidal sinusitis or an infected mastoid.
Pyogenic brain abscesses are multibacterial; however, Streptococcus sp. is the most common pathogen.
Capsule removal of parenchymal brain abscesses prevents recurrence.
Spine infections cause rapid neurologic deterioration and become a neurosurgical emergency.
Advanced osteomyelitis of the spine may require complex instrumentation because of the instability.
Postoperative wound infection should be managed with removal of all foreign bodies, foreign implants, and infected bone or soft tissue, as well as with the implementation of a long-term antibiotic regime.
Central nervous system (CNS) infections are frequent, but most do not require any type of surgical intervention. Aggressive CNS infections could become life-threatening situations for which pharmacologic treatment is insufficient for control or eradication. Pathogenic causes of infections are numerous; a full list of the infectious pathogens associated with CNS infection is beyond the scope of this chapter. This chapter addresses only the common primary and secondary infections faced by neurosurgeons. If left untreated, both primary and secondary CNS infections will lead to a fatal patient outcome.
CNS infections became more frequent in the 1980s. Human immunodeficiency virus (HIV)–related infection has been one of the main reasons for this increase. Another common cause is the use of immunosuppressive drugs in organ recipients after transplant surgery and in cancer patients who are being treated with chemotherapy. The early detection and diagnosis of the CNS infection are paramount, because it is easier to treat infections at earlier stages, possibly without surgical intervention. However, often neurosurgeons are still confronted with advanced infections in the brain or spine. This chapter presents an introduction to the surgical management of the most common types of CNS infection.
The incidence of brain abscess and brain empyema ranges from 0.4 to 0.9 cases per 100,000 people. The greater number of immunocompromised patients affected due to HIV infection, immunosuppressive drug use, and higher number of traumatic lesions resulted in an increased incidence. Furthermore, current imaging techniques make it easier to establish an early diagnosis.
For practical surgical purposes, CNS infections could be anatomically divided, affecting different anatomic compartments of the brain: brain parenchyma, the meninges, the ventricles, or extraaxial involvement. The first includes brain abscesses, cysts, or diffuse encephalitis; the second includes meningitis and ependymitis; the third includes ventriculitis; and the last group includes subdural and extradural empyema.
Magnetic resonance imaging (MRI) is the exam of choice for the diagnosis of brain and spine infections. The high resolution of the contrast, multiplane capacity, and signal changes are fundamental for the diagnosis of an infection. Additional MRI configuration techniques can be used to enhance the detection and characterization of CNS infections, configurations such as spectroscopy, diffusion, perfusion, and magnetic transference. When there is bone involvement, computed tomography (CT) scans, plain x-rays, and bone scintigraphy are useful to establish the extent of the infection. Other common laboratory findings for brain abscess and epidural or subdural empyema are elevated white blood cell count and elevated levels of the erythrocyte sedimentation rate and C-reactive protein.
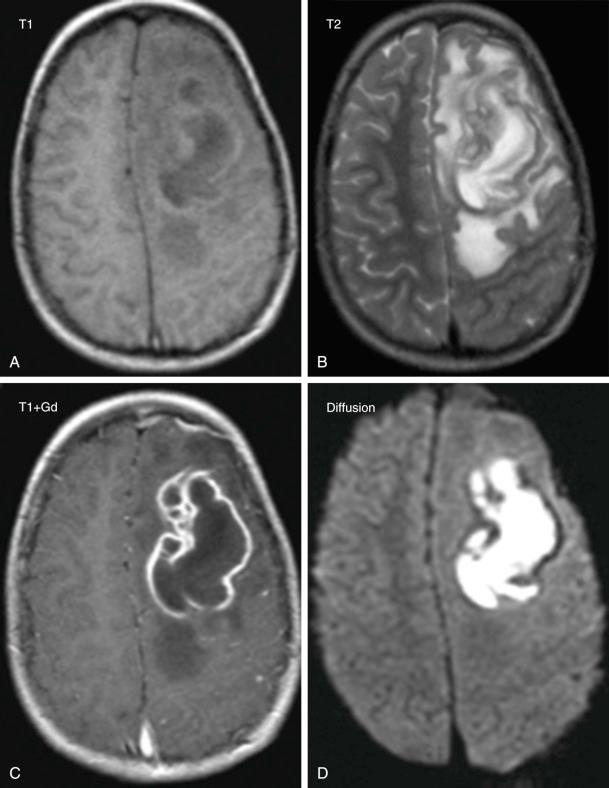
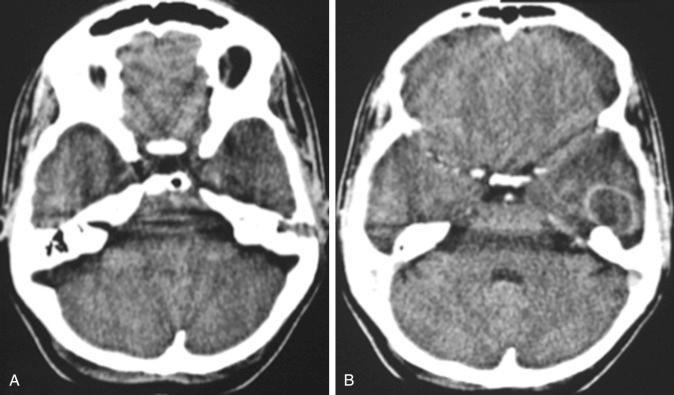
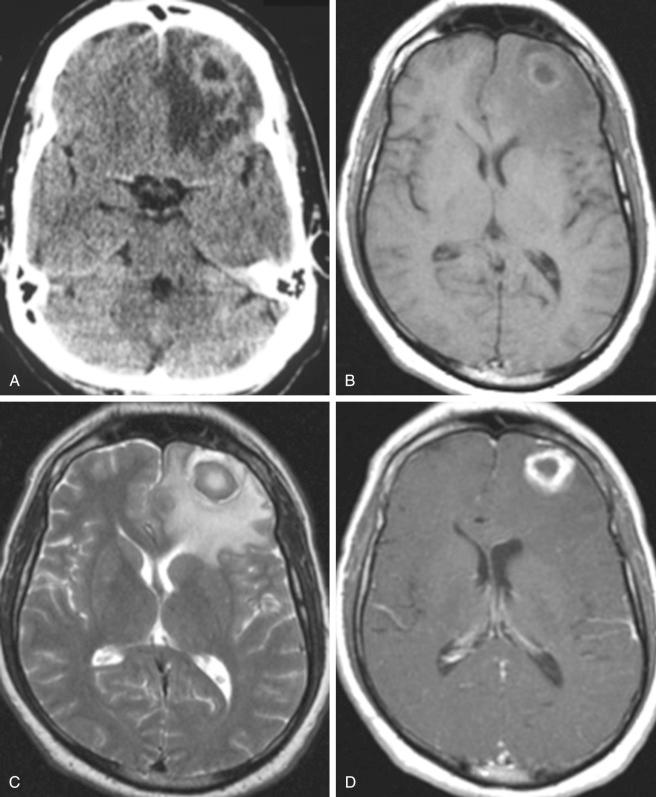
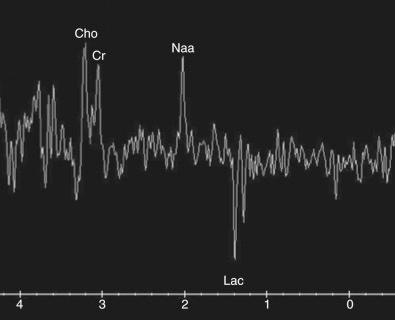
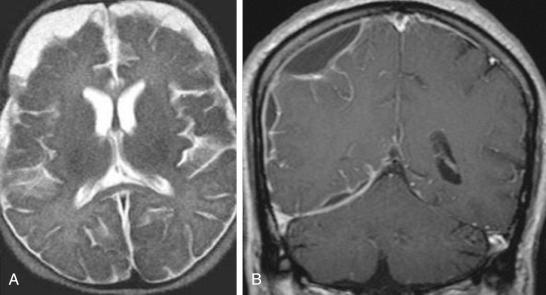
Brain abscess is the result of the proliferation of pyogenic bacteria inside the cerebral or the cerebellar white matter. Brain abscess and empyema culture are, in the majority of cases, inconclusive, with a wide variety of possible pathogens; however, these factors can be positive, and the most frequently identified pathogens and the probable reason for the infection are listed in Table 59.1 . Most commonly brain abscesses are formed through either hematogenous spread or contiguous spread from chronic sinusitis or mastoiditis. Other contiguous causes include head trauma with resulting skull fracture and the opening of the blood-brain barrier, congenital malformations such as dermal sinuses and dural dehiscence, dental infections, and secondary to the radiation of brain tumors and postoperative complications. The image of a fully developed brain abscess is usually an intrinsic parenchymal space-occupying lesion with a large cavity filled with pus and surrounded by edema. On MRI, the fully developed brain abscesses ( Fig. 59.1 ) on T1-weighted images appear hypointense relative to the brain and hyperintense relative to CSF; on T2-weighted images the brain abscesses become hyperintense to the brain and hypointense to isointense in relation to the CSF. Gadolinium enhances the rim surrounding the abscess and delineates the capsule with a hyperintense signal. Earlier stages in the development of a brain abscess are more difficult to diagnose, with the presence of some diffuse infiltrative changes. Brain abscess stages include an early cerebritis (3–5 days); late cerebritis (4–5 days up to 10–14 days); and the capsular stage, which begins at the beginning of the third week and on regular CT scan appears as a diffuse hyperintense lesion and with ring enhancement after contrast injection ( Fig. 59.2 ). The MRI and CT scan imaging of brain abscesses could be confounded with some advanced types of gliomas (particularly with glioblastomas), cystic intrinsic brain tumors, postradiation necrotic lesions, and postsurgical brain alterations ( Fig. 59.3 ). Therefore magnetic resonance (MR) spectroscopy is the method of choice to differentiate between brain abscesses and other lesions with contrast enhancing rims. The MR spectroscopy findings of brain abscesses show high levels of choline (Cho), creatine (Cr), and N -acetylaspartate (NAA) and decreased levels of lactate (Lac) ( Fig. 59.4 ). Glioblastoma multiforme MRI spectroscopy shows different characteristics with increased lactate, choline, lipids, and decreased N -acetylaspartate and myoinositol. MRIs of epidural or subdural empyema ( Fig. 59.5 ) present the following characteristics: epidural empyema typically has a lentiform shape, whereas subdural empyema can have either a lentiform or a crescentic shape. On T1-weighted images, empyema appears to be hypointense relative to the brain and hyperintense relative to the CSF. On T2- and proton-density-weighted images, the collection is hyperintense to the brain and iso- or hypointense relative to the CSF. There is also a ring enhancement on T1 with gadolinium MRIs.
| Predisposing Condition | Common Microbial Isolates |
|---|---|
| Immunocompromise | |
| HIV infection | Toxoplasma gondii , Nocardia and Mycobacterium species, Listeria monocytogenes , Cryptococcus neoformans |
| Neutropenia | Aerobic gram-negative bacilli, Aspergillus species, Mucorales, Candida and Scedosporium species |
| Transplantation | Aspergillus and Candida species, Mucorales, Scedosporium species, Enterobacteriaceae, Nocardia species, T. gondii , Mycobacterium tuberculosis |
| Contiguous spread of bacteria | |
| Penetrating trauma or neurosurgery | Staphylococcus aureus , S. epidermidis , Streptococcus species (anaerobic and aerobic). Enterobacteriaceae, Clostridium species † |
| Otitis media or mastoiditis | Streptococcus species (anaerobic and aerobic), Bacteroides and Prevotella species, Enterobacteriaceae † |
| Paranasal sinusitis | Streptococcus species (anaerobic and aerobic), Bacteroides species, Enterobacteriaceae, S. aureus , Haemophilus species † |
| Hematogenous spread of bacteria | |
| Lung abscess, empyema, bronchiectasis | Fusobacterium, Actinomyces, Bacteroides, Prevotella, Nocardia, Streptococcus species |
| Bacterial endocarditis | S. aureus , Streptococcus species |
| Congenital heart disease | Streptococcus and Haemophilus species |
| Dental infection | Mixed infection with Fusobacterium, Prevotella, Actinomyces, Bacteroides , and Streptococcus species (anaerobic and aerobic) |
* HIV denotes human immunodeficiency virus.
† The Enterobacteriaceae include Escherichia coli and Enterobacter, Klebsiella, Proteus , and Salmonella species.
Up to the formation of the capsule, which normally happens at the end of the second week, the treatment consists solely of intravenous antibiotics. Lumbar punctures should always be avoided because puncture with the raised intracranial pressure can cause cerebral herniation and increased mortality. However, occasionally before the patient undergoes imaging studies, a lumbar puncture has already been performed, and that is particularly common at the initial stages of brain infections when only a meningeal irritation is present. When that is the case, unfortunately the CSF sample rarely can be used for diagnostic and treatment purposes for a lack of a characteristic finding.
CNS infections of the brain can be approached through burr holes or craniotomies. In neurosurgery the three most common types of lesions requiring surgery are brain abscess, epidural empyema, and subdural empyema. Common tools used for the localization of the lesions are stereotactic and neuronavigation systems with intraoperative MRI and intraoperative ultrasound. Among the new developments, fluorescence has also been used for surgery for brain abscesses.
Burr holes can be used when treating epidural or subdural empyemas. However, often the viscosity of the pus makes a craniotomy necessary. If the drainage of the pus and the capsule is subtotal, there is a high probability of an empyema recurrence. Therefore a craniotomy should be performed, as it allows complete drainage of the pus and removal of the capsule. For both types of empyema, epidural and subdural, after the pus is drained and the capsule removed, a continuous irrigation using inflow and outflow of the surgical site with 0.9% saline in combination with antibiotics is warranted.
Surgery for a parenchymal brain abscess should be performed through a craniotomy. The surgeon should approach the abscess with the same microsurgical techniques used to remove intrinsic tumors. The technique requires intergyri dissection through gray and white matter using a large sulcus before reaching the capsulated abscess. Once the abscess capsule is reached, it is carefully opened and the pus is aspirated. Some amount of pus (2–4 mL) should be collected and sent to the laboratory for microbiologic studies. It is important to avoid spreading the pus into the adjacent brain tissue or the ventricle system, because rupture of abscess contents into the ventricles will cause ventriculitis, and pus that spreads to the subarachnoid space will cause meningitis. To avoid this complication, surgical cottonoids should be used to protect the brain and adjacent structures during the capsule opening. After the pus is drained, the resulting cavity should be inspected. The surgeon should then carefully dissect the capsule from the adjacent brain using bimanual microsurgical techniques; one or two brain retractors can be useful during this stage of the procedure to keep the cavity open. Removal of the capsule is of utmost importance, thus this process should be as complete as possible; failure to remove the capsule increases the chance of abscess recurrence. As described earlier for empyema surgery, the resulting brain cavity should be irrigated as long as possible with 0.9% saline and antibiotics; the inflow and outflow should remove all of the remaining capsule fragments along with the debris. After removal of all cottonoids and careful hemostasis, dura closure is performed, the bone flap is replaced, and wound closure follows in a stepwise manner.
If the pyogenic brain abscess was caused by a frontal sinus or a paranasal sinus infection, then the craniotomy has to be large enough to allow the surgeon to open the infected frontal sinus and perform an exenteration of the sinus. Sinus exenteration consists of opening the sinus, removing all the mucosa, packing the sinus with either a viable pericranial flap or fat harvested from the abdomen, and obliterating the lacrimal duct with muscle. For cases in which a pyogenic temporal abscess has resulted from either a middle ear infection or mastoiditis, depending on the etiology of the case, complete management may require a multidisciplinary approach. For example, cholesteatoma of the mastoid is a relatively common cause of temporal brain abscesses, and the treatment requires careful drilling, and opening of the mastoid, followed by excision of the lesion.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here