Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The clinical manifestations of supratentorial stroke, ischemic or hemorrhagic, are usually diagnosed in a timely fashion. However, infratentorial stroke can be indolent, and its diagnosis is often delayed until severe clinical symptoms are evident. The posterior fossa tolerates very little mass effect and can quickly lead to hydrocephalus or herniation. Thus cerebellar stroke, whether hemorrhagic or ischemic, must be managed in a quick and efficient manner. A high suspicion of such pathology should be maintained to act in a timely and appropriate manner. It is the goal of this chapter not only to summarize the diagnosis of cerebellar stroke but to give the reader the knowledge and understanding of surgical intervention when appropriate.
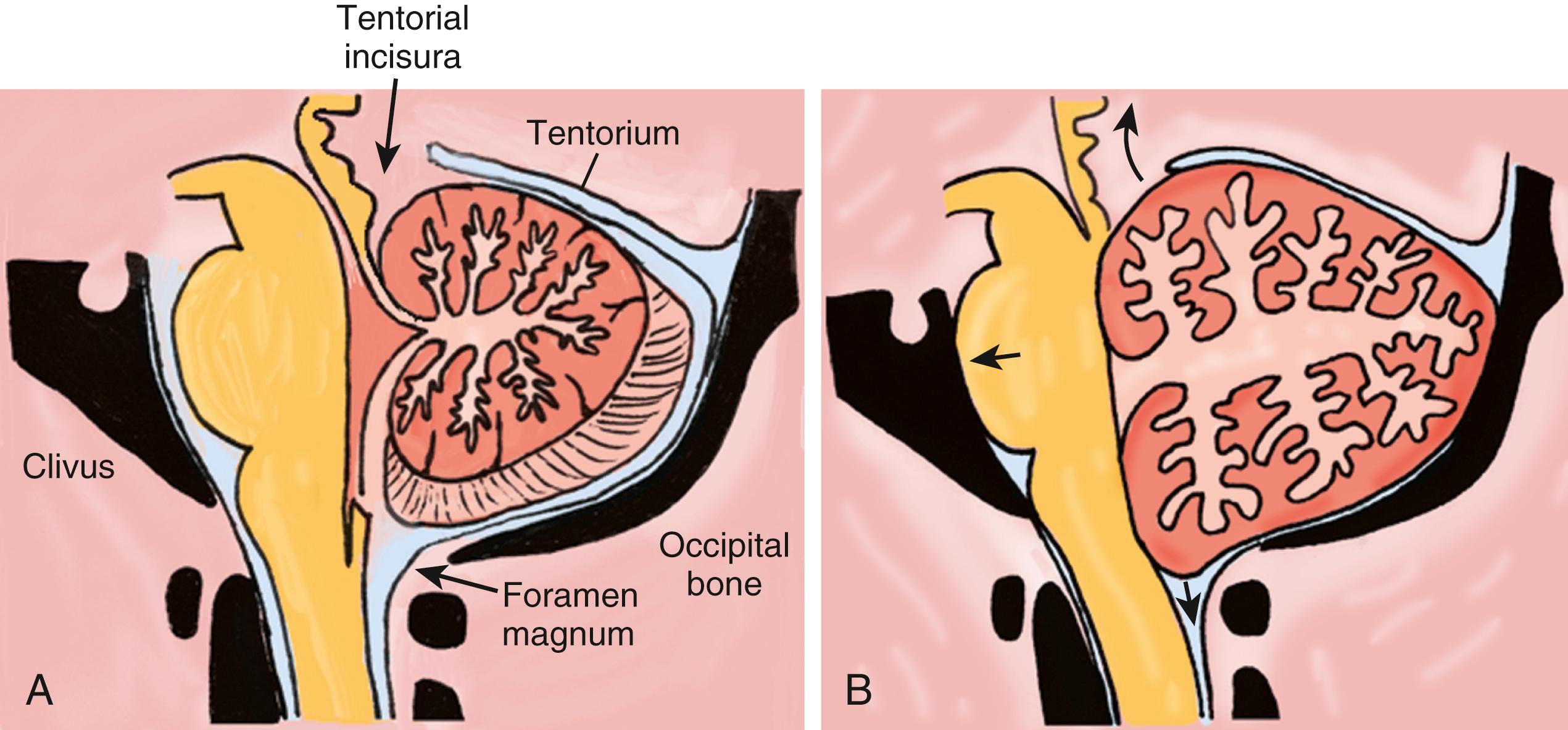
The cerebellum is a unique and fundamental structure of the brain. Composed of two hemispheres and a vermis, the cerebellum occupies the posterior fossa behind the brain stem. The boundaries of the cerebellum are well known and include the tentorium above, the petrous bone and clivus anterior, and the suboccipital skull behind and below ( Fig. 44.1 ). The cerebellum communicates above to the supratentorial space through the tentorial incisura and below to the spinal canal through the foramen magnum.
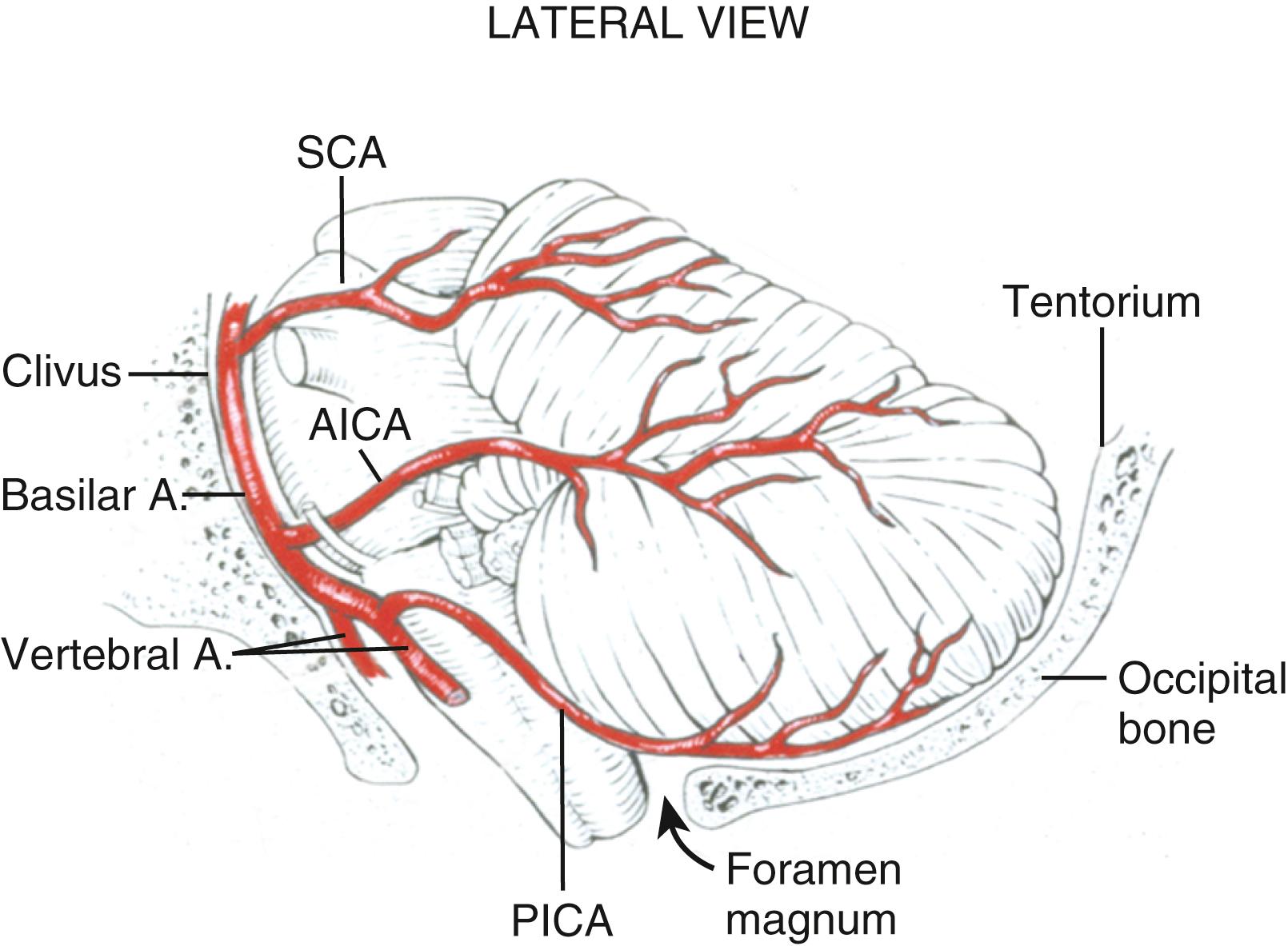
The blood supply of the cerebellum includes multiple branches from the vertebrobasilar system, including the posterior inferior cerebellar artery (PICA), the anterior inferior cerebellar artery (AICA), and the superior cerebellar artery (SCA). PICA originates from the vertebral artery before the vertebrobasilar junction and supplies the lateral medulla, inferior midline vermis, and posterior inferior cerebellar surface. AICA originates most commonly from the inferior portion of the basilar artery and supplies the caudal pons and the petrosal surface of the cerebellum. Finally, the SCA originates just proximal to the basilar terminus and supplies the caudal midbrain and rostral pons, the superior cerebellar peduncle, the dentate nucleus, the superior midline vermis, and the tentorial surface of the cerebellum ( Fig. 44.2 ).
The cerebellar functions include muscle tone, coordination, and equilibrium. It is composed of three layers, the molecular, Purkinje, and granular. There are also four deep nuclei, the fastigial, globose, emboliform, and dentate. Most lesions in the cerebellum cause ipsilateral deficits due to the double crossing of pathways. Most lesions of the midline vermis cause truncal ataxia and dysarthria, whereas hemispheric lesions cause coordination deficits in the ipsilateral hemibody and lesions of the inferior cerebellum cause vestibular dysfunction.
As mentioned, the space of the posterior fossa is much less forgiving than the supratentorial compartment. The Kellie Monroe doctrine holds true, especially in this small area: the three components of this space include brain tissue, blood, and cerebrospinal fluid. If any one of these components is changed, the other two must be modified. Thus a lesion in the cerebellum creates mass effect, thereby obstructing the fourth ventricle or aqueduct, which can lead to life-threatening hydrocephalus. In general, as little as 3 cm of expanding volume may warrant urgent surgical evacuation. The most common causes of cerebellar stroke are found in Table 44.1 .
| Vascular Causes | Other Etiologies |
|---|---|
| Valvular thrombi or vegetations | Hypertension |
| Cardiac embolism | Hemorrhagic transformation of infarct |
| Cavernous malformation | Metastatic lesions |
| Atrial fibrillation | Primary posterior fossa tumor |
| Vertebral artery atherosclerosis | Supratentorial surgery with cerebrospinal fluid drainage |
| Vertebral artery dissection | Patent foramen ovale |
| Arteriovenous malformation | Hypercoagulable state |
| Venous sinus thrombosis | |
| Vasculitis/vasculopathy |
The most common cause of cerebellar hemorrhage is hypertension. Hypertensive hemorrhages occur equally in the hemisphere and vermis. The region of the dentate nucleus is often involved, due to its supply from perforating arteries of the SCA. Other causes of cerebellar hemorrhage include vascular lesions such as arteriovenous malformations, cavernous malformations, and tumors such as metastatic melanoma and renal cell carcinoma with propensity to bleed. Patients with coagulopathy, cerebral amyloid angiopathy, and/or patients on blood thinners are also at increased risk. Cerebellar hemorrhage may only involve the parenchyma but can also extend into the fourth ventricle and aqueduct leading to obstructive hydrocephalus.
Most cerebellar infarcts are due to thromboembolic mechanisms. The common sources are atherosclerosis in the vertebral artery system, paradoxical embolism from a patent foramen ovale in young patients, and vertebral dissection. Entities such as trauma, vasculitis, venous sinus thrombosis, and vasospasm related to cocaine use are also possible causes of cerebellar infarct.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here