Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Non-melanoma skin cancer (NMSC) is the most common type of cancer and has multiple management options.
Surgical excision remains an efficient, effective, and safe method for the treatment of these tumors, particularly with thorough perioperative planning.
Excision has advantages over destructive treatment modalities because it allows for histologic evaluation of margins and tumor characteristics that may influence further management.
Various patient and tumor qualities support surgical excision as an appropriate approach to treating NMSC with consistently acceptable cure rates.
Certain situations argue against treating NMSC with standard excisional techniques.
Non-melanoma skin cancers (NMSC) are the most common among all human malignancies, with their incidence approaching that of all other cancers combined. Fortunately, mortality from these tumors is low, but their management cost to the medical system is quite high. In the US, NMSC ranks fifth among all types of cancer in healthcare expenditures, while in Australia it ranks first.
Because of their contiguous growth pattern and low metastatic potential, these tumors are well suited for standard surgical excision, which can be performed under local anesthesia in an office-based setting with relatively low associated risk and cost and high cure rates. Prior to performing these procedures, the surgeon must be familiar with several factors that influence their execution in order to optimize cure rates while minimizing destruction of uninvolved tissue
Multiple patient- and tumor-associated features must be evaluated while planning surgical excisions for NMSC. A thorough history and physical examination is of paramount importance and should be performed prior to any surgical procedure in order to avoid potential adverse events. Medication allergies should be discussed, as well as complete review of all medications that the patient is currently taking and the patient's medical diagnoses. Factors such as age, general state of health, and anxiety level will directly influence how well a given patient will be able to tolerate a procedure under local anesthesia, and, in certain cases, general anesthesia or conscious sedation may be more appropriate. Patients should be cognizant of what to expect throughout the procedure as well as in the postoperative period, including activity restrictions and the need to return to the office for suture removal if necessary. Although surgical excisions are considered extremely safe procedures, with infection and bleeding as the most common adverse events, the potential for serious undesirable complications does exist.
Medical conditions such as diabetes mellitus, acquired immune deficiency syndrome (AIDS), organ transplantation, cancer, chronic disease, and nutritional deficiency are all associated with some degree of immunosuppression and can potentially increase the risk for infection. Antiseptic handwashing with either scrub and water or alcohol-based products can significantly reduce the incidence of infection and should be employed prior to every procedure. Likewise, a variety of preoperative antiseptic skin preparations are available and should be used to disinfect the skin of the patient. The skin should be cleansed in enlarging concentric circles, beginning at the site of excision and extending beyond the area to be covered by sterile drapes. Patients should be instructed to bathe the evening before or the morning of their procedure, as this has also been shown to reduce the rate of infection. Interestingly, preoperative shaving of hair has been linked to higher wound infection rates, presumably by causing small cuts or scratches in the skin, thus providing portals of entry for infection. If hair is to be removed prior to surgery (e.g. on the scalp or on the chest of a man), scissors should be used as opposed to a razor. Additionally, infections at sites distant to the operative location increase the risk for postoperative wound infections, and should be addressed prior to excisional surgery.
The use of prophylactic antibiotics in dermatologic surgery has been an evolving issue, most recently reviewed in the advisory statement published by the American Academy of Dermatology (AAD). Bacteremia has been documented to occur during cutaneous surgery at rates ranging from 0.7% to 7%. This value is similar to the rate of spontaneous bacteremia in healthy adults, and far less than the rates of bacteremia that occur with activities of daily living such as mastication, brushing teeth, or defecation. The American Heart Association (AHA) has published guidelines for the prevention of bacterial endocarditis and recommends antibiotic prophylaxis for procedures causing bacteremia greater than 10% of the time, making antibiotic prophylaxis unnecessary for cutaneous surgery unless mucosal skin is involved, the operative site is inflamed or infected, or in high-risk patients. In these situations, antibiotics should be administered as a single dose 1 hour prior to surgery.
Antibiotic prophylaxis may also be considered in certain patients with prosthetic devices. In high-risk patients or in high-risk locations such as nasal mucosa or the perineum, preoperative antibiotics may be considered. The use of antibiotics, however, should be balanced with their potential side effects, including the emergence of resistant strains of bacteria, severe allergic reactions, cost, and serious interactions with medications such as warfarin. Ultimately, the decision to administer prophylactic antibiotics should be made on a case-by-case basis, with definite indications for use being few in number.
Inevitably, despite proper precautions, wound infections will occur and typically present within the first week after surgery with pain, erythema, warmth, and purulent drainage. Sutures should be removed to allow drainage and cultures should be collected for correct identification of the causative organism and selection of appropriate antibiotics. First-generation cephalosporins are generally accepted as first-line empiric treatment until culture and sensitivity results are obtained.
Although the risk of postoperative bleeding is low, it remains the most common complication of dermatologic surgery, and steps taken beforehand can help further reduce this risk. Of note, over-the-counter dietary supplements can also impact proper coagulation and are often overlooked in history-taking by physicians and medication lists provided by patients. The indication for anticoagulation is an important factor in determining whether it should be discontinued. It may be prudent to check the international normalized ratio (INR) level prior to surgery to confirm that it is not beyond the therapeutic range; however, a recent study of perioperative bleeding in patients taking warfarin demonstrated that patients who were taking warfarin and experienced a moderate-to-severe bleeding complication had INR levels less than 2.6 (well within the therapeutic range) at the time of surgery. Hurst and colleagues have provided a set of recommendations regarding perioperative management of anticoagulants including: 1) primary preventative aspirin should be discontinued 10–14 days prior to surgery and restarted 1 week afterwards; 2) medically necessary warfarin and aspirin should be continued with an INR value measured within 1 week of the procedure; 3) NSAIDs should be stopped 3 days prior to surgery with resumption after 1 week. The authors recommend continuation of clopidogrel. However, no studies have investigated its use or the use of combination anticoagulant therapy.
Despite meticulous intraoperative hemostasis, both immediate and delayed bleeding will occur, typically within the first 48 hours after surgery. Postoperative bleeding can often be controlled by patient-applied pressure and ice; however, patients with signs and symptoms concerning for hematoma formation should be evaluated as soon as possible and managed appropriately.
Electrosurgical instruments are often used for hemostasis during skin surgery and may interfere with the proper function of pacemakers and implantable cardioverter-defibrillators (ICD). Interference may lead to inappropriate triggering of pulses, inhibition of proper triggering, or alteration of the programming of the device. Despite recent advances in the circuitry of pacemakers and ICDs, recommendations published in 1998 for patients with cardiac devices undergoing dermatologic procedures were not changed significantly from suggested guidelines posed in 1975.
When possible, in patients with implantable cardiac devices who are in need of surgery, thermal cautery is the safest alternative as no electric current is passed through the patient. Other suggested precautions include the use of short (<5 second) bursts of current for electrocautery, minimal use of power, and avoiding usage of electric current in the immediate vicinity of a cardiac device. When in any doubt, consultation with a cardiologist should be obtained. Cardiac crash carts and staff trained in advanced cardiac life support should also be present in any dermatologic surgical facility.
Preferably, a diagnostic biopsy has been performed prior to excisional procedures, as these results along with patient and tumor characteristics contribute directly to the decision to proceed with a given course of management. The ideal treatment option considers not only long-term recurrence risk, but also risks associated with the procedure itself, comorbidities, as well as patient needs and expectations.
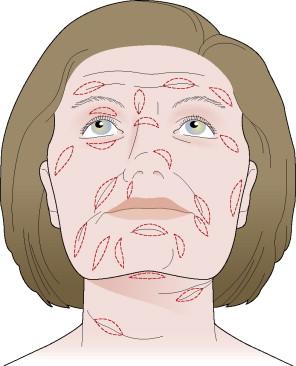
Most commonly, lesions are excised with a fusiform ellipse ( Fig. 46.1 ) with a long axis oriented along relaxed skin tension lines (lines of Langer), or variations thereof ( Fig. 46.2 ). The length-to-width ratio should be between 3:1 and 4:1 and the angles formed at the ends should approximate 30° to avoid producing standing cones (dog-ears) at the poles. Once the tumor has been excised, the wound edges are undermined to reduce tension across the wound and to enable eversion of the edges. The defect is then closed primarily. Typically, dissolving deep sutures are placed to close dead space and remove tension from the wound. Cutaneous sutures are then placed to finely approximate wound edges and provide additional eversion for optimal wound healing and cosmesis.
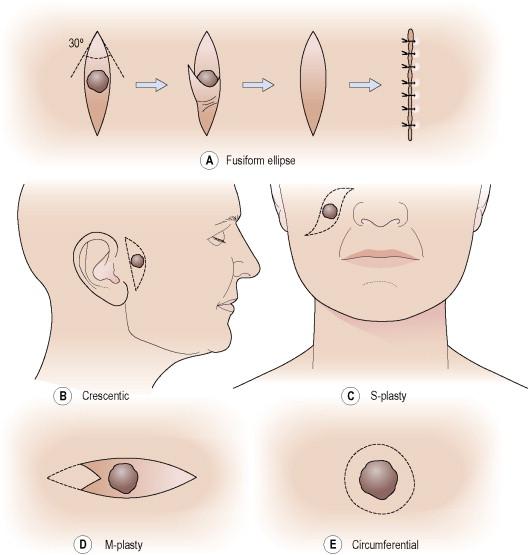
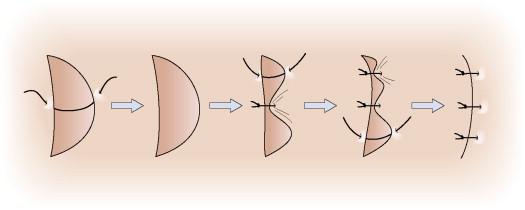
Alternate approaches include crescenteric closures in areas such as the preauricular cheek or near the nasolabial fold where the relaxed skin tension lines are curved. When suturing such an excision, the side with greater curvature will have tissue redundancy. Crescentic excisions are best closed using the rule of halves to equally distribute the excess tissue along the length of the defect ( Fig. 46.3 ). In areas where the relaxed skin tension lines lie in opposite directions at the edges of the ellipse or on convex surfaces, an S-shaped or curvilinear approach may be used. M-plasty is a technique used to decrease the length of a scar when encroaching upon vital anatomic structures (see Fig. 46.1 ). In instances where the relaxed skin tension lines cannot be adequately determined, lesions can be excised circumferentially.
In certain situations, such as for large tumors or in areas of minimal tissue movement such as the scalp or pretibial region, primary closure may not be possible. In such cases, circumferential excision can be planned with subsequent purse-string closure or healing by secondary intention.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here