Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Sudden cardiac death (SCD) is defined as death after a sudden cardiac arrest (SCA) in a patient with either known or previously undetected cardiac abnormalities in whom the mode and time of death are unexpected. Transient endogenous influences on cardiac physiology, such as electrolyte, metabolic, or respiratory disturbances, or exogenous factors, such as drug effects or chest wall trauma (as in commotio cordis ), contribute to expression of underlying risk. Although unexpectedness is a key feature of the SCD definition, clinical disorders that underlie predisposition to SCA, such as heart failure or transient ischemia, have been identified. However, despite knowledge of these predictors, a large proportion of SCAs and SCDs occur as the first clinical expression of cardiac disease, as in patients with previously unrecognized ischemic heart disease or inherited structural disorders and nonstructural arrhythmogenic disorders (channelopathies).
One generally accepted temporal definition is an interval of up to 1 hour between the onset of an abrupt change in clinical status and loss of consciousness because of cardiac arrest, although other definitions include up to 6 hours. This time period defines the onset of SCA, but the absolute definition of biologic death, which could be delayed for days to a month or more by life-support interventions after central nervous system injury resulting from the SCA, should be used in population studies and clinical analyses. Finally, the distinction between SCA as the event and SCD as the outcome should be considered in any definition.
For the last 30 years of the 20th century, the incidence of out-of-hospital SCD in the United States was estimated at 300,000 to 350,000 events per year. These estimates were derived from a broad-based accumulation of clinical and population data available at the time, rather than from direct epidemiologic studies providing national statistics that included representation from various regions of the United States and other countries. During the first decade of the twenty-first century, conflicting statements have been put forward regarding the current incidence of SCD ( Fig. 79.1A ). These newer estimates were derived from retrospective death certificate analyses and extrapolations from SCD incidences identified in specific communities. For example, an estimate from the statistical handbook of the American Heart Association (AHA), based on data from the National Center for Health Statistics (NCHS) and the National Heart, Lung, and Blood Institute, suggested an annual incidence of fewer than 250,000 SCDs. An additional analysis from the Seattle, Washington, emergency medical system (EMS) database, extrapolated to total US population numbers, calculated 184,000 cardiac arrests nationwide in the year 2000, which is a significant decrease compared with 1980 statistics. Another community-based study from Oregon, based on prospective medical examiner data plus other sources of data, also yielded a national extrapolation of fewer than 200,000 cardiac arrests. In contrast, a death certificate–based study, also from the NCHS, has suggested that more than 50% of all cardiac deaths are sudden and estimated the total annual incidence of SCD to be in the range of 460,000. In the most recent statistical update from the AHA, the estimated annual number of EMS-assessed SCAs in adults in the United States is 347,322. Other sources suggest more than 400,000 EMS responses to cardiac arrest. Combining statistics from several sources, in addition to accounting for actual deaths by subtracting survivors, this figure returns to the rate of 300,000 to 350,000 SCDs annually, with somewhat lower numbers in specific locations as cited earlier. Despite these various estimates, an accurate count of the SCD burden in the United States will require reporting of all cardiac arrests in a national registry, which should include data on sites, causes, responses, and outcomes.
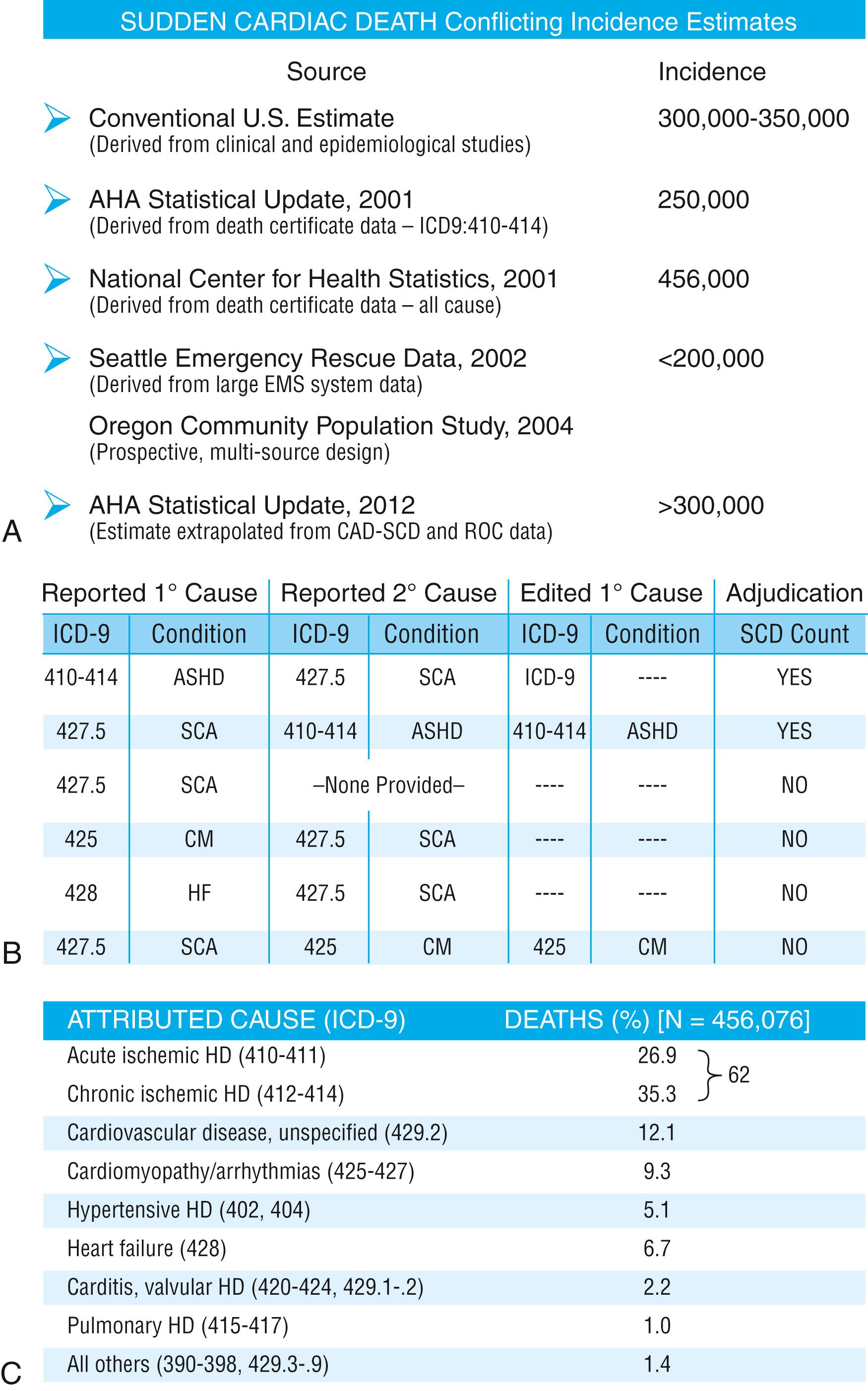
The large discrepancy between the two estimates from NCHS death certificate data stems from differences between the definitions of SCD used and the population sources. The AHA restricted its application of the NCHS data solely to coronary heart disease–related deaths, based only on International Classification of Diseases–Ninth Revision codes 410 to 414 (see Fig. 79.1B ), whereas the cumulative NCHS data included almost all causes of SCD (see Fig. 79.1C ). The much broader range of inclusion in the latter study resulted in the much larger estimate, perhaps overestimating the true incidence. The Seattle data include only SCDs involving emergency rescue responses, whereas the Oregon study population is not necessarily representative of the incidence variations within the entire US population. National estimates remain uncertain because of the hazards of relying on death certificate classification and on extrapolations from a few large population centers of excellence that might not be representative of smaller metropolitan statistical areas constituting the majority of the US population. This limitation could affect appropriateness of regional response strategies and outcomes, in addition to knowledge of the true population burden.
The strongly emphasized continuous reduction in age-adjusted risk of coronary heart disease mortality in the United States beginning in the 1970s, when translated to total number of events and size of populations at risk for future events, cannot be interpreted to mean that the absolute burden of SCD events has decreased. General preventive therapies and lifestyle modifications for controlling risk factors for coronary heart disease, plus interventions in acute coronary syndromes, have likely contributed to a population effect on evolution of disease and the reduction in age-adjusted mortality rates. However, these therapies, lifestyle modifications, and interventions have not had a proportional effect on SCD incidence, especially in low-risk subsets with large denominators and high absolute numbers of events. The previous emphasis on post–myocardial infarction patients with reduced ejection fractions as a source of large numbers of events is currently lower because of early recognition and intervention for acute coronary syndromes, but counterbalanced by risk associated with unrecognized silent myocardial infarctions and that associated with previously unrecognized coronary atherosclerosis. Based on existing data, it appears that the total numerical burden of SCD has not changed significantly over the last 30 years, even though underlying disease burden has, and SCD accounts for an increasing proportion of cardiovascular deaths, constituting 50% of cardiac deaths in the United States and Northern Europe. , The limitations of the various sources and the reliability of currently available data suggest that a prospective epidemiologic study, designed to provide accurate counts of SCDs and its specific mechanisms, including proportional representation from metropolitan statistical areas of different sizes, would be a valuable investment to help plan for future health needs, community response system designs, and clinical research targets.
The previous statements are limited to the specific problem of out-of-hospital SCAs (OHCA) and related SCDs. Another large group of SCAs, estimated at approximately 200,000 per year in the United States, occur in-hospital (in-hospital cardiac arrest [IHCA]), with approximately 75% resulting in death.
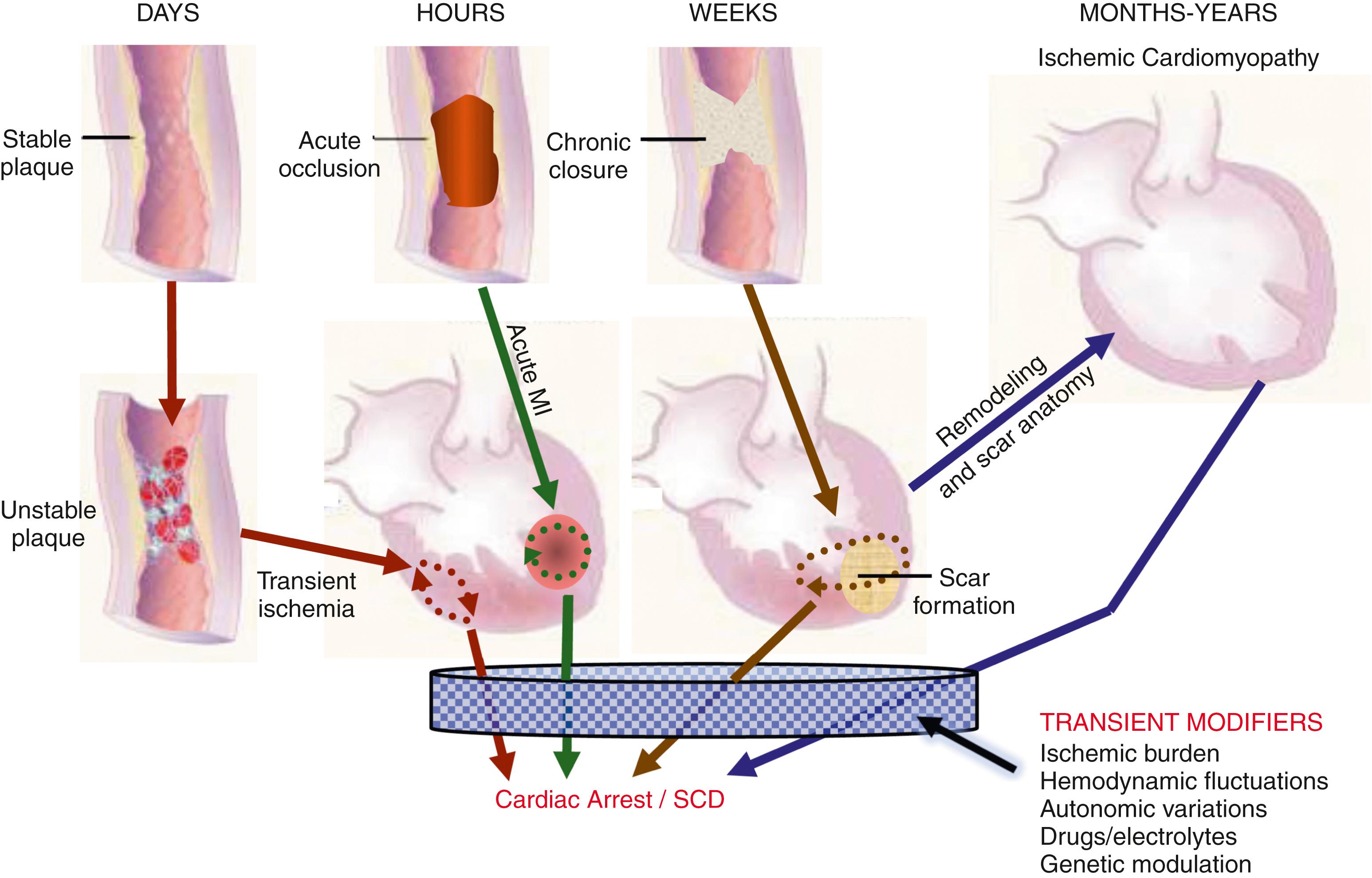
The etiologic basis for SCD can be analyzed in the context of two general categories: substrate-based causes and expression-based triggers. Substrate-based causation refers to the presence of vascular, myocardial, or molecular substrates associated with SCD risk. In parallel, expression risk refers to the identification of mechanisms that contribute to the clinical expression of the risk predisposed by the substrate and transient risk factors. In the case of SCD caused by coronary heart disease, the latter include the plaque transition and acute syndrome modules in Fig. 79.2 (plaque disruption and thrombogenesis) and their subsequent expression as an arrhythmic event (arrhythmogenic module) in the susceptible individual. The arrhythmogenic category of pathophysiology can also be viewed to include modifiers of molecular-based risk that drive individual expression.
Among the general population in the Western hemisphere, coronary heart disease is the most common substrate for SCD. Although estimates vary, approximately 75% to 80% of all SCDs in the United States and Western Europe had been associated with this underlying substrate in the past, but have appeared to have reduced in the last 2 decades to the range of approximately 70%. , Cardiomyopathies compose the second most common category of disorders associated with SCD. Many definitions of this category include both dilated cardiomyopathy (DCM) and hypertrophic cardiomyopathy (HCM), but the hypertrophic form is more appropriately counted among the rare genetic syndromes associated with SCD risk, for both clinical and epidemiologic reasons. DCMs collectively account for 10% to 15% of all SCDs, including both acquired and inherited forms. There is debate about the proportion of DCMs in the two groups, but it could be in the range of a 50 to 50 distribution. Many studies of SCD risk and interventions fail to distinguish between DCM as an etiology and congestive heart failure (CHF) as a clinical expression. Among women, SCD is more frequently associated with nonischemic cardiomyopathy than among men, and generally women are older than men at the time of SCD.
Various infiltrative, inflammatory, and valvular diseases constitute the underlying causes in most of the remaining SCDs. Viral or autoimmune myocarditis, whether manifest clinically or silent, can be associated with SCD. The frequency of this disorder is uncertain because of the difficulty validating its presence, even histopathologically. It has been considered to be among the more common causes of SCD in adolescents and young adults, but its incidence is debated because many of the estimates are derived from studies that predated the consistent definitions established by the Dallas criteria. Currently, there is emerging evidence for coronavirus-associated viral cardiomyopathy and a potential current and future concern. The recognition of persistence of viral DNA fragments in myocytes of SCD victims, even without inflammatory markers, further confounds the issue. Early data attributed this mechanism to the consequences of adenovirus and coxsackievirus infections, with uncertainty about other families of viruses.
SCD can be sporadically associated with virtually all of the less common systemic conditions that can have cardiac involvement. These include chronic granulomatous diseases, autoimmune disorders, infiltrative diseases, various cardiac tumors, and protozoan infestations. Among the granulomatous diseases, sarcoidosis is the most prominent because of the frequency of its association with SCD. The risk of SCD has been associated with ambient arrhythmias, such as nonsustained ventricular tachycardia. Cardiac amyloidosis is also associated with SCD, with a reported incidence of 30%.
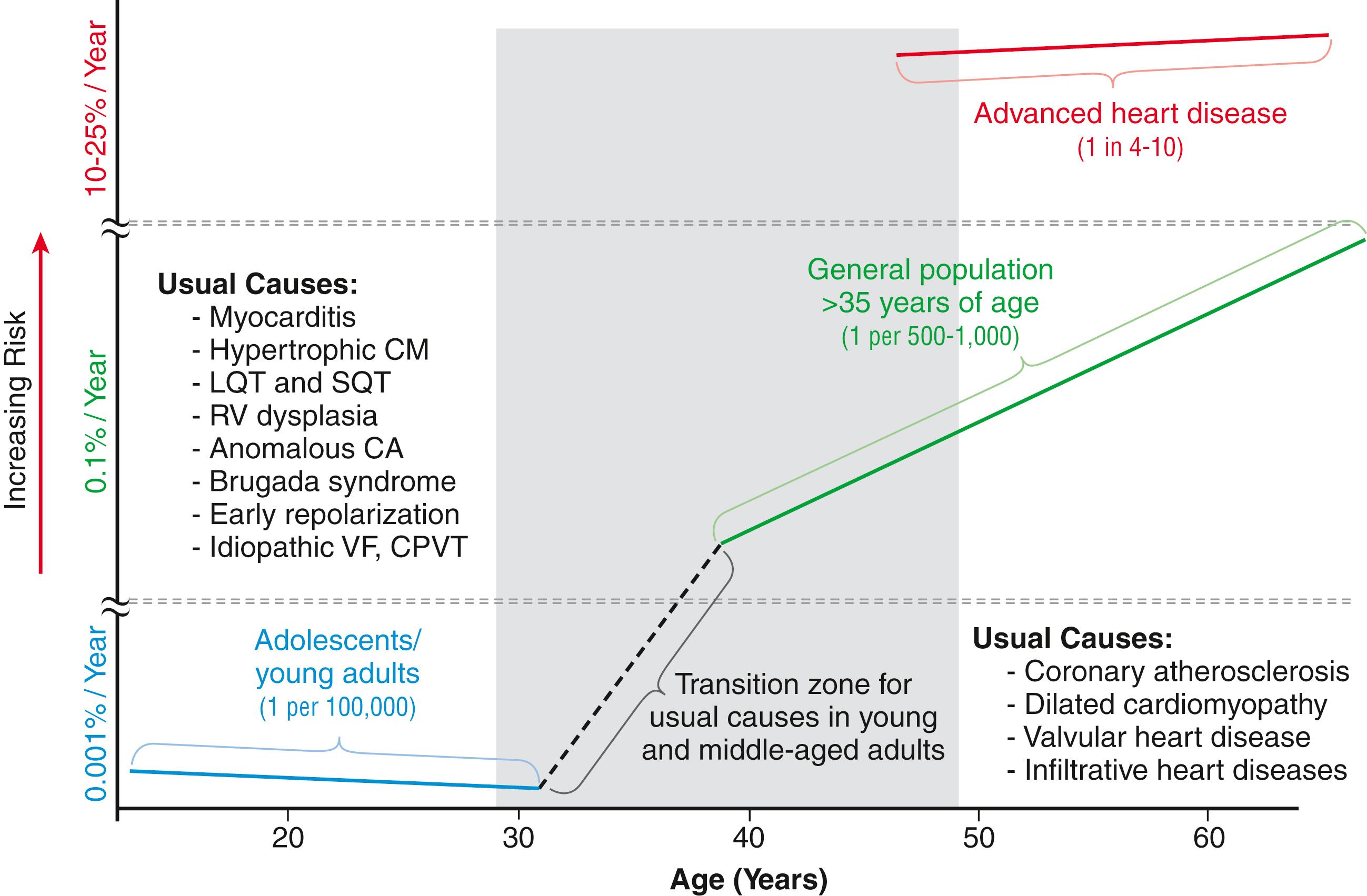
Only a small proportion of SCDs in middle-aged and older adults are caused by rare genetically determined disorders, such as long QT syndrome, Brugada syndrome, HCM, and right ventricular dysplasia, or to developmental congenital disorders, such as aortic stenosis and anomalous origins of coronary arteries. Cumulatively, these rare disorders account for no more than 1% of the total SCD burden, but the proportionate contributions of these disorders are distinctly age related. Among adolescents and young adults, these disorders (in addition to myocarditis), are major causes of SCD, whereas coronary heart disease and the DCMs dominate beyond the age of 35 years. A transition occurs in the age range of 30 to 45 years, in which the rare disorders comingle with increasing prevalence of coronary heart disease ( Fig. 79.3 ). Entities such as Brugada syndrome and right ventricular dysplasia, in addition to long QT syndrome with expression caused by proarrhythmic drug exposures and electrolyte disturbances, are those that are most likely to blend with the progressively increasing prevalence of coronary heart disease and nonischemic cardiomyopathies in this age range. It is now becoming generally recommended that middle-aged, young adult, and adolescent individuals with autopsy-negative SCD undergo postmortem genetic testing, both for clarification of cause and potential relevance for family members. Finally, it is becoming increasingly apparent that HCM may evolve into a more general cardiomyopathy, having features of a DCM, with advancing age. An increasing number of such cases are being recognized later in life, many of which had not been diagnosed previously.
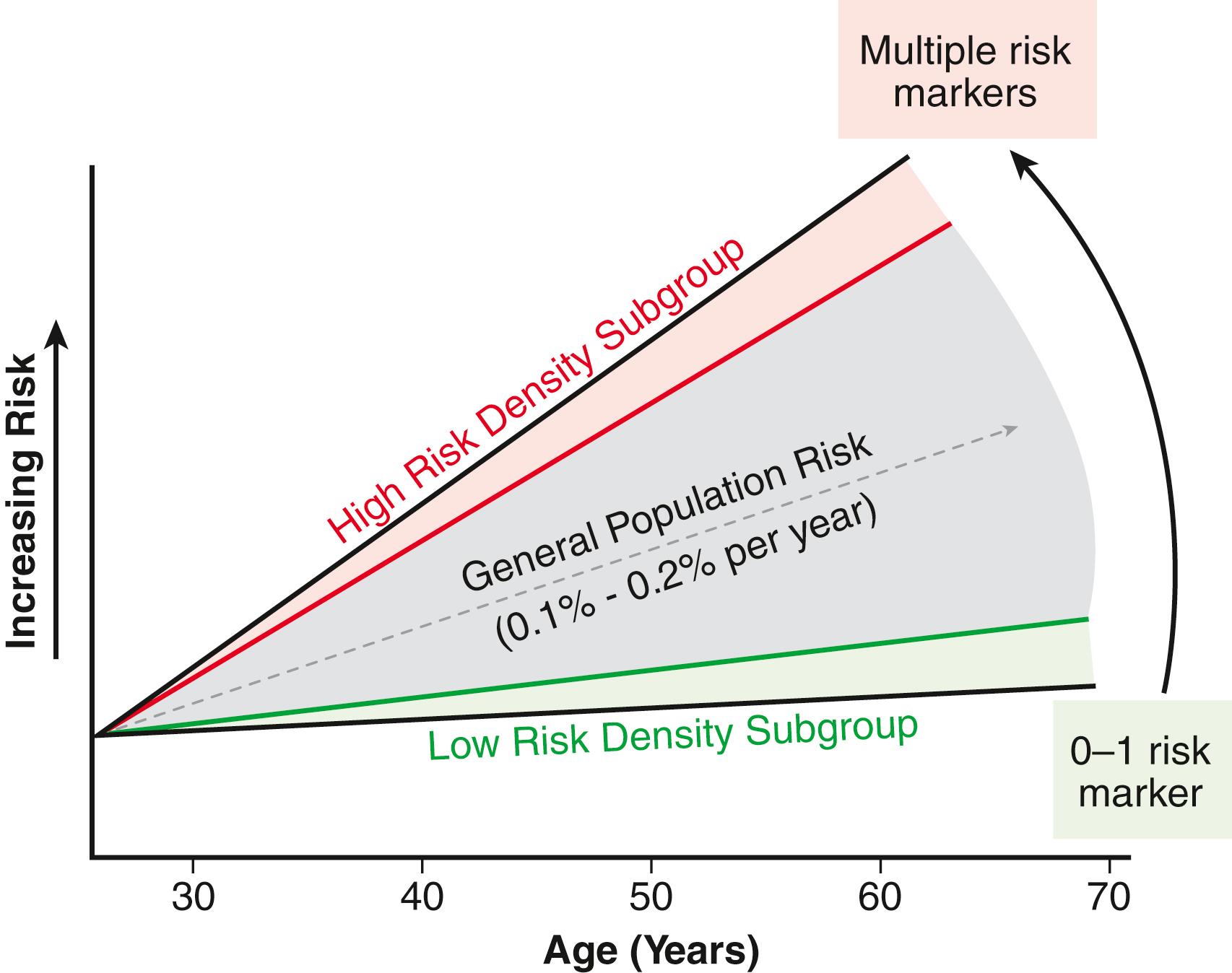
For the general population older than 35 years, the average mortality rate is subgrouped into pockets of higher- and lower-risk densities, based on numbers and power of risk factors. However, currently available profiling strategies do not have sufficient power to identify small groups with high-risk density that would permit meaningful individual risk prediction ( Fig. 79.4 ).
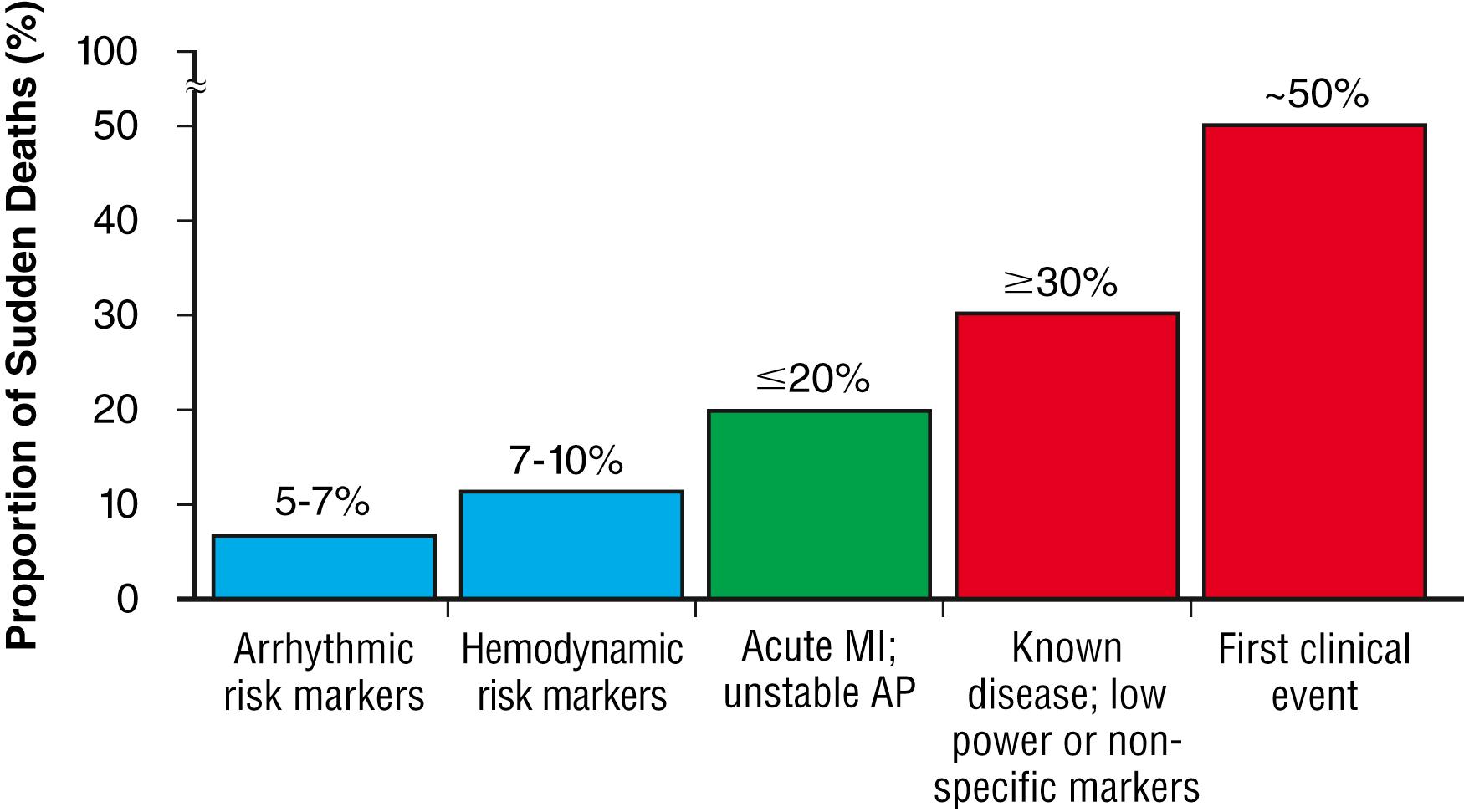
The spectrum of patterns of clinical expression of SCA/SCD syndrome ranges from anticipated events in high-risk patients with identified advanced heart disease to those with unrecognized or new-onset conditions in which SCD is the first clinical manifestation ( Fig. 79.5 ). An intermediate category of patients have known heart disease but are considered to be at low risk based on extent and stability of disease. Among the highest risk categories are subgroups characterized by low ejection fractions, with or without heart failure, after myocardial infarction or caused by nonischemic cardiomyopathies. Various other myocardial or valvular conditions are also associated with high risk. Among these groups of patients, the probability of a potentially fatal SCA is high, but the positive and negative predictive accuracies of most methods of profiling risk for individual patients are still somewhat limited. At the other end of the risk spectrum, patients with known heart disease but low-risk markers (e.g., ejection fractions greater than 40%, no heart failure, no arrhythmias) contribute a large absolute number of SCDs because of the vast number of patients that reside in this low-risk group. In addition, cardiac arrest is commonly the first clinical manifestation of the underlying disease in subjects without previously identified heart disease. Postmortem studies of cardiac arrest victims have shown that previously silent disease in such subjects is often advanced. The last two categories account for approximately two-thirds of all SCDs.
Much of the information available on the pathologic anatomy in SCD victims reflects the predominance of coronary heart disease as the major underlying etiologic disorder. Both the extent of coronary artery disease and the resulting abnormalities in ventricular myocardium have been well described. Extensive coronary atherosclerosis has been recognized for many years as the primary anatomic hallmark of coronary heart disease–related SCDs. Also, SCD closely associates with the presence of plaque fissuring or erosion, platelet aggregation, and acute thrombosis within the matrix of coronary atherosclerosis. This feature of coronary artery anatomy, superimposed on chronic lesions, does not differ among the three primary expressions of acute coronary syndromes: SCD, acute myocardial infarction, and unstable angina pectoris. Various studies have demonstrated the presence of one or more active coronary lesions in up to 90% of SCD victims. The active plaque state and its consequences (plaque disruption with hemorrhage into the plaque or intraluminal thrombosis) are more important than simply the degree of chronic occlusion in the pathophysiology of acute coronary syndromes, apparently including SCD. Active plaques are not restricted to the apparent culprit vessel in acute coronary syndromes, including SCD. Thus a 70% to 80% obstruction without a fresh thrombus might not be the true culprit when it coexists with lesser lesions in an active state. One precaution regarding postmortem studies is the apparent severity of stenosis in a vessel in the absence of the intravascular filling pressure present during life. Overestimation of the severity of stenosis has to be kept in mind.
Myocardial pathology reflects the presence and extent of chronic coronary atherosclerosis, because myocardial scars caused by healed myocardial infarction are common. Clinically recognized and unrecognized scars are both associated with SCD risk, and the magnitude of risk associated with each appears equivalent, based on cardiac magnetic resonance (CMR) imaging studies. This observation has implications for potential screening techniques for victims in the category of SCDs that are first clinical events. Evidence of acute myocardial infarction is less common, probably because the pathophysiologic mechanism leading to the anatomical and histopathologic expression is interrupted by the fatal arrhythmia. However, even among cardiac arrest survivors studied during the prethrombolytic or percutaneous coronary intervention era, evolution to acute transmural myocardial infarction was less common. An association between the number of involved coronary arteries and the extent of ventricular hypertrophy in SCD victims has also been recognized. A correlation between extensive coronary artery disease and left ventricular (LV) hypertrophy might be a consequence of long-standing hypertension as a risk factor in coronary heart disease patients or of post–myocardial infarction remodeling. Regardless of the mechanism, myocardial scars and LV hypertrophy are considered factors in arrhythmogenesis during transient ischemia. ,
Among the less common structural causes of SCD, pathologic anatomy reflects the underlying etiology. In DCMs, the pathologic findings are nonspecific and are characterized by interstitial fibrosis and myocyte degeneration ( Chapter 87 ). In HCMs, the anatomy depends on the specific form of the disease ( Chapter 89 ). Obstructive, nonobstructive, apical, midventricular, and concentric hypertrophy patterns are all observed. Although risk is increased in all forms of HCM, it is greater in the obstructive pattern and the least in the apical HCM subgroup. One common feature observed in HCM is myocyte disarray, which is common to most, but not all, genetic forms of the disease. The association between HCM expression and SCD risk is complex because of patterns of inheritance involving multiple gene loci and variable expression. Because of the large number of candidate genes for HCM and the high proportion of family-specific variants, the challenge of interpreting findings of previously unreported variants of uncertain significance is a particular problem in HCM.
A large autopsy study of SCD victims in Finland identified a significant subgroup with primary (isolated) myocardial fibrosis in the absence of myocardial infarction or other structural disorders. A subset of these carried genetic variants associated with inherited structural disorders such as HCM, arrhythmogenic right ventricular dysplasia/cardiomyopathy (ARVD/C), or inherited nonischemic cardiomyopathies, thus appearing to express the fibrotic components of these disorders in the absence of the classic structural diseases.
The landscape of SCD risk prediction is complex. Risk analysis should be divided into two general categories: population-based risk prediction and individual risk prediction. Conventional epidemiologic markers provide insight into probabilities for the development of coronary heart disease within a general class of subjects, but its limitations for individual risk prediction constrain the ability to profile risk and apply preventive strategies to specific individuals in the clinical setting. The inverse relationship between the incidence of SCD and absolute numbers of events in the various epidemiologic or clinical categories is important ( Fig. 79.6 ), especially when the intent is to use therapeutic interventions.
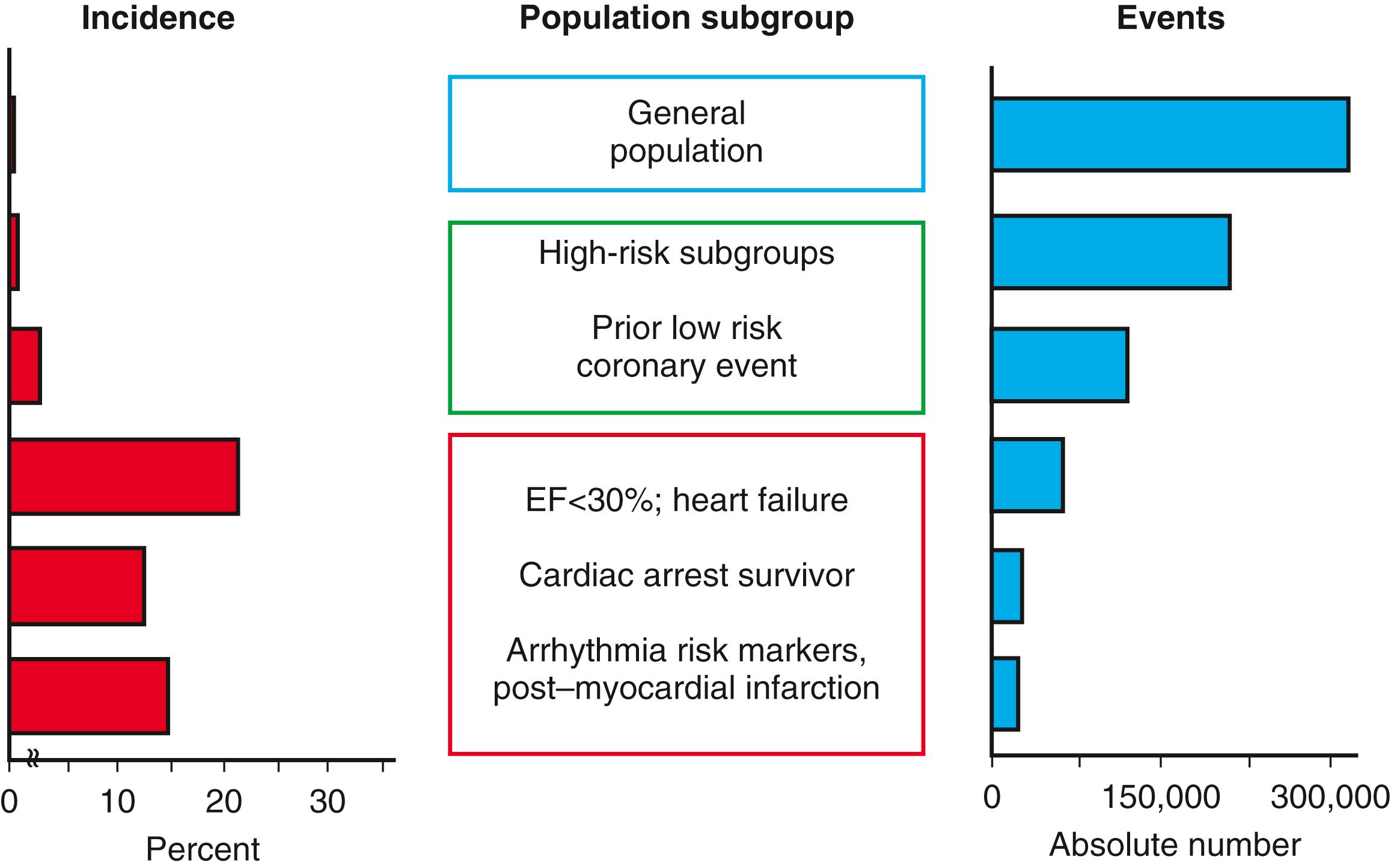
Among the general population aged 35 years and older, the estimated SCD incidence of 0.1% to 0.2% per year incorporates all out-of-hospital SCDs that occur annually in the United States. However, the low individual event rate among the general population, unselected except for age, limits the range of applicable therapeutic approaches. If patients who fall into categories of high risk for development of coronary atherosclerosis, such as those with obesity, diabetes mellitus, and hypertension, and unselected patients with established coronary heart disease are included, event rates are higher but still have limited power for specific individual risk prediction. In contrast, patients with heart failure or ejection fractions less than 35%, cardiac arrest survivors, and the specific high-risk post–myocardial infarction patients have higher event rates, but constitute decreasing absolute numbers of events and a much smaller component of the total population burden of SCD. The importance of recognizing this principle relates to the magnitude of population benefit for various preventive interventions. For example, the high-risk patient categories studied in the clinical trials of implantable defibrillators (see Fig. 79.6 ) constitute only a small part of the total universe of SCDs, and the reported benefits apply only to those small subgroups. This observation highlights the importance of identifying specific risk markers among more general segments of the population from which there is a greater potential to effect public health. Moreover, the improving outcomes in patients with acute myocardial infarction, likely attributable in large part to the benefits of early and effective interventions, appear to be decreasing the proportion of people who are more easily identified as high risk, without affecting the low-risk subgroups from which the largest number of SCD events emerge. These patterns have resulted in changes in the proportions of SCDs among the previously reported higher-risk subgroups. Specifically, the high-risk, post–myocardial infarction patient and the patient who has survived an OHCA are at relatively lower risk for cardiac arrest currently than they were in the past. In parallel with this fact are the observations that the proportion of victims in the subset with ischemic cardiomyopathy and heart failure as the pathophysiologic basis for SCD has increased (see Fig. 79.6 ). In addition, in long-term studies, an evolving pattern suggests that a prior history of heart disease is becoming less common among surviving victims of OHCA, whereas a history of risk factors is increasing.
The previous concepts can be viewed in the context of clinical patterns preceding cardiac arrest in patients with coronary heart disease. A number of studies suggest that up to 50% of all OHCAs and consequent SCDs resulting from coronary heart disease occur as the first clinical event and that up to 30% more are associated with clinical markers, suggesting a low risk for an event (see Fig. 79.5 ). A major reduction in the population burden of SCD will require the development of strategies to identify very high-risk subgroups among small clusters in the general population.
Magnitude of risk of SCD is a complex epidemiologic and clinical function, even within subgrouped categories of risk (see Fig. 79.3 ). Among the adult population, increasing age is a powerful risk predictor that becomes blunted in the presence of advanced heart disease, when it is overwhelmed by higher-risk clinical factors. The general population can be viewed as composed of a gradient of risk, depending on the number of risk factors present (see Fig. 79.4 ). However, the risk gradient based on current methods is still insufficient, and it is anticipated that pockets of increased risk density will eventually be identifiable with better profiling methods. ,
The evolution and expression of SCD resulting from coronary heart disease involve a multitiered cascade of pathophysiology operating in different time domains , (see Fig. 79.6 ). This cascade includes the elements of initiation and progression of disease in the coronary arteries, development of myocardial scarring/fibrosis, transition of vascular lesions from quiescent to active states, initiation of acute coronary syndromes, and, finally, acute arrhythmogenesis. In the early years of attention to the epidemiology of SCD, the conventional risk factors for coronary artery disease were the major focus of SCD risk prediction ( Table 79.1 ; see also Fig. 79.6 ). From a statistical and public health standpoint, this approach remains reasonable because of the large proportion and numbers of SCDs that are attributable to coronary artery disease.
| Target | Examples | Goal | Sensitivity |
|---|---|---|---|
| ASHD risk factors | Framingham risk index | Predict evolution of disease | Very low |
| Anatomic screening | Calcium scoring; CT angiography | Identify CAD | Very low |
| Clinical markers | EF; angiography; AM; EPS AM/EPS combined with EF |
Define extent of disease Identify arrhythmia markers Define high-risk subgroups |
Variable with extent of disease; low specificity Low to intermediate for screening High for specific groups Primary predictive value unknown |
| Transient risk predictors | T wave alternans; QT dispersion Pathophysiologic controls (e.g., HRV, BRS) Inflammatory markers |
Identify ECG markers of risk Quantify autonomic regulation Predict unstable plaques |
Unknown, potentially high |
| Individual risk predictors | Familial/genetic profiles | Predict specific SCD risk before disease expression | High potential for future profiling Uncertain at present; some measures useful (?) |
This concept is limited, however, by the fact that these risk factors largely predict the evolution of the substrate-based risk over time and identify orders of magnitude of risk that are too low for specific drug or device antiarrhythmic interventions. Furthermore, these risk factors do not provide a specific marker of risk for SCA and SCD. Other methods for identifying the presence of structural abnormalities in coronary arteries have been suggested as potential strategies to provide greater sensitivity and specificity (see Table 79.1 ). For example, anatomic disease screening using calcium scoring and coronary computed tomographic angiography have been suggested as methods for large-scale screening to identify abnormal coronary arteries. Although this technology identifies structural changes in coronary arteries with an acceptable degree of accuracy, its value is limited by the fact that identification of the structural abnormality does not reveal the vulnerability of plaques or specific markers of SCA risk. Repeated exposure to radiation over time is also considered a limitation of this as a screening approach.
Much of the progress that has been made to date in profiling risk of SCD has been based on clinical markers, which primarily identify the extent of disease either at a myocardial or a vascular level (see Table 79.1 ). Ischemic cardiomyopathy identifies high risk for SCD, which is particularly notable when accompanied by a history of clinical heart failure with reduced ejection fraction, and apparently also with preserved ejection fraction, especially among those with high risk markers such as type 2 diabetes. The use of LV ejection fraction as the primary indicator of risk is regarded as less specific than previously thought. Other indicators, such as myocardial scarring revealed by CMR imaging and LV volumes, are emerging as markers of potential interest.
To achieve better profiling of SCA risk, two approaches appear promising for application in future studies. One approach is prediction of transient risk, which is intended to identify patients who are at risk for the events that trigger fatal arrhythmias in a shorter time frame , , (see Table 79.1 ). Pathophysiologic elements that may contribute to transient risk include control mechanisms mediated through autonomic nervous system functions (such as heart rate variability or baroreceptor sensitivity), measures of repolarization alterations (such as T wave alternans), and inflammatory markers that are being evaluated as a predictor of risk for plaque destabilization. Whereas the inflammatory markers for plaque disruption can generally provide higher resolution of risk for acute coronary syndromes, , individual risk predictors, such as familial or genetic profiling, can potentially provide even greater resolution for SCD risk in specific persons. Because of the general principle of variable expression of many genetic risk markers, any likely future model for individual risk prediction incorporating genetic markers will have to be integrated with other methods of risk profiling, based on population or individual clinical factors. , At present, other than the general value of family history, and the specific inherited syndromes associated with SCD risk, genetic profiling has not yet yielded useful markers for individual prediction of risk of SCA/SCD.
The ability to identify the individual patient at risk for plaque disruption, in advance of an acute coronary syndrome, could provide a powerful method for identifying individuals at potential risk of SCD. In retrospective studies of men and women in whom both cholesterol levels and indices of inflammation could be correlated with risk of coronary events, each risk factor appeared to provide an independent predictive value and this combination had the strongest power of prediction of relative risk increase. However, because the outcomes were expressed as relative increases of a baseline risk among the subjects in the lowest tertiles of cholesterol and inflammatory marker concentration, the absolute contribution of inflammatory markers compared with cholesterol markers remains to be determined. A recent observation demonstrating that complex plaques are multiple suggests a generalized or systemic susceptibility to plaque disruption (rather than plaque-specific risk) and a higher recurrent event rate after myocardial infarction. This observation supports the notion of inflammation-based susceptibility. Other direct and indirect markers of the risk of plaque destabilization from inflammatory processes could also contribute to this theory of risk prediction.
SCD is more difficult to predict among patients with nonischemic cardiomyopathies, including those with familial DCMs. Although LV ejection fraction, and other parameters of depolarization and repolarization, are general risk predictors among patients who have DCM, a better association with functional capacity has been proposed. For example, among patients with DCM who are functional class I, the risk of dying is low, but the proportional probability that a death will be sudden is relatively high. As this category encompasses a large number of patients at relatively low risk, the predictive power for benefit from interventions is limited. At the other end of the spectrum, functional class III and class IV patients are at a higher risk of death generally and at a higher risk for SCD in terms of absolute numbers of deaths, although the proportional risk of SCD is lower. Moreover, among patients in this category who experience OHCA, many have nonshockable rhythms, and some shockable rhythms are secondary to the hemodynamic state and are resistant to defibrillation, possibly limiting the practical benefit of implantable cardioverter defibrillators (ICDs) in this group as well.
For this category of SCDs, which are etiologically diverse, discriminators of risk across the entire spectrum of disease expression, from early to advanced, are inconsistent. The importance of this limitation resides in the fact that the absolute number of SCDs counted among the relatively low-risk subgroups, which do not justify advanced interventions on a statistical basis, is disturbingly high. Future research must focus on discrimination of risk within the larger lower-risk population subsets, and SCDs that occur in the familial forms of DCM.
One specific etiologic category of nonischemic cardiomyopathies that is particularly challenging is acute and postmyocarditis cardiomyopathy. During the acute phase, when associated with significant impairment of LV function and classified as fulminant myocarditis, short-term risk is high, but longer-term risk ameliorates when response to therapy reverses the clinical pattern In contrast, chronic active myocarditis and persistent cardiomyopathy with scarring associates with persistent risk. However, healed myocarditis not associated with extensive LV scarring has a more benign course, even when the acute phase had been associated with life-threatening arrhythmias.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here