Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Stupor and coma refer, respectively, to moderate and severe depression of the level of consciousness. The acute onset of stupor or coma is a medical emergency. A wide variety of metabolic and structural disorders can produce this state. Management should focus on stabilizing the patient, establishing a diagnosis, and treating the underlying cause.
What are the vital signs?
Is the airway protected?
Stuporous and comatose patients are at high risk for aspiration because of impaired cough and gag reflexes, and hypoxia, which results from diminished respiratory drive. Endotracheal intubation is the most effective method for securing the airway and ensuring adequate oxygenation.
Is there any history of trauma, drug use, or toxin exposure?
Obtain a quick description of recent events and preexisting medical or neurologic conditions. Check the Emergency Medical Service run sheet.
Is someone available to provide further history?
Relatives, friends, ambulance personnel, or anyone else who has had recent contact with the patient should be identified and instructed to wait for further questioning.
Call the anesthesiology service for intubation if the patient is deeply comatose or exhibiting signs of respiratory compromise.
In stuporous or comatose patients with normal respirations, begin 100% oxygen via bag mask ventilation until hypoxemia is ruled out with pulse oximetry.
Order an intravenous line.
Order pulse oximetry.
Order a finger-stick glucose measurement.
This should always be checked immediately because hypoglycemia is a rapidly treatable cause of stupor or coma that can coexist with other diagnoses (e.g., sepsis, cardiac arrest, or trauma).
Order diagnostic blood tests.
Serum chemistries (glucose, electrolytes, blood urea nitrogen [BUN], creatinine)
Complete blood count (CBC)
Arterial blood gas
Calcium, magnesium
Prothrombin time (PT)/partial thromboplastic time (PTT)
If the etiology of stupor or coma is unclear, order toxicology screen, thyroid function tests, liver function tests, serum cortisol, and ammonia level.
Insert a Foley catheter.
Order urinalysis, electrocardiogram (ECG), and chest X-ray.
Give emergency treatment. These measures are often given in the field, or whenever the cause of stupor or coma is unclear.
Thiamine 100 mg IV
Thiamine reverses stupor or coma resulting from acute thiamine deficiency (Wernicke encephalopathy). It must be given before dextrose because hyperglycemia can lead to consumption of thiamine and acute worsening of Wernicke encephalopathy.
50% dextrose 50 mL (1 ampule) IV
Naloxone (Narcan) 0.4 to 0.8 mg IV
Naloxone reverses coma caused by opiate intoxication. Up to 10 mg may be required to reverse severe intoxication.
Flumazenil (Romazicon) 0.2 to 1.0 mg IV
Flumazenil reverses stupor or coma caused by benzodiazepine intoxication. Up to 3 mg may be required. Do not give flumazenil if seizures have occurred because flumazenil may precipitate further seizures.
What causes stupor or coma?
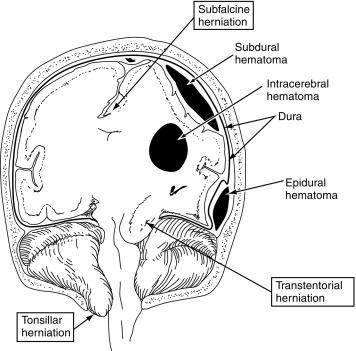
Stupor and coma result from diseases affecting either both of the cerebral hemispheres or the brain stem. As a rule, unilateral hemispheric lesions do not produce stupor or coma unless there is mass effect sufficient to raise the intracranial pressure (ICP), or compress either the contralateral hemisphere or the brain stem. Focal brain stem or bilateral thalamic lesions produce coma by disrupting the reticular activating system. Metabolic and ictal disorders impair consciousness by disrupting normal brain metabolism and electrical function. The causes of stupor and coma ( Table 5.1 ) can be broadly grouped into four categories:
Structural intracranial disorders
In most cases, these disorders are diagnosed by positive brain imaging (computed tomography [CT] or magnetic resonance imaging [MRI]) or by lumbar puncture (LP) in the case of meningitis or encephalitis.
Toxic or metabolic disorders
Abnormal blood tests usually, but not always, confirm these disorders. Drug intoxication, sepsis, renal failure, hypoxia, hypoglycemia, and multisystem systemic organ failure are common causes of toxic-metabolic encephalopathy.
Ictal or postictal states
Emergency continuous electroencephalopathy (EEG) monitoring is crucial for diagnosing active, ongoing electrographic seizure activity or epileptiform activity such as spikes or periodic epileptiform discharges (PEDs) that occur in the aftermath of seizures.
Psychogenic unresponsiveness
Technically a behavioral disorder, psychogenic unresponsiveness is a mimic of coma because normal brain function is maintained. These states are defined by their reversibility.
|
Three common and treatable causes of coma can rapidly lead to death:
Herniation and brain stem compression
Space-occupying mass lesions that produce stupor or coma are a neurosurgical emergency ( Fig. 5.1 ).
Increased ICP
Increased ICP can lead to impaired cerebral perfusion and global hypoxic-ischemic injury (see Chapter 13 ).
Meningitis or encephalitis
Death from bacterial meningitis or herpes encephalitis can be prevented with early treatment (see Chapter 22 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here