Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The editors wish to thank authors David H. Chu and Cynthia A. Loomis for their excellent contribution to this text in the fifth edition. This chapter has been reproduced here in the sixth edition essentially unchanged.
Skin is a complex organ that comprises many different cells and cell types; it forms a critical physical barrier that protects the body and maintains fluid homeostasis, temperature regulation, and sensation. Skin cells derive from both embryonic mesoderm and ectoderm, and development from these precursors is tightly regulated. Perturbations in the developmental process, either from genetic anomalies or as a result of exogenous (e.g., teratogenic) agents, can result in severe abnormalities that have important consequences in the care of infants. Understanding the normal progression of molecular and cellular events that underlie the development and differentiation of skin allows for a more rational approach to infants who have defects in these processes. For clinicians, this knowledge will direct the diagnosis, therapy, and parental counseling necessary for care of the patients.
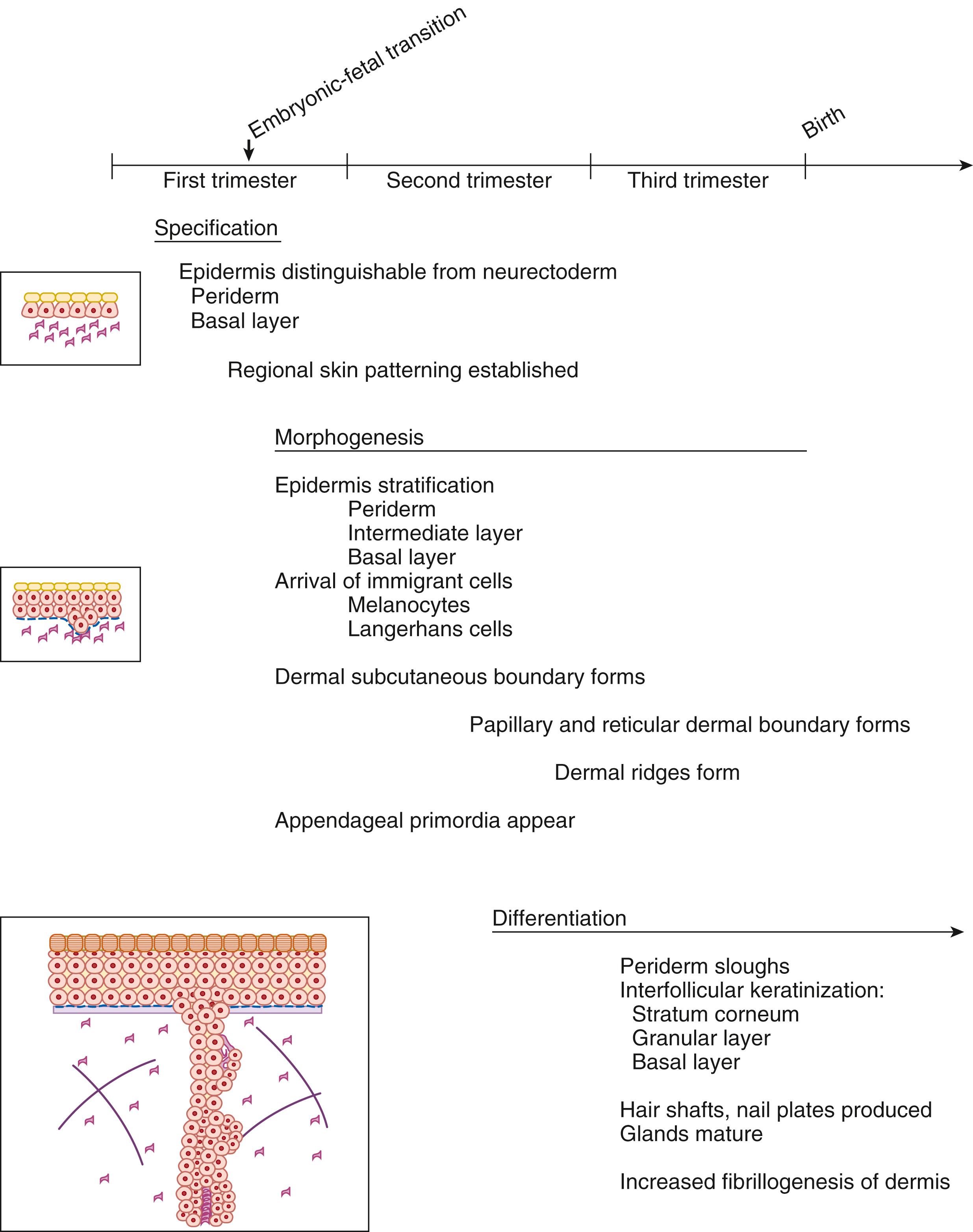
As with all organs, organogenesis of the skin proceeds through three distinct but overlapping stages, from early embryonic through fetal and neonatal development. , These stages are (1) specification, in which portions of superficial ectoderm and lateral plate mesoderm become distinct from other portions of the body wall; (2) morphogenesis, in which the specific structural and biochemical characteristics of skin begin to appear; and (3) differentiation, in which the skin tissue further develops to its mature form and postnatal stem cell niches are established.
For the sake of clarity, we have organized the discussion of the developmental progression of the skin to follow each component sequentially, first with a discussion of the epidermis, followed by the dermis and subcutaneous tissue, the dermal-epidermal junction (DEJ), and finally, epidermal appendages. Each of these sections discusses the structural and biochemical changes that occur during the particular stage of development, followed by a discussion of related clinical syndromes and genetic disorders that are related to defects in this developmental progression. However, all these tissues of the skin are, in fact, developing in parallel, and in some cases they require interaction with adjacent tissues for development. A timeline is included to illustrate the sequence of events that are occurring simultaneously ( Fig. 43.1 ).
The mature adult epidermis is a stratified squamous epithelium that develops from the ectoderm. Keratinocytes form 80% of the cellular composition. The germinative keratinocytes reside in the deepest portion of the epidermis, known as the basal layer, and these cells are known as basal cells. As differentiation of the basal cells proceeds, these cells migrate to more superficial cell layers and become progressively flattened; they also begin to express large insoluble proteins that ultimately become crosslinked along the exterior of the cell to form an insoluble shell or brick, known as the cornified cell envelope . The human epidermis self-renews every 40 to 56 days, and the constant turnover is credited to the interfollicular epidermal stem cells that reside in the basal layer. These cells are also critical for generating sufficient progeny to re-epithelialize the surface of a wound. It remains controversial as to whether most basal cells or only a select subpopulation of basal cells have stem cell self-renewal capabilities.
Above the basal cell layer rests the spinous layer, or stratum spinosum. The “spines” seen in this layer result from the abundance of desmosomes, specialized regions of the keratinocyte cell surface that promote adhesion between these cells in a calcium-dependent manner. Desmosomal proteins include plakoglobin, desmoplakins I and II, keratocalmin, desmoyokin, band 6 protein, and the cadherins—desmogleins 1 and 3 and desmocollins 1 and 2. ,
The cell layer superficial to the stratum spinosum is the stratum granulosum. , Granular cells begin to express some of the components that will contribute to the cornified cell envelope, a protein-lipid polymer that is found on the outer boundary of terminally differentiated keratinocytes. The cornified cell envelope serves a critical role in the barrier function of the epidermis. Keratohyalin granules, found within the granular cells, are principally composed of two proteins, loricrin and profilaggrin. Profilaggrin undergoes sequential proteolytic cleavage into filaggrin oligomers and finally monomers, as well as dephosphorylation, during its processing. This process is initiated at the time of formation of the granular layer and continues even after its eventual extrusion from the cornified cell. Loricrin, another major component of the cornified envelope, is also initially localized to the keratohyalin granules. Lamellar granules, which are also abundant in the granular cell layer, contain the lipid components that will be extruded from the cells and crosslinked to the cornified cell envelope. Other proteins that contribute to the cornified envelope include involucrin, small proline-rich proteins, annexin, elafin, desmoplakin, envoplakin, periplakin, repetin, and trichohyalin. Modifying enzymes such as transglutaminases are important in the final crosslinking of the cornified envelope components. Mutations in either the structural proteins or the enzymes involved in protein crosslinking and lipid and steroid metabolism can have clinically significant outcomes in genetic skin disease.
The stratum corneum contains the terminally differentiated keratinocytes, flattened dead “squames” that lack nuclei and other organelles. These cells are composed primarily of keratin filaments, tightly packed within the crosslinked cornified envelopes. Some specialized components within the epidermis maintain its architecture. Keratins are some of the most important structural proteins within the epidermal cells. They assemble as filaments composed of “basic” and “acidic” keratin peptides, which form obligate heterodimers —that is, different keratins are found to associate with a limited number of partners. , Their expression is regulated in a tissue-specific and developmentally selective manner. Mutations in these genes often exhibit clinical phenotypes that reflect the tissue expression of the specific keratin gene. For example, whereas basal cells express K5 and K14, suprabasilar keratinocytes express K1 and K10 (K1 and K9 in palmoplantar epidermis).
Other critical structural elements of the epidermis are the cell-cell and cell-matrix adhesion systems. , The major cell-cell adhesion junctions of the epidermis are desmosomes. The proteins in these complexes include specialized adhesion proteins (cadherins, calcium-dependent adhesion molecules), as well as intracellular plaque and adaptor proteins. An analogous adhesion structure, the hemidesmosome, attaches basal cells to the basement membrane at the DEJ. Although the proteins in the hemidesmosome are distinct from those of the desmosome, the plaque proteins have similar amino acid sequences, and both are tightly associated with the keratin filament network. Gap junctions form important intercellular bridges that allow small molecules to pass from one keratinocyte to another. These specialized junctions are formed by proteins known as connexins . Mutations in any of these molecules have effects on the normal formation of the epidermis that can result in certain genodermatoses, many of which have manifestations from birth.
Gastrulation of the embryo occurs during the third week after fertilization. This is a critical process that results in the generation of the three primary embryonic germ layers: endoderm, mesoderm, and ectoderm. The ectoderm then is further divided into the neuroectoderm and the presumptive epidermis. The epidermis is then subsequently specified into distinct regional domains, such as palmoplantar skin, scalp skin, and mammary skin.
The earliest presumptive epidermis consists of a basal cell layer, which covers the embryo. , By 6 weeks estimated gestational age (EGA), the surface ectoderm consists of two layers: basal cells and more superficial periderm cells. The periderm layer does not give rise to any portion of the definitive epidermis, and as such it serves as a transient embryonic covering that protects the underlying basal cells and prevents interepidermal adhesions. , This layer is ultimately sloughed during late gestation and contributes to the vernix caseosa, which covers the newborn.
The process of morphogenesis begins at approximately 8 weeks EGA, the classic transition between embryonic and fetal development, when hemopoietic production shifts to the bone marrow. At this point, the epidermis begins its process of stratification, by forming an intermediate layer between the basal cell and the periderm layers. This intermediate layer remains highly proliferative, and more layers are added as development proceeds over the next several weeks. In mice, it has been shown that this process of epidermal stratification requires the TP63 genes. In humans, partial loss of function mutations in TP63 have been seen in various ectodermal dysplasias.
Maturation of the epidermal layers includes keratinization, which results in the differentiation of granular and stratum corneal layers and the formation of a water-impermeable barrier. Accompanying this stage of development is the sloughing of the periderm. Keratinization occurs first in the skin appendages between 11 and 15 weeks EGA, followed by the interfollicular epidermis between 22 and 24 weeks EGA. , ,
The process of keratinization involves the production of certain proteins, including filaggrin and loricrin. , Posttranslational modification of the crosslinked proteins and production of specialized lipid and steroid components contribute to the water-impermeable matrix formed in the mature cornified layer. Structurally, the third-trimester stratum corneum is similar to that of an adult, but functional studies have shown that it is much less effective at preventing water loss and is more permeable than the mature epidermis. It is actually not until the third week of life that the barrier function of a newborn’s stratum corneum is comparable to that of an adult.
Human mutations that inhibit the process of specification in the epidermis have not been reported, most likely because such mutations would be incompatible with further development of the embryo. However, experiments in animals have suggested that a group of proteins—the bone morphogenetic proteins (BMPs), as well as the Engrailed-1 (En1) , Lmx1b, and Wn7a—may play an important early role in specifying distinct skin domains on the distal limb. Similarly, only a few mutations in humans have been found that affect epidermal morphogenesis. RIPK4 and IRF6, the genes defective in Bartsocas-Papas syndrome and popliteal pterygium syndrome, have been shown to be critical for early periderm formation and function, preventing inappropriate interepithelial fusions. Subsequent stratification of the definitive epidermis depends on a functional TP63 gene. ,
In contrast to the relative lack of mutations that affect epidermal specification and morphogenesis, mutations that have an important impact on epidermal differentiation are quite numerous. In general, these genes are not required for development in utero, but they become critical for effective barrier function of the epidermis after birth. Thus defects in these genes can often cause significant postnatal morbidity.
Two groups of such diseases include the palmoplantar keratodermas and ichthyoses. The palmoplantar keratodermas are a diverse group of disorders that share a common presentation of hyperkeratosis of the palms and soles. These disorders are also commonly associated with other cutaneous, as well as noncutaneous, findings. The genetic bases of many of these disorders have been discovered, and they include defects in connexins, differentiation keratins, and desmosomal components.
The ichthyoses are another diverse group of diseases that often present around the time of birth with diffuse scaly skin and defective epidermal barrier function. These conditions differ in both pattern and morphology of scaling, as well as extracutaneous features. Ichthyosis vulgaris, lamellar ichthyosis, and X-linked ichthyosis have phenotypes predominantly restricted to the skin ( Table 43.1 ). Ichthyoses can also be a cause of erythroderma (e.g., in bullous and nonbullous congenital ichthyosiform erythroderma). Neurologic abnormalities can be associated with the skin condition, as in Sjögren-Larsson syndrome, Refsum syndrome, or Tay syndrome (IBIDS: ichthyosis, brittle hair, intellectual deficit, decreased fertility, and short stature). In X-linked dominant ichthyoses, female children inheriting the relevant mutation can develop asymmetry of limbs, as in congenital hemidysplasia with ichthyosiform erythroderma and limb defects (CHILD) syndrome or chondrodysplasia punctata (Conradi-Hünermann disease). Interestingly, mutations in several genes required for barrier formation and normal epidermal desquamation also confer susceptibility to development of atopic dermatitis-like inflammatory skin diseases, including the genes encoding the cornified envelope protein filaggrin, the serine protease inhibitor SPNK1 (LEKT1), and the adhesion molecule desmoglein 1 (DSG1). ,
| Disease | Inheritance | Defective Protein(s) |
|---|---|---|
| Ichthyosis vulgaris | AD | Filaggrin |
| X-linked ichthyosis | XLR | Steroid sulfatase |
| Lamellar ichthyosis | AR | Transglutaminase 1 |
| NBCIE | AR | Transglutaminase 1; ALOX12B; ALOXE3; CGI58 |
| Bullous congenital ichthyosiform erythroderma | AD | Keratin 1; keratin 10 |
| Harlequin fetus | AR | ABCA12 |
| Sjögren-Larsson syndrome | AR | Fatty aldehyde dehydrogenase |
| Refsum syndrome | AR | Phytanoyl-CoA hydroxylase |
| Conradi-Hünermann syndrome | XLD | Emopamil binding protein |
| CHILD syndrome | XLD | NSDHL (NAD(P)H steroid dehydrogenase-like protein) |
| Netherton syndrome | AR | LEKTI (lymphoepithelial Kazal-type–related inhibitor) |
| Erythrokeratodermia variabilis | AD | Connexin 31, connexin 30.3 |
| KID syndrome | AD | Connexin 26 |
One of the earliest phenotypic presentations of a group of these disorders is known as collodion baby, in which an infant is born encased in a parchment-like membrane. Over the next few days to weeks, the membrane is shed, eventuating in lamellar ichthyosis, nonbullous congenital ichthyosiform erythroderma, Netherton syndrome, Tay syndrome (IBIDS), Conradi-Hünermann disease, and occasionally, a normal baby.
In contrast to the relatively benign outcome for collodion babies, the so-called harlequin fetus usually dies soon after birth. These babies are born encased in restrictive plates of thick, armor-like scale that have extremely poor barrier function, often resulting in fluid derangements, infections, sepsis, and death. Mutations in the gene ABCA12 , which encodes an adenosine-5′-triphosphate (ATP) binding cassette transporter, have recently been discovered to be responsible for this condition. Milder mutations with protein function cause a less severe congenital ichthyosis (lamellar ichthyosis or congenital ichthyosiform erythroderma).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here