Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
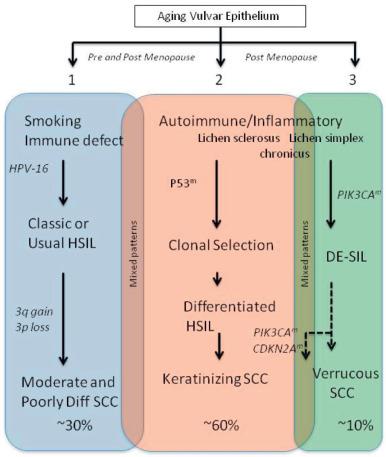
This chapter focuses on pure squamous lesions of the vulva and focuses on three general categories, including benign common human papillomavirus (HPV) associated lesions (condylomata), two accepted and one rather newly appreciated category of preinvasive squamous neoplasia, and the range of squamous carcinomas ( Figs. 6.1 and 6.2 ). This chapter emphasizes the differential diagnosis of each of these and their clinical significance and highlights those areas where the practicing pathologist may encounter difficulty.
Condylomata acuminata are extremely common, sexually transmitted, benign tumors that are most common in the early years of sexual activity. Approximately 80% are associated with HPV type 6 or (less commonly) type 11. The remaining are associated with the concomitant presence of multiple viral types, including types 6, 11, 16, and 18. The infections associated with more than one HPV type may predispose multiple and larger warts, longer disease courses, and frequent recurrences. In a recent review, the incidence was estimated at from 160 to 289 cases per 100,000 years, peaking in the third decade in both men and women.
It should be emphasized however, that the incidence has decreased in populations where young women are receiving the vaccine that covers the more common HPV types (types 6 and 11). This is also true for the risk of anal lesions in men who have sex with men.
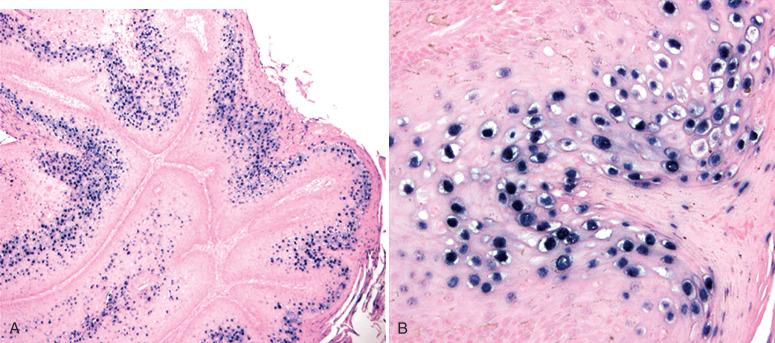
The virus life cycle is completed in the epithelium, specifically the mature superficial cells. This dependence of viral growth on squamous maturation is typical of HPV and produces a distinct cytologic change in the mature cells—koilocytotic atypia (nuclear atypia and perinuclear vacuolization)—that is considered a viral “cytopathic” effect ( Fig. 6.3 ).
Immunosuppression is an important risk factor for a range of anogenital HPV infections.
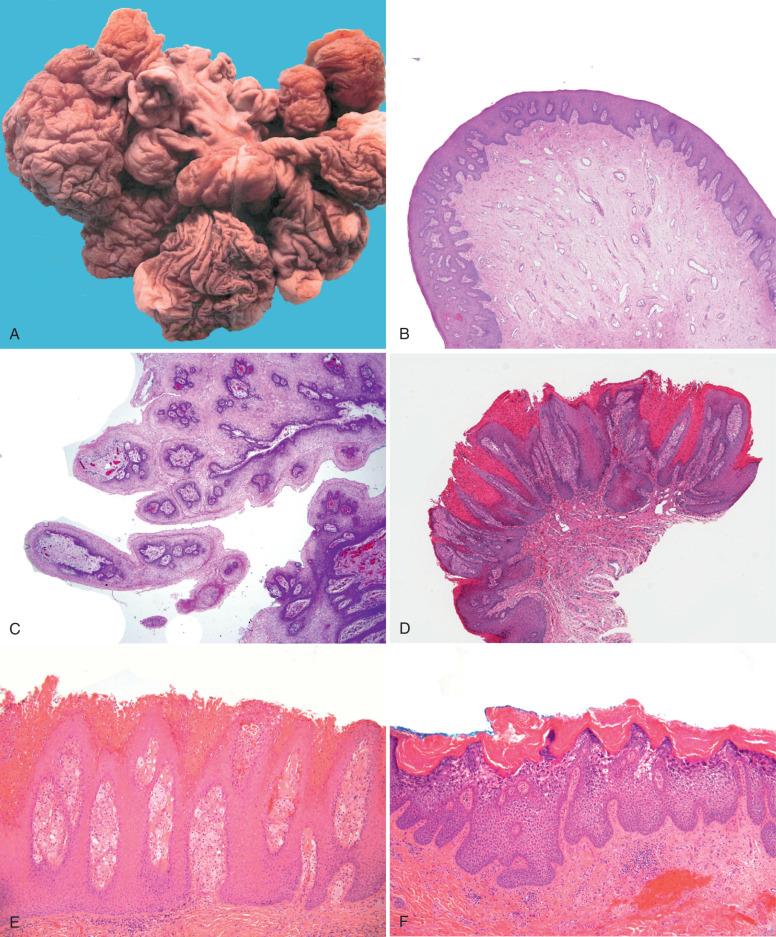
Condylomata may range in presentation from nearly invisible maculopapillary lesions in the introitus to extensive disease involving the entire vulva. They are frequently multiple and often coalesce; they involve perineal, vulvar, and perianal regions, as well as the vagina and, less commonly, the cervix ( Fig. 6.4 ), where detection by cytology is variable.

Several questions come to mind before scrutinizing a possible condyloma.
What is the age of the patient? These lesions are typically seen in young women, although they are not uncommon in the older age group. However, in the latter case, potential precursors must be excluded. This is discussed later. As is discussed subsequently, the diagnosis of condyloma based on acanthosis, papillomatosis, and hyperkeratosis should be made with care if the following are also observed: (1) more pronounced nuclear atypia, (2) abnormalities in squamous differentiation, and (3) a clinical history of vulvar inflammatory dermatoses. Concerning the latter, particular care must be taken in older women with limited samples, in which case a more significant vulvar lesion must be excluded. Contrariwise, the diagnosis must be made carefully in very young patients, keeping in mind the potential implications for inappropriate sexual contact.
Is there a greater risk of multiple lesions or higher-grade vulvar precursors? As mentioned earlier, this comes up particularly if the patient is immunosuppressed, in which case a careful survey of the entire lesion is particularly important.
Condylomata may present in several forms, several of which may coexist in the same lesion and all of which are associated with HPV types 6/11.
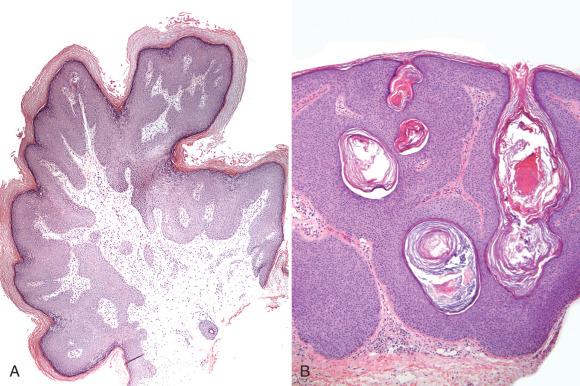
The “ classic type, ” consists of a branching, treelike proliferation of stratified squamous epithelium supported by a fibrous stroma ( Fig. 6.5 ). Acanthosis, parakeratosis, hyperkeratosis, and, most specifically, nuclear atypia in the surface cells with perinuclear vacuolization (koilocytosis) are present. The degree of cytopathic change can vary considerably, and many lesions occurring in skin do not have prominent koilocytosis. The typical finding is that of a few keratinocytes in the granular layer showing modest nuclear enlargement and variable halo development (see Fig. 6.5 ). The most important accompanying findings are discrete acanthosis and papillomatosis.
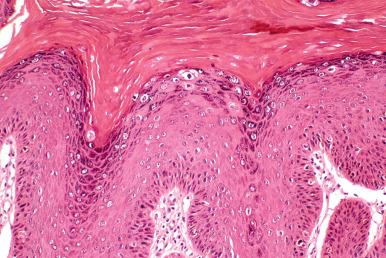
Some low risk HPV infections may exhibit no obvious cytopathic changes. Such lesions may call to mind the diagnosis of “ fibroepithelial papilloma ” ( Fig. 6.6A ). Nevertheless, the presence of acanthosis and papillomatosis supports the diagnosis of condyloma by virtue of the strong association with HPV.
Giant or extensive condylomas are uncommon and as defined here would consist of very large lesions that have the following features: (1) evidence of cytopathic effect and (2) verifiable low risk HPV, although the latter need not be proven as long as a non-HPV-related differentiated exophytic vulvar intraepithelial lesion (DE-VIL) is excluded. One caveat is the rare example of a malignancy arising in a low-risk HPV infection, which we have rarely seen.
Large condylomata are by definition difficult to remove in their entirety. Their distinction from other verruciform lesions, including verrucous carcinoma, is discussed later in the section on differentiated exophytic lesions.
Seborrheic keratosis like condyloma displays a prominent homogeneous population of basaloid cells, horn cysts (see Fig. 6.6B ). This subset differs from cutaneous seborrheic keratosis by the strong association with HPV-6 nucleic acids based on earlier studies. In the study by Bai et al., 72% of vulvar seborrheic keratosis lesions were HPV positive. In contrast, a recent study using a series of vulvar seborrheic keratosis cases of similar size (28 cases) found only 14% of HPV positivity. Thus, it should be emphasized that (1) this association may be strongest in young women, and (2) it might be argued that strict application of criteria for the diagnosis of seborrheic keratosis may lower the frequency of HPV-6 positivity. Suffice to say that (1) many HPV-6 positive vulvar lesions resemble seborrheic keratosis and (2) most classic-appearing seborrheic keratosis in post-menopausal women are HPV negative. This underscores the importance of clarifying the HPV association in the older group to avoid inappropriately labeling the lesion as a sexually transmitted disease (STD).
Flat condyloma is a distinct subset of low-grade squamous intraepithelial lesion (LSIL) of the vulva and includes discrete foci of mild acanthosis with cytologic changes ranging from koilocytosis to minimal nuclear atypia ( Fig. 6.7 ). The designations flat condyloma and HPV effect were recently substituted by LSIL of the vulva or vulvar LSIL in the 2015 ISSVD Terminology of Vulvar SIL. According to this terminology and to the 2014 World Health Organization (WHO) classification, the three exophytic lesions such as condyloma acuminatum, fibroepithelial papilloma, and seborrheic keratosis would be and classified as benign squamous lesions. Flat condylomas (VIN I) are less obvious clinically, and being flat they are usually associated with viruses other than HPV 6 and 11; up to 84% have been associated with high-risk HPVs. Nevertheless, the risk of a malignant outcome seems no higher than that for other low-grade lesions of the vulva.
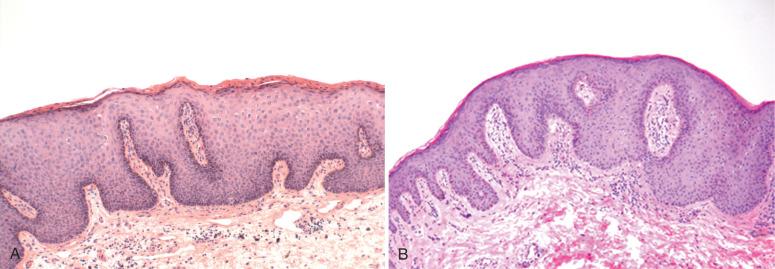
Pseudo-Bowenoid papulosis is another unusual variant of condyloma that is characterized by a striking increase in apoptosis in the upper epithelial layers, resulting in multiple cells in various stages of degeneration, beginning with chromatin dispersal (pseudomitoses) and ending with small condensed eosinophilic bodies derived from shrunken cytoplasm. This variant closely resembles oral epithelial hyperplasia of Hecht ( Fig. 6.8 ). This variant is not associated with the common genital HPV types in our experience and was associated with HPV types 13 and 32 in one report.
Condylomas resembling cutaneous warts are occasionally encountered, raising the question of a cutaneous papillomavirus infection. Although the majority of these lesions contain genital HPV types, cutaneous HPVs may be present. This is addressed later in this chapter in the Pediatric Complications of HPV Infection section.
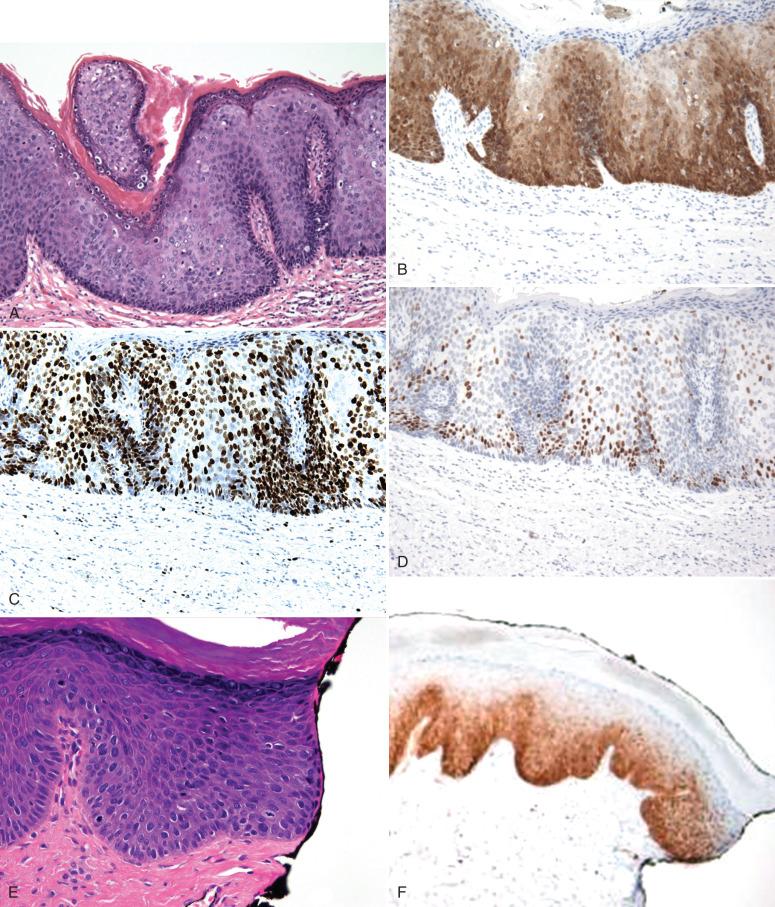
P16ink4: Because they contain low-risk HPV types such as HPV-6 and HPV-11, exophytic condylomata and their variants typically stain weak or patchy for p16ink4, a property that easily distinguishs them from higher-grade vulvar intraepithelial neoplasia (VIN) ( Fig. 6.9A and B ). We occasionally use this immunostain to aid in classifying lesions that resemble condylomata but contain more atypia than expected.
Ki-67: Immunostains for Ki-67 antigen (Mib-1) will also show increased proliferative activity in the middle and upper epithelial layers (see Fig. 6.9C ) of condylomata, a staining pattern not seen in normal mature squamous epithelium (see Chapter 13 ). Studies have established increased proliferative activity in the upper layers and have proposed the use of Ki-67 (MIB-1) as a marker to distinguish non-HPV from HPV-related lesions. We do not employ this stain in routine practice given the fact that most condylomas are easily recognized.
HPV testing: Other options include HPV in situ hybridization or polymerase chain reaction (PCR) amplification of extracted DNA. However, it should be emphasized that with the exception of the pediatric population, the demonstration of HPV serves relatively little purpose from the standpoint of management. For this reason, although special stains or HPV testing occasionally have been helpful in clarifying the origins of mild atypias of the vulva, we do not consider them an appropriate use of resources in most cases and do not routinely employ them in practice.
The differential diagnosis of condyloma includes a range of verruciform lesions, which is discussed in greater detail later and summarized in Table 6.1 .
Fibroepithelial stromal polyp (FSP): These polypoid lesions of the vulva can be single, multiple, or extensive ( Fig. 6.10A ). They exhibit minimal acanthosis and stromal atypia and usually score negative for HPV (see Fig. 6.10B ). Occasional lesions are HPV positive, but we do not test them for HPV or perform special stains.
Introital papilloma: This entity consists of small villiform polypoid excrescences at the introitus, likely remnants of hymenal ring. Lesions like this have been mistakenly classified as condylomata. However, they contain no cytopathic effect (see Fig. 6.10C ). Ultimately, with the exception of children (for whom the question of sexual abuse or exposure must be excluded) and the potential stigma of being diagnosed with a STD, the practical distinction of a low-risk HPV infection from a noninfectious polyp is not critical. One exception is the distinction of introital condylomata from hymenal ring , particularly if a misdiagnosis precipitates treatment that is painful and unnecessary. For this reason, the management of introital condylomas in young women—most of which will regress spontaneously—should be conducted with care.
Verruciform xanthoma (see Fig. 6.10D and E ): This is a discrete verruciform keratosis with dyskeratosis and foamy histiocytes in the polyp stroma. The latter may be inconspicuous. These lesions are more commonly seen in the oral cavity, and their pathogenesis in the vulva is not clear. An inflammatory origin has been proposed by some and one study found an association with inflammatory dermatoses.
Epidermolytic hyperkeratoses (see Fig. 6.10F ): This entity comprises less than 1% of lesions found on vulvar biopsy. It is occasionally found in biopsies being taken for other conditions (such as, VIN) and carries no known significance. Acantholytic dyskeratosis or papular acantholytic dyskeratosis (PAD) has been seen previously as sporadic papules or plaques on the labia majora and adjacent skin of the vulva, until concomitant lesions in other locations were reported and one familial case was described. Its main histological features include acantholysis with variable degrees of dyskeratosis. PAD is probably a specific entity that shares overlapping features with Darier disease and Hailey-Hailey disease, and could be caused by ATP2C1 gene mutations.
Polynucleated atypias: Another mimic is pronounced polynucleated atypias associated with nonspecific vulvar inflammatory changes (discussed later). These conditions are characterized by multiple (2 to 15), normal-sized nuclei associated with mild acanthosis. The atypia may be seen in both the lower and upper epithelial layers and must be distinguished from both condyloma and VIN. The presence of multiple nuclei, their similarity in appearance to the nuclei in adjacent cells, and the absence of hyperchromasia and nuclear enlargement support this benign variant, which is analogous to nonspecific cutaneous inflammatory changes.
| Diagnosis | Figure | Atypia | Comment |
|---|---|---|---|
| Condyloma | 6.5, 6.6 | Variable koilocytosis | No atypia in lower two-thirds of the epithelium, discrete, normal keratinocyte maturation. |
| Fibroepithelial papilloma | 6.6 | Mild surface karyomegaly | Similar to condyloma but lacks koilocytosis. |
| Seborrheic keratosis | 6.6 | None | Resembles cutaneous seborrheic keratosis, may have rare koilocytosis. May be pigmented. |
| Pseudo-Bowenoid papulosis | 6.8 | None | Prominent apoptosis with “pseudomitoses.” Lower epithelial layers are bland appearing. |
| Fibroepithelial stromal polyp (FSP); introital filiform polyps | 6.9 | None, except stromal cell atypia | Minimal acanthosis. |
| Verruciform lichen simplex chronicus (LSC) | 6.22 | None | Preservation of keratohyalin granules. |
| Differentiated exophytic vulvar intraepithelial lesion (DE-VIL) | 6.23 through 6.25 | None or mild keratinocyte maturation | Surface pallor, parakeratosis. |
| Verrucous carcinoma | 6.29 | 0-1+ | Minimal surface or interface atypia; uniform invasion. |
| Giant condyloma | 6.36 | Variable surface atypia | Difficult diagnosis at times; might closely resemble verrucous carcinoma. |
| Verruciform squamous cell carcinoma | 6.28 | 1-2+ surface and interface | Atypia may be minimal in some cases but irregular invasive growth should be present. |
| Keratoacanthoma (KA) | 6.37 | 1+ | Slight interface atypia, pseudoepitheliomatous appearance. |
| Verruciform classic/usual vulvar intraepithelial neoplasia (VIN) | 6.11 | 3+ | High-grade nuclear changes with variable verruciform growth. |
| Papillary squamous carcinoma | 6.29 | 3+ | Uniformly demarcated but disordered epithelial growth (intraepithelial carcinoma). |
In the previous edition of this book, we diagnosed these low-risk proliferations as LSILs. The current terminology from the Lower Anogenital Squamous Terminology (LAST) project is in line with this. Terms include:
Low-grade squamous intraepithelial lesion (exophytic condyloma)
Condyloma acuminatum
Low-grade squamous intraepithelial lesion (flat condyloma/VIN I).
Condylomata typically present within 6 weeks of infection and usually regress over the ensuing months. In a minority of cases, the lesions persist. For this reason, immediate treatment may or may not be successful and should be conservative. Small condylomata in teenagers may be best managed by addressing coexisting infections (Candida), with follow-up in 3 to 6 months. Care should be taken in treating small introital lesions, particularly with attention to avoiding treatments (e.g., 5-fluorouracil [5-FU]) that could produce long-standing irritation and dyspareunia. Larger lesions may be treated by topical agents (Aldara [imiquimod]) or cryotherapy and, if extensive, carbon dioxide laser.
With the recent introduction of vaccines targeting HPVs 6 and 11, the incidence of genital warts has been closely monitored in populations of young men and women. A recent meta-analysis of several studies noted a 61% reduction in genital warts in the 13 to 19 age group following vaccination targeting HPVs 6 and 11.
Genital warts can occur at any point in infancy and childhood. The potential mechanisms of transmission include vertical (during birth), casual contact, and sexual abuse. Spontaneous regression occurs in approximately half. Although the principal concern imposed by genital wart virus infection in the pediatric population is sexual abuse, HPV infection does not correlate closely with abuse. Moscicki et al. reported that HPV types 16/18 were more commonly seen in infections that were presumed vertical (neonates and infants), whereas genital warts later in childhood were due to HPV types 6/11. Even in the latter case, modes of transmission other than sexual abuse have been proposed.
The three important messages regarding pediatric genital warts are as follows:
Sexual abuse must be excluded by appropriate means. Although the detection of HPV has been reported in the absence of abuse, abused children clearly have a higher frequency of HPV infection than controls. Studies have documented that although the frequency of HPV infection in abused children between 4 and 12 years old (those without obvious warts) is low (10% to 16%), it is significantly higher than in nonabused individuals. A multicenter study conducted in the United States, including 576 children between 6 months to 13 years old, detected HPV by PCR and hybridization in 13.7% of the abused participants and in 1.3% of the participants without evidence of child abuse, respectively ( p < 0.0001). The number of HPV-infected children increased with certainty of abuse (8.4%, 15.6%, and 14.5% in participants with possible, probable, and definite sexual abuse; p < 0.0001) and with age (20.6% in participants 10 years old or older). These HPV infection frequencies are similar to those seen in populations of young sexually active women. Child sexual abuse, presence of anogenital warts, and age were independently associated with HPV detection by logistic regression analysis. When participants with genital warts where excluded from the analysis, abuse and age persisted independently and were significantly associated with HPV. A study conducted in Norway including 211 children ages 5 to 6 years old, selected exclusively for nonabuse, detected HPV by PCR and sequencing in 3% of the cases (all girls), 1.8% with clinically detectable anogenital warts. Thus despite the association between abuse and HPV detection, screening of children for abuse based on testing alone is not recommended. Importantly however, another study showed that most HPV-positive abused children between 5 and 12 did not manifest with genital warts.
A proportion of genital infections have been associated with HPV-2 (≈15%), with the majority (75%) belonging to the common genital types 6 and 11 ( Table 6.2 ). In the multicenter study described earlier, the HPV types most frequently detected were 16, 6, and 84 (low-risk). From the tested children, 52.4% had high-risk or high-plus low-risk genital HPV types, 41.0% had low-risk genital HPV types, 0.6% had cutaneous HPV types (epidermodysplasia verruciformis), and 0.2% had oral HPV types.
| Lesion | n | LR:HR Human Papillomavirus |
|---|---|---|
| Vulvar condyloma | 34 | 97 : 3 |
| VIN 1 | 11 | 70 : 30 |
| VAIN 1 | 19 | 16 : 84 |
| VIN 3 | 6 | 0 : 100 |
Stevens-Simon et al. proposed the following criteria for sexual abuse:
The child discloses that abuse has occurred under appropriate interview.
A physical examination discloses genital trauma characteristic of abuse.
Other STDs are present.
A perpetrator admits to abuse.
A credible witness observed abuse to occur.
A forensic examination reveals semen, sperm, or acid phosphatase from genital fluids.
A review by Bussen et al. about the correlation between anogenital warts and child abuse, including the assessment of the statements by national and international professional associations, concluded: (1) diagnosis of anogenital warts should be made by clinical examination; (2) HPV typing or serological examination is not recommended; (3) histological investigation is only indicated if the clinical diagnosis is uncertain, treatment resistance or early recurrence are present, or malignancy is suspected.
In the great majority of cases, confirming abuse is exasperatingly difficult. In a study of 131 children with anogenital warts, a history of HPV infection was documented in 50% of the mothers and siblings. Only three were suspected of abuse, and none were proven.
In summary, a careful history and examination are warranted when children present with genital warts. However, sexual abuse will not always be confirmed, and HPV testing alone is unlikely to resolve this question. Future studies of the means of HPV transmission and the development and repercussions of the infection during infancy and childhood are expected to evaluate possible changes during the vaccination era.
Recurrent respiratory papillomatosis (RRP; laryngeal papillomas) is an uncommon chronic papillomavirus infection in children, associated with HPV type 6 or 11 and affecting between three and four offspring per 100,000 births. RRP has been estimated at three per million person years in children, making it a uniquely rare complication of HPV infection. It is the most common laryngeal infection in children, associated with voice changes, hoarseness, choking, and failure to thrive. A recent European multicenter study highlighted the occurrence of RRP in adults, also verifying three peaks in its distribution of age of onset, with median ages of 7, 35 (most patients), and 64 years. Measso do Bonfim et al. identified the differences among the cellular transcription factors of juvenile and adult-onset RRP caused by HPV-6 molecular variants, respectively, HPV-6vc and HPV-6a. In approximately 30% of cases, papillomas extend beyond the larynx, and the risk of malignant transformation is estimated at 5%. Karatayli-Ozgursoy et al. showed that the age of disease onset is the strongest predictor of transformation and that dysplasia or carcinoma associated to RRP is most commonly seen in adults. Deaths are rare, but the disease is chronic, often necessitating numerous procedures to maintain the airway, including tracheotomy in as many as 14% of cases with juvenile onset. The later the diagnosis, the more procedures are needed to control the disease. The risk factors vary among studies. Shah et al. noted a strong relationship between juvenile papillomatosis and a lower incidence of cesarean births (4.6-fold less), first-order births (1.6-fold higher), and younger (<20 years) maternal age (2.6-fold greater). The impression from these statistics is that laryngeal papillomas are transmitted at birth via contact with an infected genital canal, particularly in younger mothers. The latter suggests a shorter interval between exposure to HPV and birth, implying insufficient time to generate protective antibodies. In a recent study from Denmark, Silverberg et al. observed a strong association between laryngeal papillomas and maternal genital warts during pregnancy, with a risk of 7 per 1000 live births. The authors estimated that the relative risk imposed by concurrent genital warts in the mother was 231-fold. Additional risk factors included a non-cohabiting father and longer delivery time (>10 h). The former was considered to increase the risk of additional exposures during pregnancy and the latter to increase contact between mother and fetus during labor. Despite the latter, cesarean section offered minimal protection (RR = 0.86). However, it is conceivable that infection can occur in the interval from membrane rupture and surgery. Whether the virus can ascend through intact membranes to infect the fetus is controversial.
A systematic literature review identified maternal genital condylomas during pregnancy and delivery as the major risk factor for the acquisition of juvenile RRP. HPV-11 genotype and early age of onset were identified as important determinants of disease severity. Genetic and immunological profiles influenced both acquisition and clinical course. The authors concluded that once most of these factors are not readily modifiable, prevention of condylomas in women of childbearing age is the key to reduce the impact of this disease.
Therapeutic options for RRP have expanded to include antivirals and antivascular endothelial growth factor antibodies. Other options include the use of the vaccines targeting both HPV-6 and 11, which in some (but not all) studies have been associated with a reduction in the severity of the disease and increased symptom-free intervals. This is to be distinguished from the potential beneficial effect of prophylactic vaccination to reduce the risk of acquiring this disease via the mother.
As far back as in the 1960s, authors noted the presence of at least two different forms of preinvasive vulvar neoplasia. Kaufmann and Gardner grouped precancers into three categories, corresponding to erythroplasia of Queyrat, Bowenoid carcinoma in situ, and carcinoma simplex. The first two fall into the group associated with high-risk HPVs, combine abnormal maturation with conspicuous atypias, bear close similarity to their counterparts in the cervix, and are simply termed high-grade squamous intraepithelial lesion (HSIL) of the vulvar (VIN II to VIN III). In contrast, carcinoma in situ simplex, which is now termed differentiated VIN (or differentiated HSIL), exhibits less striking atypia that is predominately basal, display altered keratinocyte differentiation, and are HPV negative.
This is the most common form of vulvar cancer precursor and as defined implies an infection by high-risk HPV. Excepting exophytic condylomata, which are usually separated from this group types, most are associated with high-risk HPVs. Other HPV types include types 31 and 33. HPV-18 is rarely found in HSIL. VIN I is analogous to a “flat” condyloma and falls under the category of LSIL described in the prior section; VIN II and VIN III equate to HSIL and are strongly associated with HPV-16, which is isolated from nearly 70% of cases. In an effort to standardize the histopathologic terminology for HPV-associated squamous intraepithelial lesions across all lower anogenital tract sites, the term high-grade squamous intraepithelial lesion (HSIL) was proposed to be used in vulva lesions by the Lower Anogenital Squamous Terminology (LAST) in 2012. Later, HSIL was included with LSIL and differentiated-type VIN in the WHO classification under the term squamous intraepithelial lesions.
Important attributes of HSIL:
HSILs of the vulva typically occur in slightly older women than in the cervix, with a mean age in the mid- to late 30s, rather than 10 years earlier. In recent years, the mean age of women with classic HSIL of the vulva has decreased from older than 50 years to younger than age 40 years.
A strong correlation with smoking, both for classic HSIL and HPV-positive vulvar carcinomas, has been reported.
Immunosuppressed patients are also at risk and may exhibit a range of HPV-related lesions affecting younger women.
Importantly, the frequency of VIN in older women appears to have remained relatively constant, suggesting that in the older age group, factors other than HPV exposure may be involved.
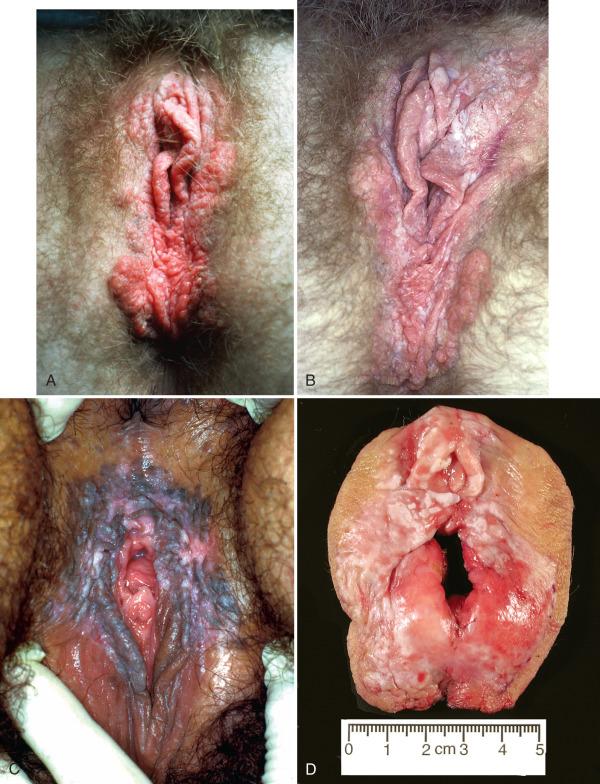
Classic vulvar HSILs are more likely to present as discrete abnormalities in the vulvar squamous mucosa. They can appear as small pigmented or hyperkeratotic maculopapular, plaque-like lesions, or more extensive, confluent lesions ( Fig. 6.11 ). They may closely resemble condylomata, although they tend to be less discrete and more irregular in distribution. They may coexist with condylomata, a feature more commonly seen in (but not limited to) immunosuppressed individuals.
Proper gross exam of VIN requires the following:
The lesion should be carefully inspected and any satellite lesions noted.
Margins should be inked such that lateral and medial orientation is preserved.
The lesion should be photographed once pinned out.
Care should be taken to avoid driving pins through lesional tissue.
Section location should be labeled on the photograph and the specimen left as intact as possible to facilitate reevaluation.
When preparing to examine a vulvectomy specimen, the pathologist should pay particular attention to the following:
Specimen orientation: HSILs typically have a “pushing” appearance, with larger bulbous projections that might appear to infiltrate the stroma.
Margins: These should be well marked to ascertain involvement. In our experience, margins are often involved, which may speak to the difficulties in mapping the lesion with the naked eye.
The diagnosis of classic vulvar HSIL is based on the following:
High-risk HPV infections of lower genital tract squamous epithelium presumably initiate with entry into the basal cells by breaks in the keratinized epithelium. Expression of viral oncogenes leads to altered cell growth and differentiation in the replicating cells that will be carried upward into the upper layers such that all layers of the epithelium will display both atypia and increased proliferative activity.
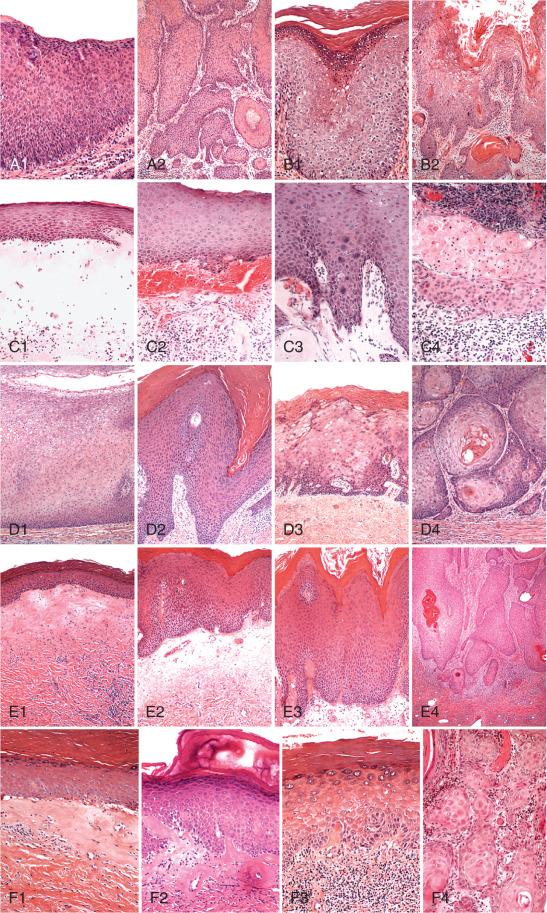
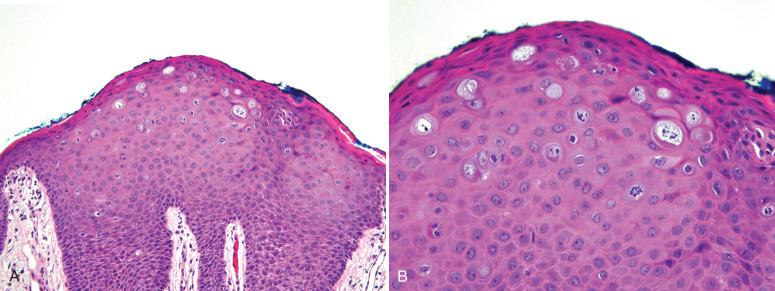
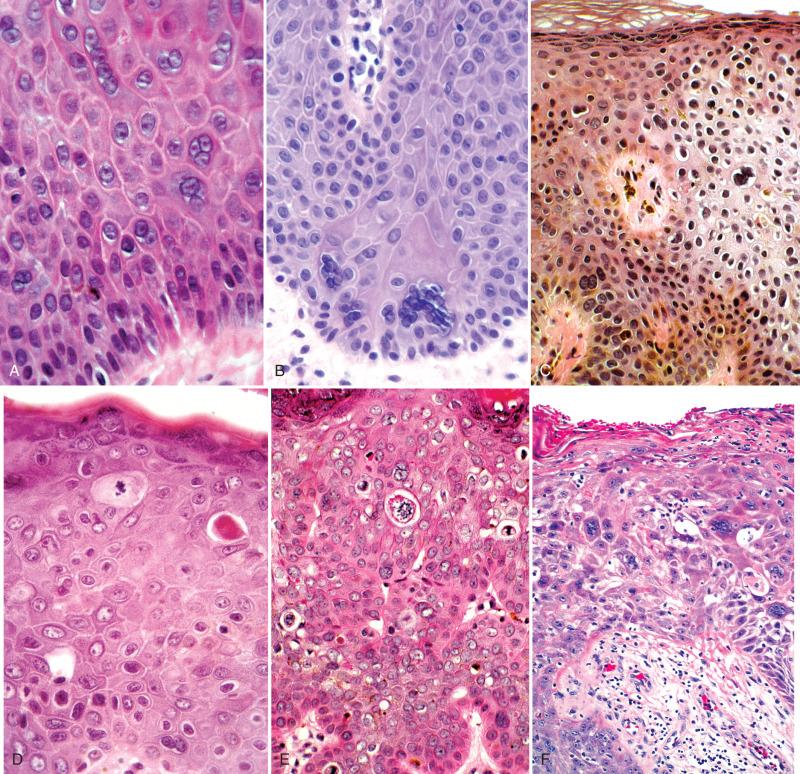
With occasional exceptions, atypia should be present in at least the lower and middle thirds of the epithelium ( Fig. 6.12A-C ). The degree of atypia may vary in the most mature third. Characteristic morphologic findings include nuclear enlargement, hyperchromasia, and multi-nucleation in the lower epithelial layers, often with abnormal mitoses (see Fig. 6.12B ). Apoptotic cells (resembling corps ronds) are frequently present (see Fig. 6.12C ). The surface often contains atypical parakeratosis with or without koilocytotic atypia (see Fig. 6.12D ).
![Fig. 6.12, Microscopic features of classic vulvar intraepithelial neoplasia (VIN) (high-grade squamous intraepithelial lesion [HSIL]). A, Junction of non-neoplastic (left) and neoplastic (right) epithelium. There is full-thickness atypia with minimal maturation, characteristic of carcinoma in situ (VIN III). B, The basal third exhibits marked nuclear atypias with anisokaryosis, pleomorphism, and variable nuclear staining. Note the abnormal mitosis (arrow). C, A higher magnification showing apoptosis. D, Dense parakeratosis on the surface of a classic VIN. E, A condylomatous HSIL. F, Skin appendage involvement by classic VIN. Fig. 6.12, Microscopic features of classic vulvar intraepithelial neoplasia (VIN) (high-grade squamous intraepithelial lesion [HSIL]). A, Junction of non-neoplastic (left) and neoplastic (right) epithelium. There is full-thickness atypia with minimal maturation, characteristic of carcinoma in situ (VIN III). B, The basal third exhibits marked nuclear atypias with anisokaryosis, pleomorphism, and variable nuclear staining. Note the abnormal mitosis (arrow). C, A higher magnification showing apoptosis. D, Dense parakeratosis on the surface of a classic VIN. E, A condylomatous HSIL. F, Skin appendage involvement by classic VIN.](https://storage.googleapis.com/dl.dentistrykey.com/clinical/SquamousNeoplasiaoftheVulva/11_3s20B9780323447324000066.jpg)
A basaloid pattern usually predominates, but a range of differentiation, including koilocytosis or warty features, can also be encountered (see Fig. 6.12E ).
Skin appendage involvement is common in classic HSIL and is analogous to crypt involvement in the cervix (see Fig. 6.12F ). The significance of this phenomenon is twofold: (1) It may be confused with superficial invasion if tangentially sectioned. (2) It may influence the therapeutic success of treatment methods that target removal of the superficial mucosa, such as laser and topical application of 5-FU (Efudex). However, the latter are employed less commonly now and appendage involvement is not a factor in choice of therapy for classic VIN.
It is important to emphasize that although most high-grade VIN lesions are easily identified, some lesions may cause some diagnostic confusion and include the following:
Lesions corresponding to what was previously termed Bowenoid dysplasia ( Fig. 6.13 ). These are characterized by milder atypia throughout the epithelium, and we typically classify them as HSIL (VIN II).
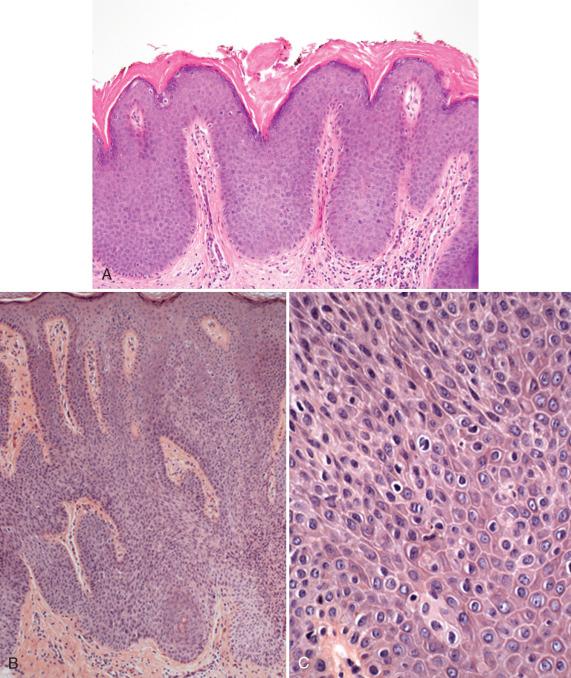
Some variants may display minimal surface atypias with keratohyaline granules, particularly when there are superimposed lichen simplex chronicus (LSC) changes ( Fig. 6.14 ). The degree of atypia may be far less striking than normally seen in HSIL. Special stains for p16 typically highlight the lower third of the epithelium.
Uncommon variants of classic VIN in which less well-differentiated squamous cells invade the mature squamous epithelium, so-called pagetoid VIN ( Fig. 6.15A ). The neoplastic cells form a discrete nesting pattern interposed with normal keratinocytes.

Even rarer variants demonstrate columnar cell differentiation, which must be distinguished from Paget disease or extension from urothelial carcinomas (see the next section) (see Fig. 6.15B ).
A rarely encountered variant identical to cutaneous lesions seen in epidermodysplasia verruciformis (EV) is associated with immune suppression. These lesions are likely associated with EV-associated HPVs (such as, HPVs 5 and 8) and display clusters of large keratinocytes with one or more nucleoli in the mid- to superficial epithelial layers with blue-gray cytoplasm. The distribution is reminiscent of pagetoid VIN given the juxtaposed normal appearing epithelial cell (see Fig. 6.15A ). We have seen two cases in our practice; neither was associated with an invasive neoplasm.
The following pertain to immunostaining classic HSILs of the vulva.
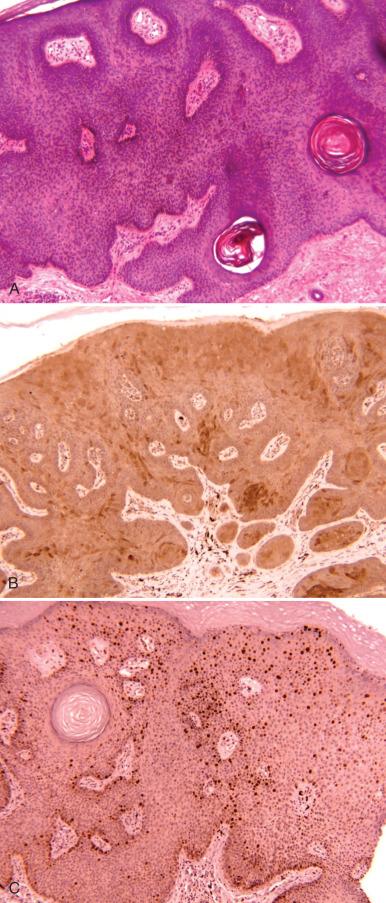
Studies have shown strong nuclear and cytoplasmic staining for p16 and diffuse staining for Ki-67, similar to cervical intraepithelial neoplasia. Fig. 6.16 shows a classic example of diffuse staining in a vulvar HSIL, which in combination with the cytologic atypias confirms the diagnosis of HSIL (see Fig. 6.16A and B ). However, the reader is reminded that strong but focal staining can be seen at the interface cells in the setting of reactive/reparative change (see Fig. 6.16C ).
Most but not all p16-positive vulvar HSILs score positive for high risk HPVs. This leaves open the question of whether a subset of HPV+/p16− HSILs exist.
We have seen some HSILs stain strongly for p16, but the distribution is exclusively cytoplasmic. The significance of this is unclear.
Mib-1 staining is generally higher than in condylomata; it is not generally used in practice (see Fig. 6.16D ).
In contrast to differentiated VIN (HSIL), which is discussed later in the chapter, p53 immunostains show patchy nuclear localization.
Although not necessary in most cases, a p16 stain might be helpful in ambiguous lesions and in occasional instances can be helpful in highlighting margins when the pathologist is uncertain (see Fig. 6.16E and F ).
Because many flat condylomas can also score positive because of their association with other high-risk HPVs, the reader is cautioned to avoid relying too much on the p16 staining pattern alone when assigning lesion grade.
The differential diagnosis of classic VIN includes the following:
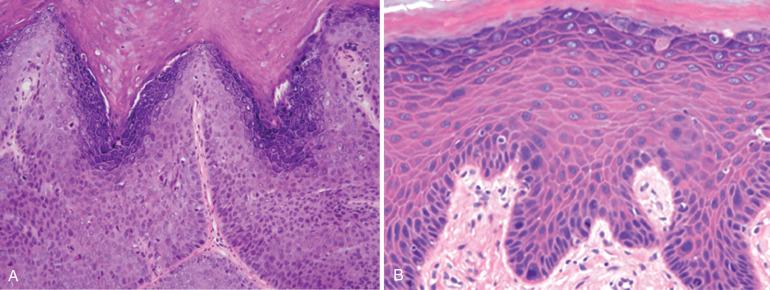
Multinucleated atypias involving the lower epithelial layers may mimic VIN ( Fig. 6.17A and B ); however, the lack of atypia in the multinucleated cells and adjacent epithelium distinguishes this from VIN (see Fig. 6.17C ).
Condylomata with apoptosis (pseudo-Bowenoid papulosis; see Fig. 6.17D and E ) may mimic VIN (see Fig. 6.17E ) by the presence of pseudomitoses and apoptosis. However, the lower epithelial layers are bland in appearance.
Seborrheic keratosis-like condylomata are composed of immature squamous cells but lack atypia and are usually easily distinguished from VIN. In rare instances, other neoplasms may mimic VIN.
Rare reports have described vulvar mucosal involvement by urothelial neoplasia, which may be confused with either VIN or Paget disease (see Chapter 7 ).
Rarely, herpes zoster-like lesions may mimic VIN, particularly when multinucleated cells are prominent, but inclusions are not conspicuous (see Fig. 6.17F ).
High-grade squamous intraepithelial lesion (VIN II/VIN III)
High-grade squamous intraepithelial lesion, usual type (VIN II/VIN III): This degree of refinement is not usually needed given that the great majority of practitioners equate HSIL with the common form of VIN II/VIN III.
VIN II or VIN III alone is also acceptable.
A precise risk of progression for classic HSIL is not possible given that so many individuals are treated. However, recurrence and increasing age are important factors. Jones et al. noted that 3.8% of women treated for HSIL developed a malignancy, 2% by failure to remove the HSIL and the other 1.8% as new “field” carcinomas. Chafe et al. identified unsuspected invasive carcinoma in 18.8% of patients undergoing surgical treatment for VIN. The mean age of this group was 58 years old, in contrast to 39 years old for those without invasion, emphasizing the increased risk after menopause. However, Jones et al. reported a mean age of 42 years old for their invasive group and cautioned that increased risk began in the fourth decade. They noted that prior radiotherapy, immunosuppression, and multicentric neoplasia were not risk factors for invasion.
Regression of VIN, like its counterpart in the male, has been reported. Features of this unique group include:
Young age (median 19 years)
Non-European ethnicity (81%)
Multifocal/pigmented lesions (81%/88%)
HPV positive (87%), usually HPV-16 (82.5%)
Lesions detected incidentally without prior symptoms (87%)
The preferred management for VIN is wide local excision. The recurrence rate with a negative margin is approximately 15% and with a positive margin approximately 50%. Selective use of CO 2 laser vaporization or topical treatment with imiquimod is used for patients with multifocal disease or clitoral involvement. Smoking cessation is strongly recommended.
As discussed earlier, the pathway to vulvar cancer involves a classic HPV-associated HSIL in about 40% of cases. However, in a majority of vulvar squamous malignancies, the epithelium adjacent to the cancer contains a range of alterations manifesting in underlying condition (LSC, lichen sclerosus), basal epithelial cells (atypia), and keratinocyte differentiation (dyskeratosis). Some may contain minimal or no appreciable basal atypias, but in many, there is a combination of dyskeratosis and mild to moderate atypia seen principally in the basal or suprabasal epithelial layers. There are several important aspects to this carcinogenic sequence:
It emerges in a background of vulvar inflammatory changes that are not linked to HPV, including lichen sclerosus and LSC.
The precursor lesion that emerges demonstrates more subtle nuclear atypias with conspicuous abnormalities in keratinocyte differentiation.
At least one molecular perturbation consists of loss of normal p53 function, and this has been indirectly linked to aneuploidy.
Loss of p53 function apparently can occur prior to the development of overt atypias, leaving open the question of precisely when or where the precursor can be separated from the preexisting conditions.
The sometimes subtle changes that occur in histopathology along the spectrum of HPV-negative precursors are mirrored in the associated invasive cancers that are often well differentiated and keratinizing. One of the conundrums faced by the practitioner is the very well-differentiated keratinizing squamous lesion that provokes the typical questions: “Is it neoplastic?” and if so “Is it invasive?” What the pathologist is seeking is a series of cellular changes that distinguish this form of precursor disease.
The clinical management is more problematic, inasmuch as these atypias may be indistinguishable from the surrounding dermatoses on gross examination or may be sufficiently extensive to create a significant management challenge. For the purpose of this discussion, the term differentiated VIN is used to connote this form of HSIL.
Differentiated VINs have the following attributes:
Unlike classic HSIL, differentiated VIN comprises a small proportion (less than 5%) of prospectively identified VINs.
They typically are identified in older women and share the clinical presentations associated with vulvar lichen sclerosus and LSC.
They are more commonly identified retrospectively, in reviews of epithelium adjacent to vulvar carcinomas, often in continuity with conventional-appearing vulvar lichen sclerosus with acanthosis (LSA) or LSC.
Differentiated VIN are less conspicuous clinically and may be impossible to separate from the background changes of LSC. Epithelial thickening (acanthosis), hyperkeratosis, verruciform changes, and ulceration may be present ( Fig. 6.18 ).

On gross examination, the pathologist needs to liberally sample the excision. One must focus on the conspicuous acanthotic or verruciform areas but also bear in mind the adjacent mucosa, inasmuch as the mutations that are associated with differentiated VIN (such as, in TP53) may occur in seemingly normal mucosa (see later).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here