Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Spinal masses include those arising from the central nervous system, as well as those arising from other organ systems with either direct extension or systemic spread to the spine.
It is important to remember that inflammatory processes such as transverse myelitis can present with mass-like features and congenital malformations such as lipomas or meningoceles can present as a mass. These entities should not be misdiagnosed as neoplastic.
An approach to a spinal mass starts with determination of whether the mass is intramedullary, intradural extramedullary, or extradural. Extradural masses can be additionally subdivided into those involving bone, bone and soft tissue, or soft tissue. This approach allows for a narrow differential diagnosis, which, in many instances, is the limitation of imaging and at which point a tissue diagnosis is required.
This section will illustrate the common and uncommon spinal masses in children using this organizational approach.
Spinal imaging modalities include radiographs, ultrasound, CT, and MRI. The majority of spinal masses are best evaluated with MRI, and consequently, the majority of diagnoses presented in this section will feature MRI images.


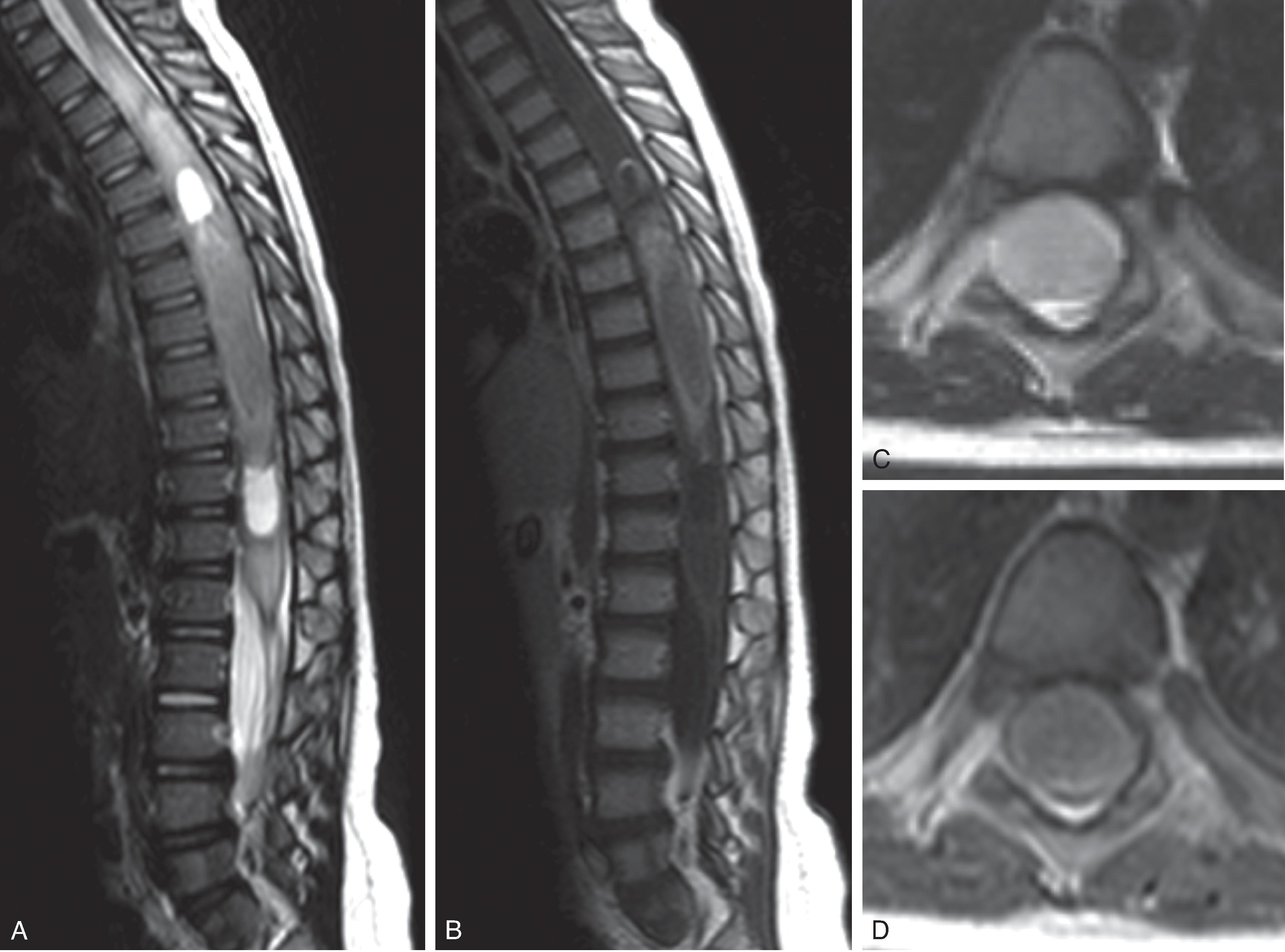
Astrocytomas are the most common intramedullary tumor in children (60%–80%).
Majority (90%) are low-grade astrocytomas (pilocytic > fibrillary). Pilocytic astrocytomas typical occur in children ages 1 to 5 years; fibrillary astrocytomas typically occur in children ∼10 years of age.
Clinical symptoms include progressive scoliosis, torticollis, head tilt, dysphagia, dysphonia, back pain, and weakness.
Location: Intramedullary mass.
MRI: Expansile T2W hyperintense. Variable enhancement. Usually no hemorrhage. May have a cyst and nodule pattern.


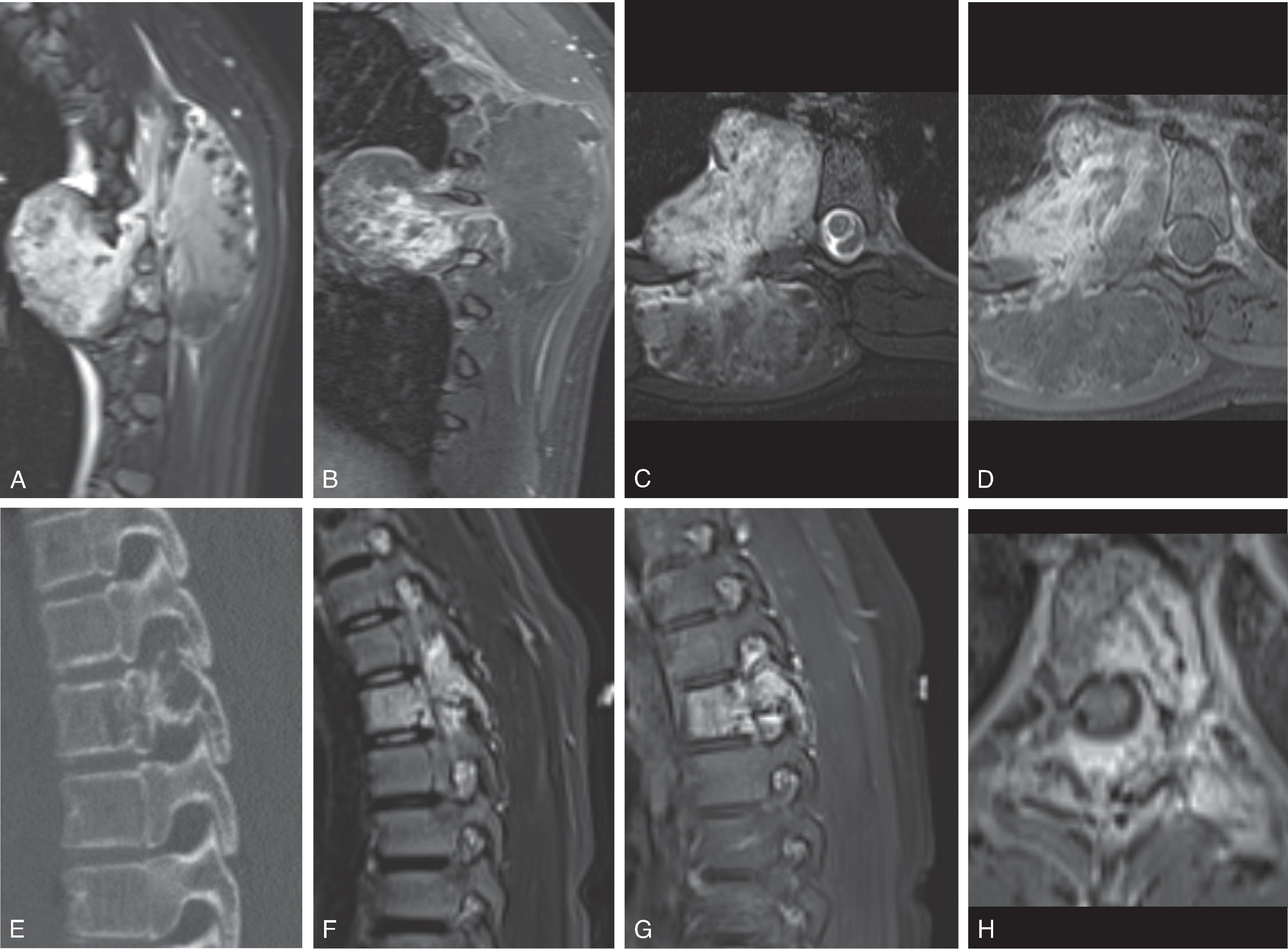

Usually extend craniocaudally <4 vertebral body lengths.
Tumor margins are usually indistinct.
Pilocytic astrocytomas can have a necrosis/cystic degeneration, cyst and nodule, or solid appearance.
Astrocytomas are more frequently located within the periphery of the spinal cord, but large size at presentation usually limits this as a helpful clue. Astrocytomas are typically ill defined and diffusively infiltrative without a clear cleavage plane.
DTI may be helpful for determining margins/resectability.
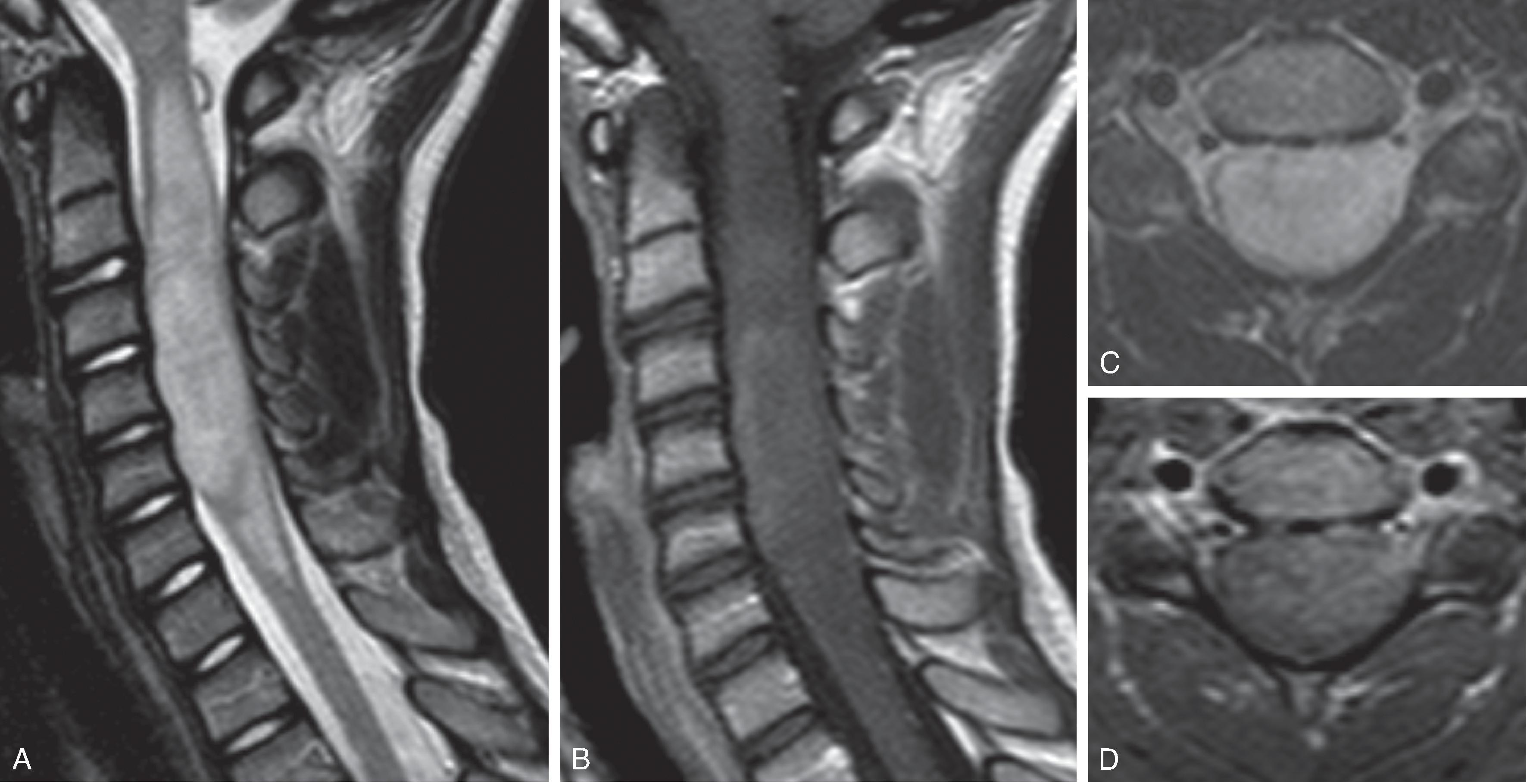
Location: Intramedullary mass
MRI: Well-defined nodular enhancement. Frequent cyst formation at the margins of the tumor. Intratumoral hemorrhage results in T2W hypointensity. “Cap sign” = hemosiderin at the cranial or caudal margin seen in 20% to 33%.
Ependymomas are more frequently noted in a central location surrounding the central canal and are more often expansile rather than infiltrative with a better defined cleavage plane compared to astrocytomas.
DTI fiber tracking demonstrating displaced tract rather than infiltration.
Neurofibromatosis Type-2 –associated ependymomas frequently small in size and multiple.
Radiotherapy can result in pseudoprogression demonstrating new peripherally enhancing lesion that spontaneously regresses over time.

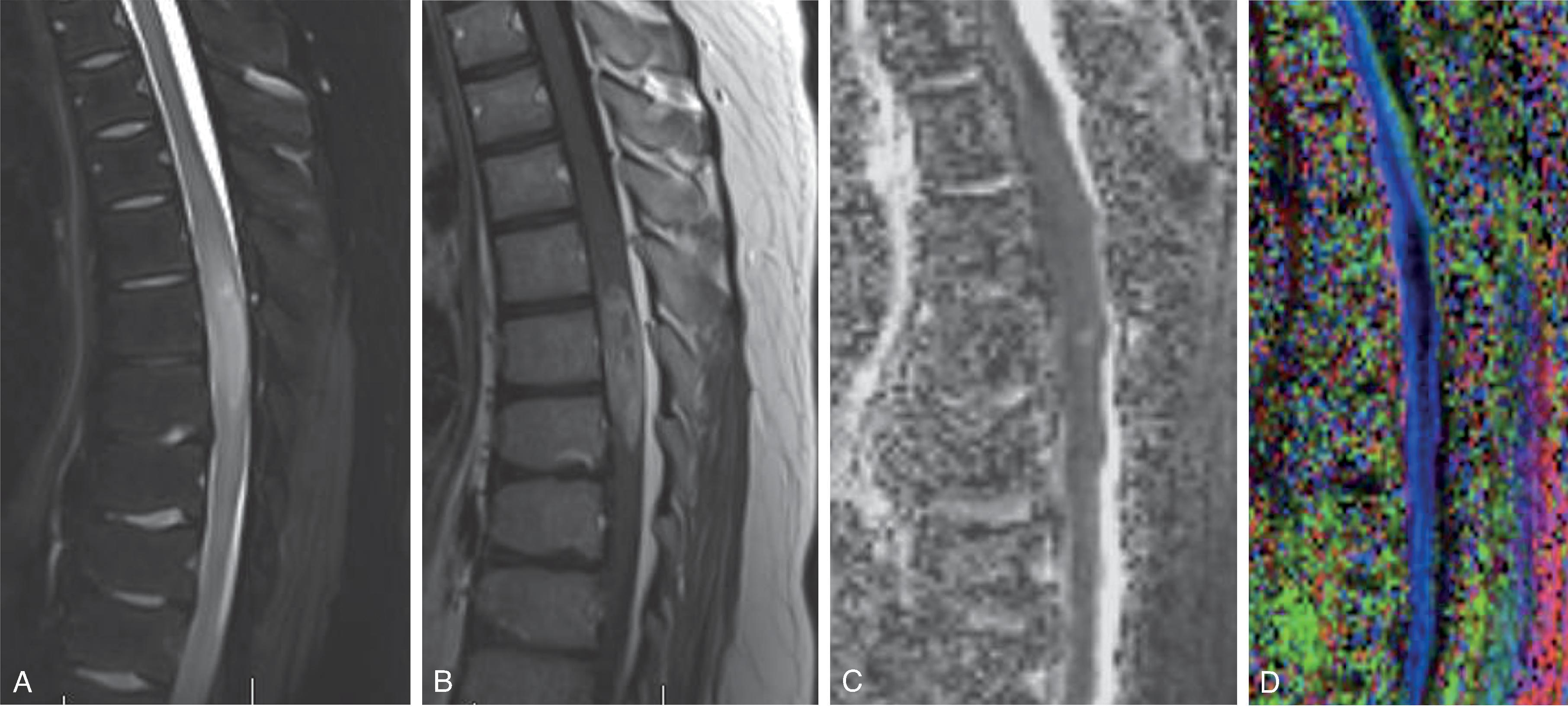
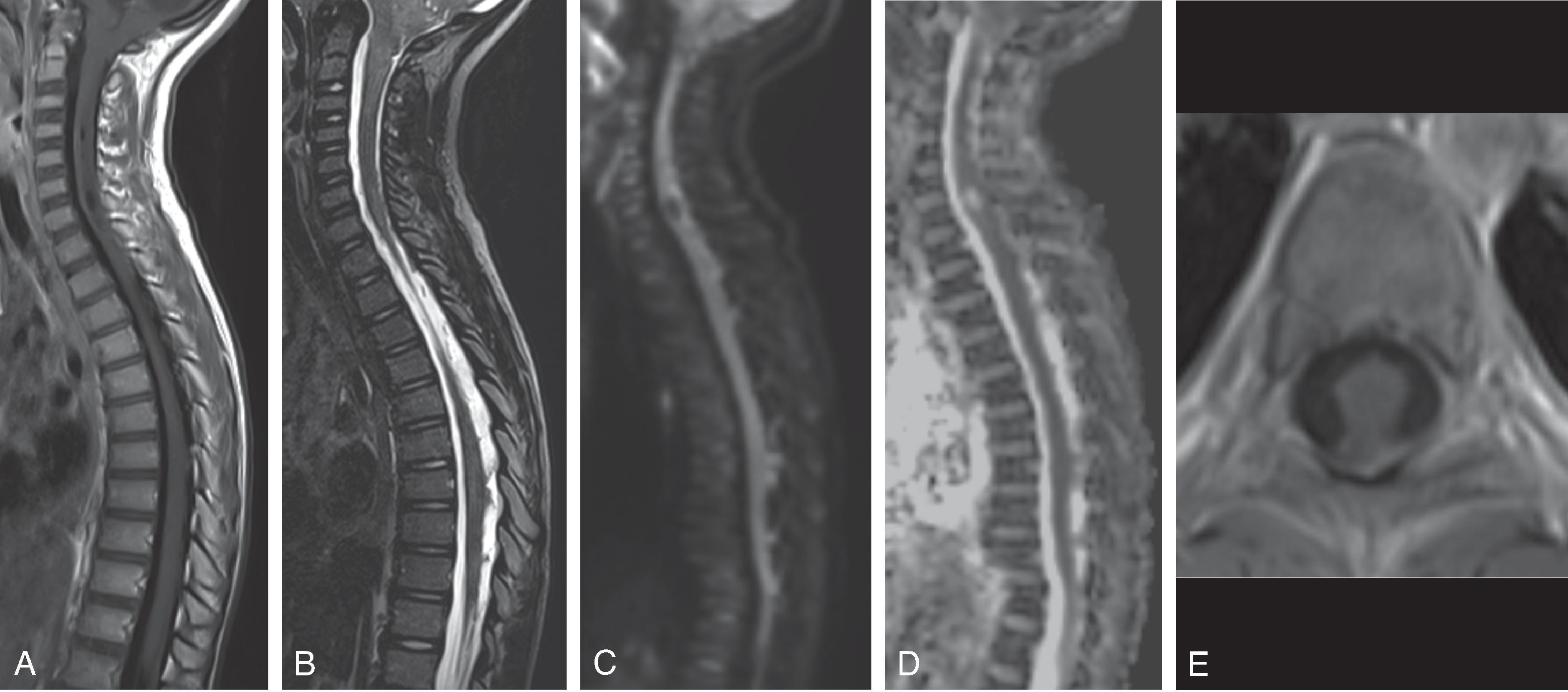
Third most common intramedullary spinal cord tumor in children (15%)
Low grade (WHO grade 1 and 2) with low potential for malignant degeneration
Age 1–5 years. Typically present with slow progression of pain, myelopathic symptoms, and/or scoliosis
Often centered in the cervical cord with extension to the medulla or upper thoracic cord
Location: Intramedullary mass
MRI: May appear completely solid or have cyst formation. Variable enhancement. May contain calcification
Currently not possible to distinguish from astrocytoma
Rare high-grade glioma of the spinal cord
H3K27M mutation similar to high-grade thalamic and pontine gliomas
Poor prognosis
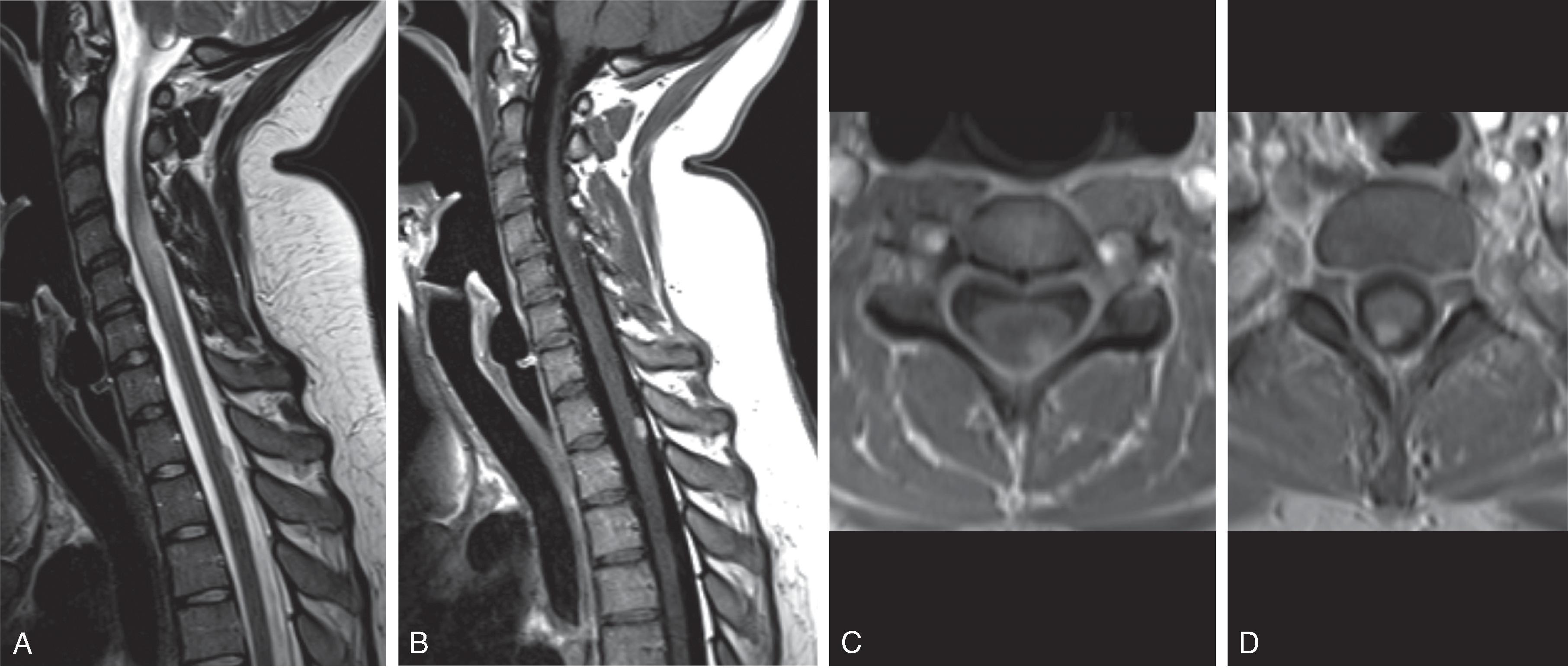
Benign vascular tumor
Arise from the pial surface so may appear on the surface of the cord
25% to 40% associated with Von Hippel-Lindau disease
Location: Intramedullary mass along the surface of the cord .
MRI: Typically small, circumscribed, avidly enhancing , and disproportionate cord edema . Larger tumors may have a cyst and nodule pattern.
Dilated feeding and or draining subependymal or subpial vessels may be noted.
Often multifocal and may be associated with von Hippel Lindau disease.
Coexisting intracranial lesions must be excluded.
Tendency to present with spontaneous intralesional hemorrhage including subarachnoid or intradural hemorrhage.
Location: Intradural extramedullary mass.
MRI: Variable T2 signal; variable but generally avid diffuse enhancement.
Located near the conus . Can be very large, and subsequently the origin could be difficult to determine.
Propensity to spread in the CSF despite low grade classification, requiring imaging of the entire spine and brain.
Chronic pressure may result in dorsal scalloping or deformity of the adjacent vertebral bodies.
Uncommon in children
Most commonly clear cell histopathology which has more aggressive behavior, higher recurrence rate, and potential for CSF spread
Associated with NF-2
Location: Intradural extramedullary mass
MRI: Homogeneous enhancement, circumscribed, dural tail
Rare occurrence in children, and often misdiagnosed as myxopapillary ependymoma when located near the conus
Significantly reduced diffusion due to high cellularity and, consequently, DWI-hyperintense with lowered ADC values
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here