Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A spinal orthosis is a device that provides support or restricts motion of the spine. Spinal orthoses may also be prescribed to treat spinal deformities such as scoliosis. All orthoses are force systems that act on body segments. The forces that an orthosis generates are limited by the tolerance of the skin and subcutaneous tissue.
To immobilize a painful or unstable spinal segment (e.g., spinal fracture)
To prevent or correct a spinal deformity (e.g., scoliosis, kyphosis)
To protect spinal instrumentation from potentially dangerous externally applied mechanical loads (e.g., postoperative immobilization following instrumented spinal fusion).
Orthoses may be described according to method of production (prefabricated, custom fit, computer-aided design and computer-aided manufacture [CAD-CAM]), rigidity (i.e., rigid, semirigid, flexible), location of origin (e.g., Milwaukee brace, Charleston brace), inventor (e.g., Knight, Williams), or appearance (e.g., halo). The most universally accepted classification system describes spinal orthoses according to the region of the spine immobilized by the orthosis:
Cervical orthosis (CO): for example, Philadelphia collar
Cervicothoracic orthosis (CTO): for example, sternal occipital mandibular immobilizer (SOMI) brace
Cervicothoracolumbosacral orthosis (CTLSO): for example, Milwaukee brace
Thoracolumbosacral orthosis (TLSO): for example, Jewett brace
Lumbosacral orthosis (LSO): for example, Chairback brace
Sacroiliac orthosis (SIO): for example, Sacroiliac belt
The patient’s body habitus
Likelihood of patient compliance
The intended purpose of the orthosis (motion control, deformity correction, pain relief, postoperative immobilization)
The location of the spinal segment(s) that require immobilization
The degree of motion control required
CO
CTO
Halo skeletal fixator
Cervical orthoses variably restrict flexion-extension, axial rotation, and lateral bending based on their design characteristics. In the normal cervical spine, axial rotation approaches 90º, lateral bending approaches 45º, flexion approaches 45º, and extension approaches 55º. Approximately 50% of cervical flexion-extension occurs at the occipital-C1 level and 50% of cervical axial rotation occurs at the C1–C2 level. Normal ranges of motion for each subaxial cervical spine segment are estimated as 8º–10º of flexion-extension, 3º–5º of axial rotation, and 2º–6º of lateral bending.
COs are cylindrical in design and encircle the neck region. They may be anchored to the mandible and/or occiput to increase stiffness and motion control. COs are commonly prescribed for pain associated with cervical spondylosis, stabilization following cervical spinal surgery, and protection and immobilization of the cervical spine following trauma.
COs may be soft or rigid. Soft collars provide no meaningful motion control. Rigid COs (e.g., Philadelphia, Miami-J) provide some restriction of flexion-extension, and to a lesser degree, restriction of rotation and lateral bending in the middle cervical region. However, motion restriction is less effective in the occiput to C2 region and lower cervical (C6–C7) region. COs are inadequate for immobilization of unstable spine fractures. Common types of COs include:
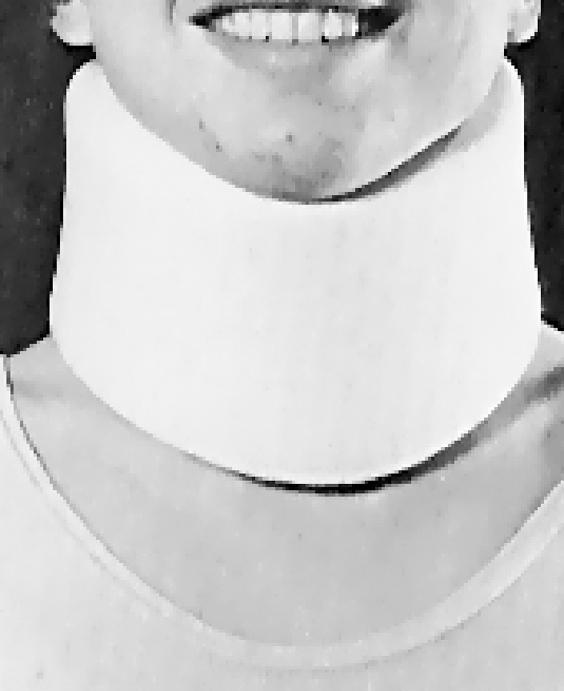
SOFT COLLAR ( Fig. 18.1 )
Design: Nonrigid; made of firm foam covered by cotton and fastened posteriorly with Velcro. Provides minimal restriction of cervical movement.
Indications: Cervical spondylosis, cervical strains. Allows soft tissues to rest, provides warmth to muscles, and reminds patients to avoid extremes of neck motion. Contraindicated in conditions in which cervical motion must be restricted (e.g., ligamentous injuries, fractures).
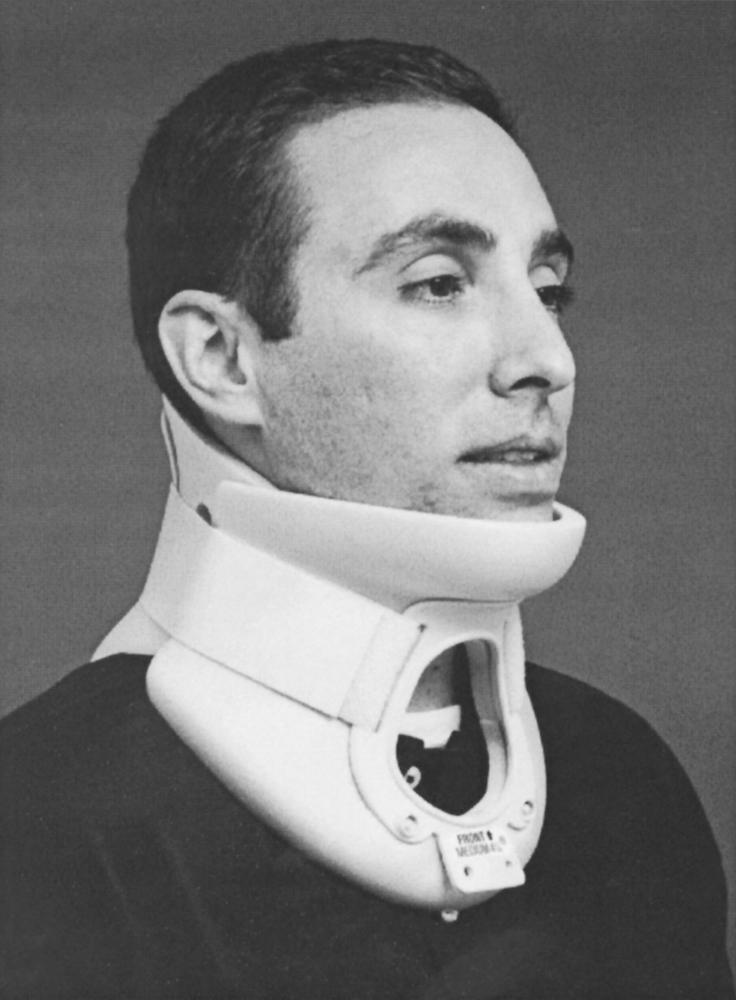
PHILADELPHIA COLLAR ( Fig. 18.2 )
Design: Two-piece polyethylene foam (Plastazote) collar with Velcro fasteners. Includes ventilation apertures, a molded chin support, and an occipital support. Tracheostomy style is available.
Indications: Stable cervical spine injuries, emergent mobilization of cervical injuries, and postsurgical immobilization. Contraindicated if the patient cannot tolerate pressure over the chin, occiput, or upper sternum.
MIAMI-J COLLAR ( Fig. 18.3 )
Design: Ventilated, two-piece polyethylene collar. Adjustable mandible and occipital components. Reported by patients to be more comfortable than Philadelphia collar. Provides greater limitation of cervical motion than Philadelphia collar.
Indications: Similar to Philadelphia collar. More appropriate for use in patients with altered mental status because collar-skin contact pressures generated by this brace are below maximal capillary skin pressure.

CTOs encircle the cervical region to a variable degree and use chin and occiput fixation attached to the trunk via straps or rigid circumferential supports. Two to four rigid uprights may be used to increase stiffness and improve motion control. CTOs are prescribed when greater motion restriction is desired in the middle and lower cervical spine compared with the motion restriction achieved with COs. These designs are generally reported to be more uncomfortable by patients. Common types of CTOs include:
TWO-POSTER CTO ( Fig. 18.4 )
Design: A metal orthosis consisting of single anterior and posterior uprights. Occipital, mandibular, sternal, and thoracic pads are attached. Difficult to use if the patient cannot sit erect.
Indications: Provision of support following cervical fusion procedures

FOUR-POSTER CTO ( Fig. 18.5 )
Design: Similar to two-poster CTO but with two anterior and two posterior uprights
Indications: Provision of support following cervical fusion procedures

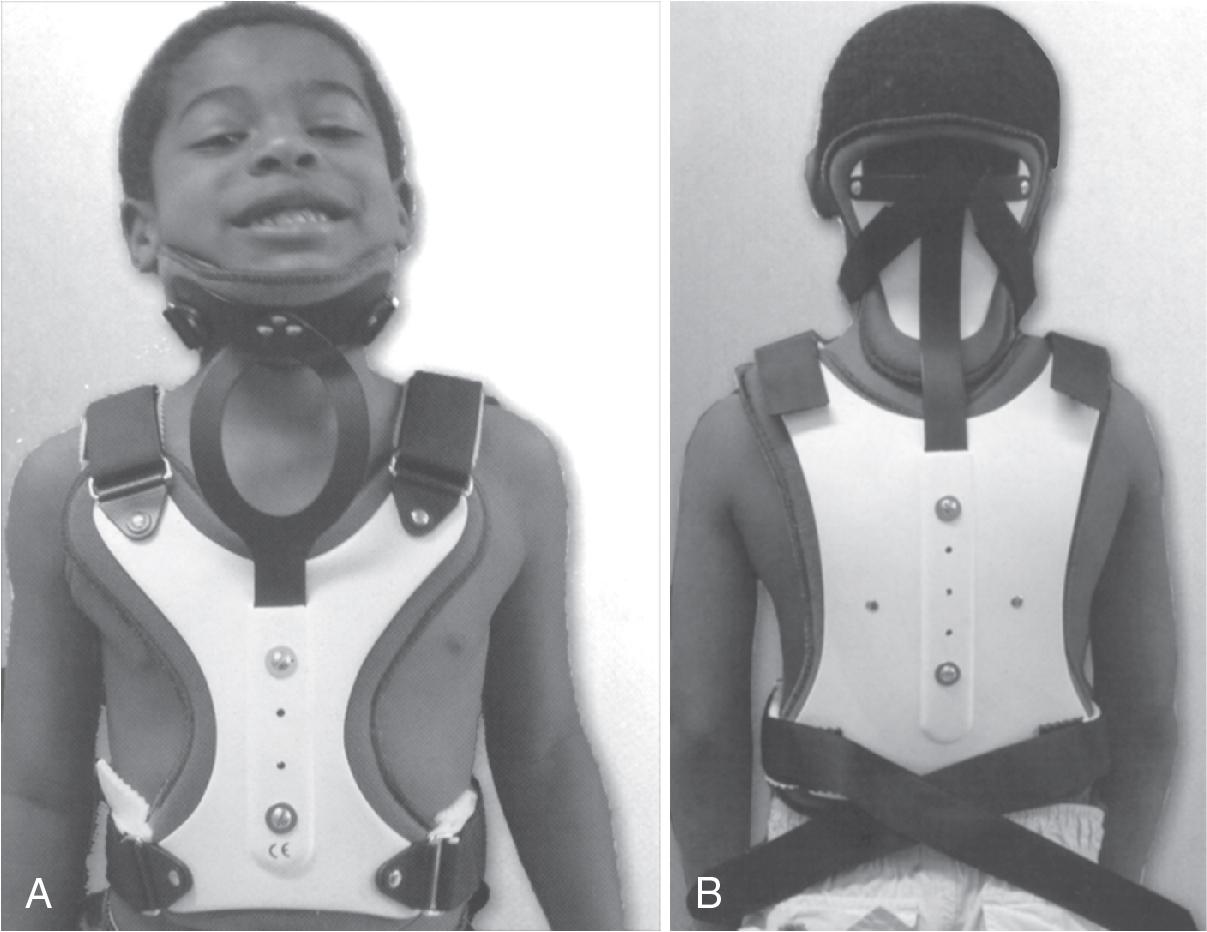
SOMI CTO ( Fig. 18.6 )
Design: The s ternal o ccipital m andibular immobilizer (SOMI) derives its name from its points of attachment. It consists of a sternal plate with shoulder components, a waist belt, and occipital and mandibular pads connected by uprights to create a three-post design. A head band may be added and is useful if the chin piece must be temporarily removed due to skin irritation. This orthosis can be more easily fitted to the supine patient than poster type CTOs because the uprights that maintain position of the occipital pad are attached anteriorly to the sternal plate. This brace is not compatible with magnetic resonance imaging (MRI).
Indications: Provision of additional support after cervical fusion procedures, immobilization of stable cervical fractures, and as a transition brace after treatment with a halo orthosis.

ASPEN CTO SYSTEM ( Fig. 18.7 )
Design: Consists of a CO attached to a thoracic vest via two or four posts
Indications: For maximum possible stabilization of the lower cervical and upper thoracic spinal regions. Indicated for minimally unstable fractures.

MINERVA CTO ( Fig. 18.8 )
Design: An occipitocervical support encircles the lower skull and supports the chin and subsequently attaches to an adjustable vest. This orthosis reduces axial load on the cervical spine and provides immobilization across the cervical region, as well as the cervicothoracic junction.
Indications: Similar to SOMI
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here