Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
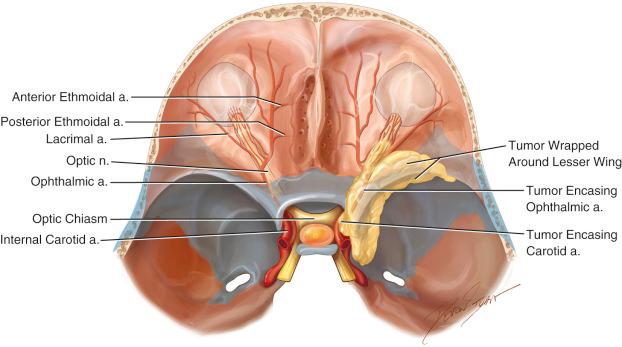
Meningiomas are one of the most frequently occurring intracranial primary tumors. Sphenoid wing meningiomas (SWMs) represent up to 18% of intracranial meningiomas. Those are anatomically located along the sphenoid ridge, the bony crest formed by the greater and lesser sphenoid wings. Medial SWMs are relatively common tumors associated with significant morbidity and mortality, primarily from their anatomic proximity to many critical neurologic and vascular structures. Medial SWMs cause displacement, encasement and usually invasion of neurovascular structures. These include the optic nerve, cavernous sinus, internal carotid artery (ICA) and its branches and the middle cerebral arteries ( Figure 32.1 ).
Visual loss is one of the major complications of this lesion, which has been reported to occur in 20–35% of cases.
Medial SWMs can also be accompanied with hyperostosis, brain edema, associated cysts and an en plaque component making the management of this lesion difficult.
Reactive hyperostosis, intraorbital involvement and/or venous congestion usually cause cosmetic problems such as exophthalmos. Diplopia is not rare, especially if the tumor involves the superior orbital fissure, cavernous sinus or the orbit. This can lead to cranial nerve palsies or restriction of extrinsic ocular muscles. Larger tumors that extend to the cranial convexity may produce hemiparesis and aphasia.
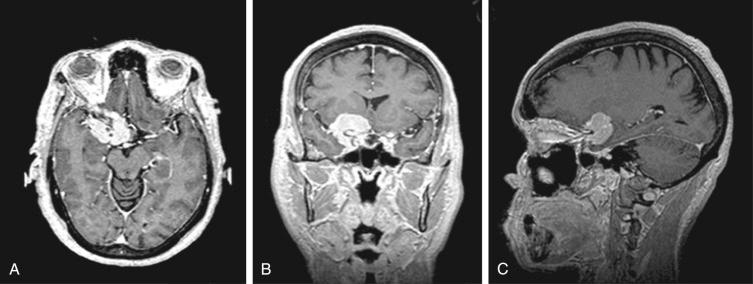
Useful preoperative imaging includes MRI with gadolinium enhancement and CT scanning, which is necessary to look at hyperostosis, bone involvement, as well as arterial/venous anatomy surrounding the tumor ( Figure 32.2 ). If there are concerns of vessel involvement, an angiogram can be performed. Angiography is also useful for identifying hemangiopericytomas, which may require preoperative embolization. Late-phase studies of the venous outflow may be important if the tumor involves one of the major sinuses.
Preoperative medical management, in addition to antibiotics, consists of mannitol (prior to incision, 0.5–1 g/kg ), dexamethasone (decadron 10 mg q4h) and antiepileptic medication (levitiracetam or phenytoin).
These tumors are approached through a large pterional craniotomy, giving access to the middle fossa and orbital roof. Different surgical modifications to this approach, such as the frontotemporal–orbitozygomatic, and supraorbital–pterional approach, are alternative approaches we use depending on the tumor size and location.
The tumor recurrence rate is low if removed completely at the first intervention. Ten year recurrence has been estimated to be between 9 and 15%. However, 30–50% risk recurrence has been reported in those cases invading the orbit. The aim of the surgery is to achieve a complete removal of the lesion including its dural origin as well as any bony invasion whenever possible.
The patient is positioned supine. After fixation in a Mayfield clamp, the head is extended, reduced and rotated 30° opposite to the lesion, in order to bring a vertical orientation to the sphenoid ridge. Appropriate patient positioning will avoid the need for brain retraction during the surgery.
A standard arching incision is performed extending from a half-centimeter anterior to the tragus to the contralateral midpupillary line.
A bicoronal incision may be helpful in tumors that extend anteriorly requiring an extended orbital osteotomy.
At the lower part of the skin incision, just anterior to the tragus, care must be taken to preserve the superficial temporal artery and the fronto-temporal branch of the facial nerve. At this point blunt scissors are used instead of a blade to enlarge the incision and to dissect the fad pat where the superficial temporal artery is encased until it is visualized and spared.
A myocutaneous flap, or a cutaneous and muscular flap, is usually performed. However, in cases where an orbitozygomatic craniotomy is needed, the temporal fascia is elevated together with its fad pat in order to preserve the enclosed branches of the facial nerve. The temporalis muscle is incised and dissected subperiosteally leaving a 1-cm cuff along the linea temporalis for its posterior reattachment.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here