Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The aim of fixation is to maintain clear and consistent lesional features and to preserve tissue in an optimal state suitable for a range of staining and ancillary histopathological techniques. Most fixation methods employed during tissue processing depend on chemical fixation of tissue in liquid reagents. Tissue fixation may also be accomplished by physical (heat, microwave, freeze-drying, and freeze substitution) and/or chemical (coagulant and cross-linking) methods. The most commonly used fixative is 10% neutral-buffered formalin solution with a pH between 7.2–7.4. It prevents the formation of formalin pigment in tissue sections. The quality of fixation is affected by:
the size of the specimen,
duration and temperature of fixation,
pH,
concentration,
osmolality,
ionic composition of fixatives and additives contained in the fixative.
Formalin fixation occurs at an approximate rate of 1 mm per hour. The volume of the fixative should ideally be at least 10 times the volume of the specimen. Large specimens, such as tumors, may require sectioning into 5-mm thick slices, covering with fixative-soaked gauze or cloth and fixation overnight.
Diagnostic dermatological biopsies may be:
small incisional (shave, core, punch),
excisional specimens.
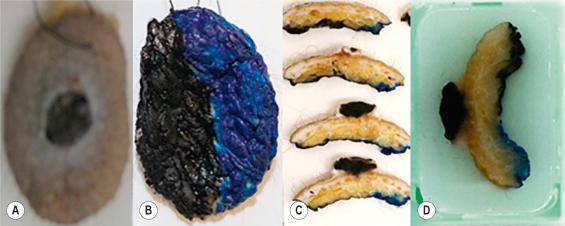
Prior to put-through, excisional specimens that require an appraisal of margins should be inked. If localization sutures have been inserted by surgeons then four-quadrant, four-color painting or two-color painted halves ( Fig. 2.1 ) is usually appropriate. Shave biopsies are used to sample or remove lesions and, if of appropriate size, may be divided into sections, bisected or trisected and embedded on edge. Edge embedding is critical in a shave excision of a lesion such as a small melanoma so that both the width and depth of invasion can be quantified. The main purpose of core or punch biopsies, which generally measure 2–8 mm in diameter, is for diagnostic sampling of larger lesions. Biopsies larger than 4 mm in size should be bisected and the specimens embedded with the cut surfaces down. The bisectioning and embedding cut surface down ensures that the lesion is not missed. Biopsies less than 4 mm are put through in toto .
Tissue processing refers to a series of steps that effect the removal of extractable water from biopsies to ensure sections of optimal diagnostic quality. These include fixation, dehydration, clearing, infiltration, and embedding in a support matrix. Use of manual and automated tissue processing achieves this goal, including:
carousel-type processors,
self-contained vacuum infiltration tissue processors ( Fig. 2.2 ),

microwave tissue processing.
In most laboratories, overnight processing runs are the norm. However, microwave-assisted tissue processing facilitates shorter processing times of 1–2 hours. Dehydrating reagents promote the removal of unbound water and aqueous fixatives from the tissue. Clearing reagents serve as an intermediary between the dehydrating and infiltrating solutions, being miscible with both. Paraffin is the most popular infiltration and embedding medium, being suitable for the majority of routine and special stains. The important principle to be adhered to during embedding of skin biopsies is that the orientation of the skin sample should offer the least resistance to the blade during microtomy ( Fig. 2.3 ). Skin biopsies are usually cut in a plane at right angles to the epidermis so as to minimize its compression and distortion.

Suboptimally processed tissue may result in incomplete tissue sections and expansion or disintegration of sections in the water bath. Incorrectly embedded tissue may result in poorly orientated incomplete sections. Faulty microtome mechanisms; loose, dull, or damaged blades; and inaccurate clearance angles may be the causes for:
The presence of calcified areas and suture in skin tissue and nicks in the blade may result in chatter or splitting of sections at right angles to the knife edge.
With the advent of immunohistochemistry, special stains are less commonly employed, but can still play an important role in highlighting certain tissue characteristics or for detection of infectious organisms.
Diagnostic sections are usually stained with hematoxylin and eosin (H&E), the most widely used routine stain. The hematoxylin component is positively charged and thus acts as a basic dye staining the negatively charged DNA in the nucleus blue-black. Eosin is anionic and thus acts as an acidic stain of the positively charged proteins comprising the cytoplasmic compartment and connective tissue resulting in variable shades and intensity of pink, orange, and red. The periodic acid-Schiff (PAS) technique is used widely to demonstrate:
glycogen,
starch,
sialomucin,
neutral mucin,
basement membranes,
α1-antitrypsin,
reticulin,
Russell bodies of plasma cells,
fungi.
The PAS technique is employed to demonstrate basement membrane thickening in lupus erythematosus, porphyria cutanea tarda, and in some tumors. Glycogen is digested by diastase, while neutral mucopolysaccharides are not—thus these PAS-positive components can be distinguished. Mucicarmine demonstrates acidic epithelial mucins. It is useful for the diagnosis of adenocarcinomas and the mucoid Cryptococcus neoformans capsule. Alcian blue highlights acidic mucopolysaccharides, staining the mucinous components of dermal mucinoses, granuloma annulare, scleredema of Bushke, lupus erythematosus, and metastatic adenocarcinomas among others. Alcian blue demonstrates heterogeneity of staining that is pH based: are demonstrated at pH 2.5 and sulfamucins at pH 1.0.
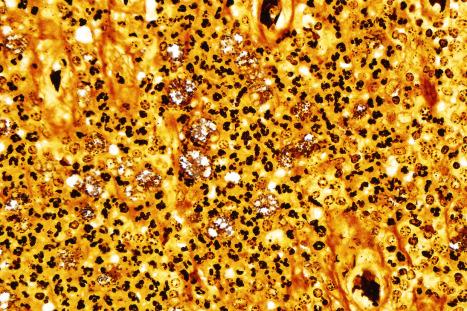
While colloidal iron, initially described by Hale for the identification of acid mucopolysaccharides, is as sensitive as Alcian blue for this purpose, its specificity and selectivity are debatable and background staining can be problematic. However, reduction of pH of the colloidal iron solution and inclusion of acetic acid washes may reduce this artifact. The high iron diamine stain, in contrast to colloidal iron, stains highly acidic sulfamucins but does not stain sialomucins or hyaluronic acid. Connective tissue stains highlight collagen, elastic and reticulin fibers. The trichrome stain, a combination of three dyes, is employed for the differential demonstration of muscle, collagen fibers, fibrin, and erythrocytes. Elastic fibers usually stain with eosin, phloxine, Congo red, and PAS stains but are demonstrated well and differentially with the Verhöeff method in the diagnosis of conditions like scleroderma, anetoderma, and pseudoxanthoma elasticum. Silver stains are useful to demonstrate reticulin fibers, melanin, and the identification of infective agents. While methenamine silver and Gomori-Grocott methenamine silver stains highlight fungi and bacteria, Warthin-Starry, Dieterle, and Steiner silver stains are particularly useful in the demonstration of spirochetes, Bartonella species and Donovan bodies ( Fig. 2.7 ). Masson-Fontana silver staining is pivotal to the staining of the cell wall of C. neoformans , especially in the identification of capsule-deficient C. neoformans. The role of the more commonly used special stains is summarized in Table 2.1 .
| Stain | Component | Outcome | |
|---|---|---|---|
| A. | Routine | ||
| Hematoxylin-eosin | Cells, connective tissue | Nuclei: blue Cytoplasm: pink/red Extracellular matrix: red/pink |
|
| B. | Carbohydrates & glycoconjugates | ||
| Periodic acid-Schiff (PAS) | Neutral mucins, glycogen | Magenta | |
| PAS-diastase | Glycogen, proteoglycans, HA resistant sialomucin | Resistant to diastase digestion | |
| Alcian blue, pH 2.5 | Labile sialomucin | Blue | |
| Alcian blue, pH 1.0 | Sulfomucin, resistant sialomucin | Blue | |
| Mucicarmine | Sialomucin, sulfomucin | Pink | |
| Colloidal iron | Sialomucin, sulfomucin HA, proteoglycans | Blue | |
| High iron diamine | Proteoglycans, sulfomucin | Blue | |
| Toluidine blue | Sulfomucin | Blue | |
| Hyaluronidase | HA | Sensitive to HA | |
| C. | Connective tissue fibers | ||
| Masson trichrome | Collagen | Blue or green | |
| Muscle, nerve | Red | ||
| Verhöeff-van Gieson | Elastic fibers | Black | |
| Pinkus acid orcein | Elastic | Dark brown | |
| Silver nitrate | Reticulum fibers | Black | |
| D. | Infective stains | ||
| Ziehl Neelsen | Acid fast bacilli | Red | |
| Fite-Faraco | (weakly) acid fast bacilli | Red | |
| PAS | Fungi, parasites | Magenta | |
| Mucicarmine | Cryptococcus sp | Red | |
| Giemsa | Leishmania sp, Donovan bodies |
Red Metachromatically purple |
|
| Methenamine silver | Fungi, bacteria | Black | |
| Grocott methenamine silver | Fungi | Black | |
| Warthin Starry silver | Spirochetes, bacteria | Black | |
| Dieterle and Steiner silver | Spirochetes, bacteria | Black | |
| E. | Other | ||
| Perl potassium ferrocyanide | Hemosiderin | Blue | |
| Oil red O | Lipids | Red | |
| Scarlet red | Lipids | Red | |
| Von Kossa | Phosphate (often as calcium phosphate) | Black Black |
|
| Alizarin red S | Calcium | Orange-red | |
| Alkaline Congo red | Amyloid | Apple green birefringence | |
| Chloro-acetate esterase | Myeloid series | Red granules |
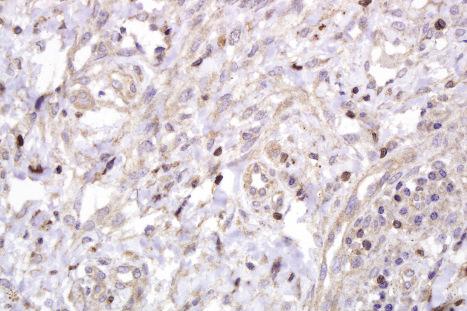
Since the first practical application of antibodies using the peroxidase-labeled antibody method on paraffin-embedded tissues in 1968, immunohistochemistry (IHC) has emerged as a powerful supplementary investigation to histomorphological assessment. IHC has widespread dermatopathological diagnostic, prognostic, therapeutic, and pathogenetic applications, not only in a range of neoplastic ( Table 2.2 ), immunobullous, and infective disease, but also in the distinction between reactive and neoplastic disorders. Immunohistological techniques can be performed manually or in automated platforms ( Fig. 2.8 ). While automation allows enhanced quality and reproducibility of staining; detailed, exact IHC protocols are critical in the many laboratories that still perform manual IHC, to achieve optimal, reproducible results.
| Stain | Application |
|---|---|
| Epidermal and appendageal neoplasms | |
| AE1/AE3 | Pan-keratin. Confirms epithelial lineage |
| CAM 5.2 | CKs 8,18. Confirm epithelial lineage. Useful to confirm glandular neoplasms |
| MNF 116 | CKs 5, 6, 8, 17, 19. Useful in diagnosis of SCC with single cell infiltration |
| BerEP4 | Positive in BCC. Negative in SCC |
| CK 7 | Confirmation of mammary and extramammary Paget disease |
| p63 | Distinguish primary cutaneous spindle SCC from mesenchymal spindle cell tumors & primary cutaneous adnexal from metastatic adenocarcinomas |
| CD10 | Trichoepithelioma: positive in stroma and papillae, negative in epithelium. BCC: positive in epithelium, negative in stroma |
| bcl2 | Positive in BCC, negative in SCC |
| Vascular proliferations | |
| ERG | Nuclear staining in endothelial cells. High specificity and specificity for endothelial tumors (better than CD31) |
| CD31 | High specificity and good sensitivity for endothelial tumors |
| CD34 | High sensitivity but low specificity for endothelial tumors |
| Fli-1 | Nuclear staining of endothelial cells |
| GLUT 1 | Positive in endothelial cells of all juvenile hemangiomas. Usually negative in congenital hemangiomas (rapidly involuting congenital hemangioma and noninvoluting congenital hemangioma) |
| Melanocytic tumors | |
| S100 protein | Most widely used melanocytic marker. It is highly sensitive but not as specific as other melanocytic markers |
| Sox-10 | Newly introduced melanocytic marker also positive in neural tumors. Very useful in spindle cell melanomas including desmoplastic melanoma and in the evaluation of intraepidermal melanocytic proliferations as lentigo maligna (nuclear staining) |
| MITF-1 | Low specificity but useful in the evaluation of intraepidermal melanocytic proliferations (nuclear staining) |
| HMB 45 | Good specificity but relatively low sensitivity. Tends to be negative in spindle cell melanoma. Also positive in PEComa |
| Melan A/Mart 1 | Similar specificity to HMB45. Tends to be negative in spindle cell melanomas |
| Ki-67 | Higher proliferation index in melanoma (13–35%) than in nevi (< 5%). Useful in the evaluation of some melanocytic tumors, mainly nevoid melanoma |
| Neuroectodermal and neural tumors | |
| S100 protein | Positive in neuroectodermal, neuronal, nerve sheath, chondroid tumors, some sweat gland tumors, and myoepithelioma |
| NSE | Merkel cell carcinoma |
| CK 20 | Merkel cell carcinoma |
| Neurofilament | Merkel cell carcinoma |
| Chromogranin | Merkel cell carcinoma |
| Synaptophysin | Merkel cell carcinoma |
| TTF1 | Negative in most Merkel cell carcinoma |
| Myogenic/myofibroblastic differentiation | |
| MSA | Tumors of muscle origin |
| Desmin | Tumors of muscle origin (smooth muscle and skeletal muscle, rarely and focally in myofibroblastic tumors) |
| Myogenin | Positive in rhabdomyosarcoma |
| SMA | Positive in smooth muscle tumors, glomus tumor, myopericytoma, dermatomyofibroma |

In many centers, IHC is now the most commonly utilized ancillary test for clinical tissue samples.
Historically, the introduction of enzymes as labels in IHC overcame difficulties associated with immunofluorescence, including the inability to assess histomorphology with the latter. The peroxidase-antiperoxidase (PAP) technique was replaced by alkaline phosphatase-antialkaline phosphatase (APAAP) techniques and avidin-biotin complex (ABC) labeling. Although the streptavidin-biotin labeling system gained popularity, the endogenous biotin-associated background staining under certain circumstances has resulted in increasing use of labeled polymer-based detection systems, suitable for manual and automated IHC platforms ( Fig. 2.9 ).
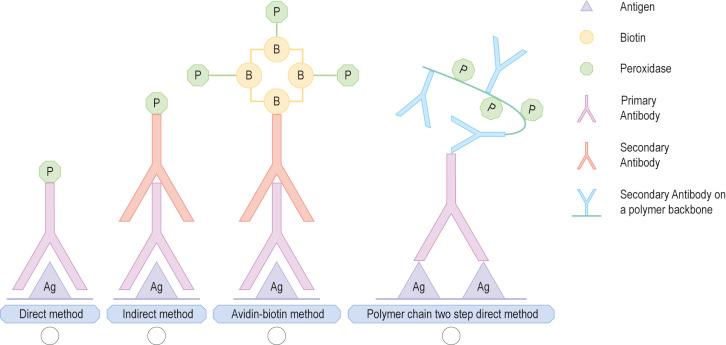
The direct conjugation of the primary antibody to the label formed the principle of the initial, traditional direct technique, in which the labeled antibody reacted directly with the tissue antigen. In the two-step indirect technique, labeled secondary antibody directed against the immunoglobulin of the animal from which the primary antibody was obtained to visualize the unlabeled primary antibody. The labeled streptavidin-biotin (LSAB) method is a three-step technique. An unconjugated primary monoclonal or polyclonal antibody attached to the tissue antigen forms the first layer, creating an antigen-antibody complex. The second layer is formed by a biotinylated secondary antibody raised against the same species of the primary animal. The secondary antibody binds to the primary antibody with the biotinylated end being available for binding to a third layer. This layer may bind either to enzyme-labeled streptavidin or to a complex of enzyme-labeled biotin and streptavidin. The enzyme may be horseradish peroxidase or alkaline phosphatase. An appropriate chromogen is used for detection. In the peroxidase method, peroxidase-oriented chromogens such as diaminobenzidine or 3-amino-9 ethylcarbazole are appropriate. Indole reagents (red), naphthol fast red (red), or NBT/BCIP (blue) are the chromogens used in the alkaline phosphatase-streptavidin method.
The presence of endogenous biotin and resultant background staining led to the introduction of the increasingly popular polymer-based immunohistochemical methods. In the new direct enhanced polymer one-step (EPOS) technique, approximately 70 enzyme molecules and 10 primary antibodies are conjugated to a dextran ‘backbone.’ While the entire IHC procedure is completed in one step, the method is limited to highly select manufacturer-specific primary antibodies. Other newer polymer detection systems with a dextran backbone to which multiple enzyme molecules may attach are available for manual and automated IHC. These quick, reliable, and reproducible techniques are also characterized by greater sensitivity. Single-, dual-, triple-, and multi-color staining with different chromogens is possible.
Background staining is a common difficulty that has multiple predisposing causes. While monoclonal antibodies reduce non-specific background staining, not only must antibody concentrates and prediluted preparations be optimized for usage at the correct dilution in different laboratories ( Figs 2.10 and 2.11 ), diluent pH is also critical in ensuring the absence of antibody degeneration and resultant background staining. Avidin-biotin detection systems and horseradish peroxidase systems may require biotin blocking and endogenous peroxidase quenching steps to decrease unnecessary background staining. Polymer-based detection systems can effectively eliminate biotin-induced false-positive staining. While antigen retrieval techniques are critical for antigen unmasking, optimal results require control of the pH and temperature of retrieval solutions and controlled enzymatic digestion. The latter may cause variable tissue loss ( Fig. 2.12 ), excessive background staining when sections are exposed to increased digestion time, inappropriate high temperature and inadequate rinsing, causing protein diffusion into or deposition in skin sections and background staining.
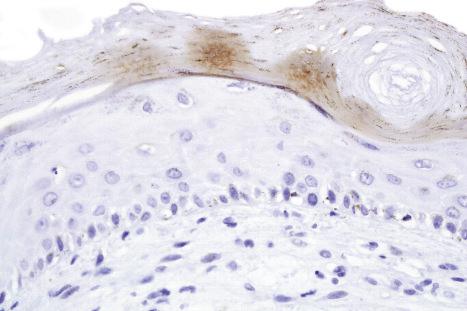

Chromogen entrapment, precipitation, and contaminants may lead to false-positive interpretation of an IHC test. Depletion of peroxidase or alkaline phosphatase chromogenic activity, a consequence of the breakdown of chromogens because of the sensitivity to light and heat, results in a background blush. A similar effect is seen when there is inadequate chromogen rinsing or prolonged chromogen time. Filtering of the chromogen is effective in preventing chromogen precipitation. Chatter, tears, folds and wrinkles and poor adhesion of sections to slides causes entrapment and suboptimal rinsing of chromogen ( Fig. 2.13 ). Skin sections with a thick stratum corneum, dermal calcification, or sclerosis may be prone to these artifacts, requiring meticulous microtomy to prevent its occurrence. The improper handling of water baths, tissue sections, and slides with ungloved hands may cause contamination of sections with squames.
False-negative immunostaining may also compromise IHC interpretation. Incomplete deparaffinization causes suboptimal or incomplete staining because of incomplete tissue penetration by the antibody. Overdigestion of tissue sections by proteolytic enzymes can destroy the tissue sections with attendant loss of antigen for antibody binding. Other causes of false-negative immunostaining include:
incorrect temperature of reagents, including retrieval solutions,
expired antibodies,
inappropriate dilutions,
suboptimal storage of antibodies.
Immunofluorescent techniques have the potential to define antigen-antibody interactions at a subcellular level. This interaction requires the irreversible binding of a readily identifiable label for its recognition. Fluorochromes such as rhodamine or fluorescein are labels that can absorb radiation in the form of ultraviolet or visible light. Direct and indirect immunofluorescence (IMF) techniques demonstrate a range of tissue antigens of dermatopathological importance, including the diagnosis of infectious and autoimmune blistering disorders. In the direct IMF technique, antibody is conjugated directly with a fluorochrome and is used to detect an antigen in a tissue section using ultraviolet light microscopy. In the indirect IMF technique, patient serum (containing the antibodies) interacts with a tissue section containing the antigen. Antibody to a human immunoglobulin, conjugated to a fluorochrome, is applied thereafter. The successful demonstration of the antigen requires the antigen to remain sufficiently insoluble in situ . Skin biopsies for direct immunofluorescence can be transported fresh on saline-soaked gauze in a container on ice, or in a transport medium such as Michel medium. The transport medium must be maintained at a pH of 7.0–7.2. The main uses for IMF in dermatopathology are in the interpretation of the autoimmune blistering diseases, lupus erythematosus, and vasculitis. In general, immunofluorescence has the following advantages over immunohistochemistry:
more sensitive detection of antigen.
use of special fixation that preserves ‘difficult’ antigens.
Fading of immunofluorescence sections can be overcome by the use of anti-fading mountants.
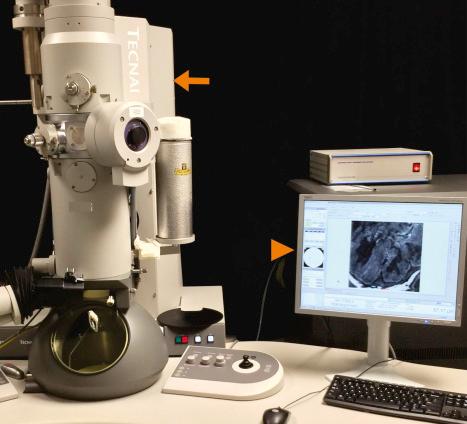
Electron microscopy is much less utilized than in the past. Immunohistochemical approaches are preferred in those instances where they are a reasonable substitute.
Transmission electron microscopy offers much better resolution than light microscopy. To optimize this, tissue has to be embedded in extremely rigid material to allow ultrathin sectioning at 80 nm. In most circumstances, hydrophobic epoxy resins are preferred. When a specimen requires ultrastructural examination, the portion to be examined must be treated in a suitable fixative immediately. The volume of the fixative should be 10 times the sample size. The final specimen is cubed to 1 mm portions. Fixation is affected by:
pH,
osmolarity,
ionic composition of buffer,
fixative concentration,
temperature,
duration of fixation.
Primary fixation in an aldehyde, usually glutaraldehyde, and secondary fixation in osmium tetroxide are standard procedures. Advances in immunohistochemistry have decreased the dependence on electron microscopy for ultrastructural confirmation of cell lineage. Notwithstanding, dermatologic ultrastructural investigations are important in the diagnosis of:
undifferentiated tumors,
immunobullous disease,
cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL),
amyloidosis,
metabolic storage diseases.
Intercellular junctions, Weibel-Palade bodies, melanosomes, and premelanosomes may help in the diagnosis of carcinomas, endothelial tumors, and melanocytic tumors, respectively. In CADASIL, extracellular, electron-dense granular material is present in an indentation in vascular smooth muscle cells. Amyloid is identifiable as randomly arranged, extracellular, nonbranching fibrils of indeterminate length and 7–10 nm diameter. Transmission electron microscopy remains a valuable tool in the ongoing evaluation of the structure of normal and pathological human cell and tissue components and infective agents. Technological advancements have enabled electronic capture of ultrastructural images ( Fig. 2.14 ).
Although frozen section appraisal of the skin is undertaken mainly for assessment of excision margins of cutaneous tumors, it may also be used for primary diagnosis of cutaneous lesions. Frozen section evaluation of incisional (punch, shave) or excisional biopsies can be performed. Frozen section specimen processing and sectioning is undertaken in a cryostat (‘cryo’ referring to cold and ‘stat’ referring to stationary) ( Fig. 2.15 ), a refrigerated steel cabinet with a holding temperature of −5 to −30°C, containing a microtome and an anti-fogging air circulating system. Commercially available freezing mixtures, e.g., optimum cooling temperature (OCT) mixture, enables rapid fixation of the skin sample on a freezing stage. Evaluation of tumor margins by conventional or Mohs micrographic surgery is expensive and time consuming; hence cases for frozen section assessment must be selected carefully. Indications for frozen section evaluation include lesions with poorly defined clinical margins, infiltrative growth patterns, and longstanding and/or recurrent lesions, especially those in locations where skin preservation is necessary.

Cytopathological investigation of selected skin lesions has excellent outcomes in dermatopathological practice if used appropriately. Cytodiagnostic skin testing, introduced in the previous century by way of the Tzanck test, currently encompasses exfoliative and aspirational sampling methods. The exfoliative technique involves touch imprints or gentle scraping of a skin lesion with a straight scalpel and smearing of the scraped contents onto a slide, air drying, and staining with hematoxylin and eosin, May-Grünwald-Giemsa, or Papanicolaou stains. The main indications for exfoliative cytology in dermatological practice includes autoimmune bullous disease infections and genodermatoses. Fine-needle aspiration cytology may be used for the initial diagnosis of some superficial, palpable nodular, tumoral lesions inclusive of basal cell carcinomas, Langerhans cell histiocytosis, mast cell diseases, and adnexal tumors and infections but limitations of the technique include technical training of aspirators, poor cellular yields, and lack of assessment of tumor patterns and excision margins. Issues related to tumor patterns and excision margins may be overcome by various cell block techniques that may be undertaken when small aspirated tissue fragments are unsuitable for cytological preparation and for processing of residual cell sediments after smear preparation. Cell block preparations have evolved from simple sedimentation techniques to sample centrifugation and the addition of a range of cellular adjuvants for cell cohesion. The fundamental steps in cell block preparation encompass fixation, centrifugation and cell pellet hardening and transfer for paraffin embedding. The most popular adjuvants for manual pellet hardening include plasma thrombin and agar techniques. Recent technological advances have introduced automated cell block preparation that are claimed to have shorter processing times, maintain crisp and clear cellular architecture, maximized cellularity, reduced cross-contamination risk, and minimal operator-associated result inconsistency.
An efficient approach to genetic testing often relies on initial traditional histologic characterization of skin biopsies.
Recent advances in molecular genetics and gene sequencing have led to many inherited skin diseases being diagnosed or confirmed by clinical molecular biologists rather than dermatopathologists. Analysis of skin biopsies still remains vital for the accurate diagnosis of several genodermatoses, and often provides a guide for subsequent molecular analyses. Examination of the skin biopsy informs the selection of additional molecular testing. Communication between the dermatopathologist and molecular laboratory is absolutely critical for efficient use of molecular techniques.
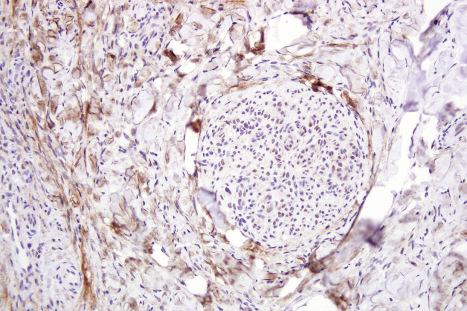
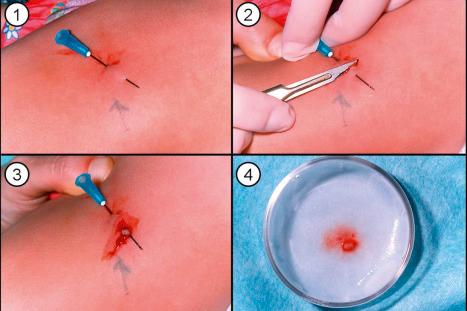
Analysis of the inherited skin blistering disorder known collectively as epidermolysis bullosa (EB) discussed in detail in Chapter 4 demonstrates the complex, multifaceted approach to diagnosis required in such cases. EB has been shown to result from mutations in at least 18 different genes encoding different structural proteins at or close to the dermal-epidermal junction or within the epidermis ( Fig. 2.16 ). Clinically, the different types of EB are characterized by widely differing prognoses, from death in early infancy to blistering that may become milder in later life. The clinical presentation in neonates, however, can be confusing to dermatologists and pediatricians because of the overlapping features ( Fig. 2.17 ). In these circumstances, skin biopsy, usually a superficial shave biopsy since the key region is usually the dermal-epidermal junction, can provide critical diagnostic and prognostic information. Typically, non-blistered skin is sampled; clinicians should be discouraged from biopsying established blisters however because of the potential artifact associated with re-epithelization and misrepresentation of the true plane of cleavage. Just before the biopsy is taken, the non-blistered skin is rubbed gently in an attempt to induce fresh microsplits in the skin to facilitate the microscopic subtyping of EB ( Fig. 2.18 ).
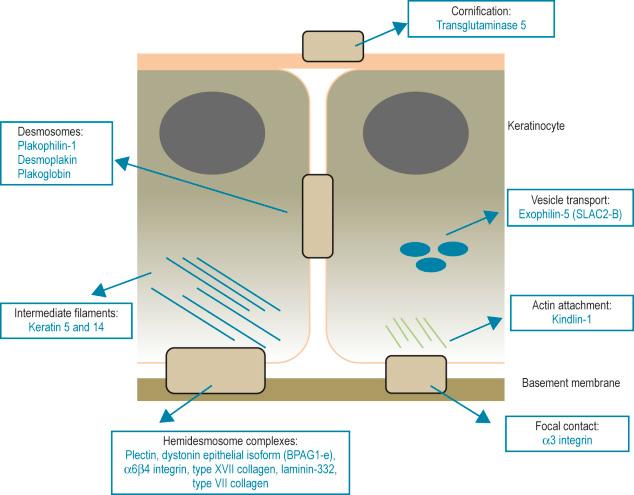

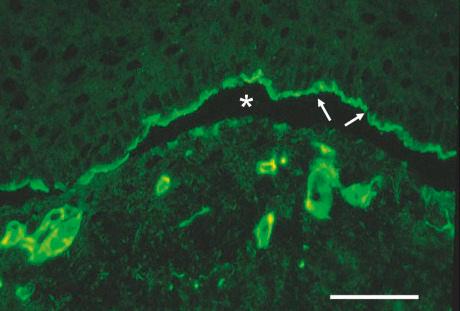
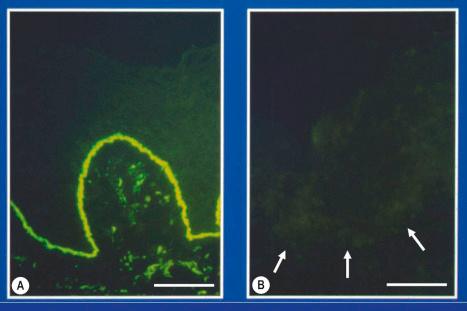
The most informative investigation is immunolabeling of the dermal-epidermal junction (and keratinocyte junctional proteins for more superficial forms of EB, if necessary) using a panel of basement membrane or desmosomal antibodies. Skin biopsies can be transported in Michel medium to a diagnostic laboratory at ambient temperature: this fixative is extremely useful since basement membrane zone and desmosome immunoreactivity is maintained for at least 6 months. For the immunolabeling, frozen skin sections are used rather than formalin-fixed paraffin-embedded material because the antigenic epitopes of several transmembranous proteins may be lost in routine skin processing. The antibodies can be used either to determine the level of cleavage in the skin (antigen mapping) or to see if there is a reduction or absence of immunostaining for a particular antigen. Fig. 2.19 , for example, demonstrates labeling using an antibody against type IV collagen in skin from the neonate illustrated in Fig. 2.17A . In this example, labeling maps to the roof of the split. This indicates that the lamina densa is in the blister roof and that there is a sublamina densa plane of blister formation. These findings support a diagnosis of dystrophic EB. This diagnosis can be refined by immunolabeling with an antibody to type VII collagen, as shown in ( Fig. 2.20 ). In normal skin there is bright, linear labeling at the dermal-epidermal junction; however, in the skin from the neonate shown in Fig. 2.17A , there is a complete absence of type VII collagen immunoreactivity. All other antibodies show normal reactivity at the dermal-epidermal junction. These findings therefore establish a diagnosis of generalized severe recessive dystrophic EB. Reduced or absent immunolabeling with specific basement membrane antibodies is an extremely useful and rapid means of diagnosing recessive forms of EB. For example, skin from the neonate shown in Fig. 2.17C demonstrated a lack of reactivity against laminin-332 but normal immunostaining for all other antibodies. These findings establish a diagnosis of generalized severe junctional EB.
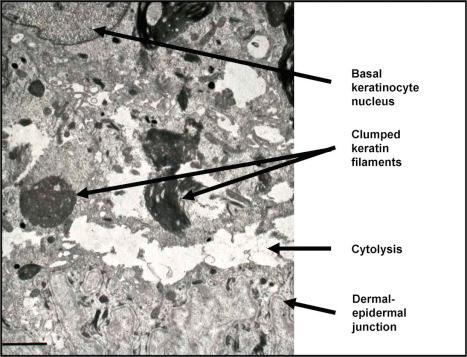
The development of a panel of antibodies for the target proteins implicated in the different forms of EB, most of which are commercially available, has led to decreased emphasis on transmission electron microscopy as a diagnostic tool in EB. Ultrastructural analysis, however, can be useful in confirming the plane of cleavage and in establishing the diagnosis of certain dominant forms of EB. Skin from the neonate illustrated in Fig. 2.17B , for example, shows normal intensity basement membrane zone reactivity for all diagnostic probes but transmission electron microscopy ( Fig. 2.21 ) identifies discrete clumps of tonofilament and basal keratinocyte cytolysis, characteristic of the generalized severe variant of autosomal dominant EB simplex. For recessive forms of EB, however, skin immunolabeling has become the most important diagnostic approach. Reduced or absent staining for a particular protein provides a rapid diagnosis as well as a means of identifying the encoding gene (or genes) in which the underlying pathogenic mutations are present. Thus the skin biopsy findings, both histologic and immunohistochemical, provide a direct guide to molecular screening tests, most of which are PCR-based or next-generation sequencing (NGS)–based, as discussed below. For dominant forms of EB, however, skin immunohistochemistry of patient skin may be indistinguishable from normal control skin and therefore Sanger sequencing of DNA is often preferred to skin biopsy analysis as the initial diagnostic investigation. Indeed, DNA sequencing is the optimal method for diagnosing the most common form of EB, localized EB simplex (blisters mainly on the hands and feet, which accounts for > 70% of all cases of EB). Furthermore, the diagnosis of EB is increasingly embracing NGS technologies, including whole exome sequencing and selected gene panels, as primary diagnostic tools. This molecular information can then be used for genetic counseling, carrier screening, and DNA-based prenatal testing, if indicated. Nevertheless, a clear advantage of skin biopsy diagnostics for EB is time to diagnosis: skin immunohistochemistry can be completed within 2 days and thus skin biopsy is likely to remain a key part of EB diagnostics, particularly in the diagnosis of neonates with EB, for the foreseeable future.
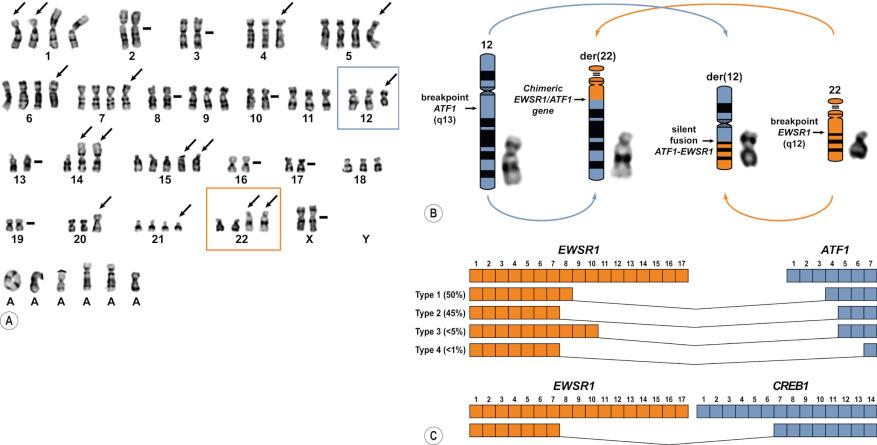
This technique can be used as an initial screen to demonstrate gross chromosomal aberrations associated with certain tumors. Most skin tumors are small and thus tissue is generally not set aside for karyotype analysis.
Chromosomal karyotyping is the historical gold standard for detecting chromosomal aberrations in neoplastic tissue ( Fig. 2.22 ), though many other excellent techniques now exist as well. Fresh tumor tissue is required to grow the cells and the cytogenetic preparations and interpretation require skilled personnel. Nonetheless, this technique provides an open, unbiased look at all of the chromosomes of a particular tumor. Total chromosomal gains and losses and also translocations between chromosomes can be demonstrated. Some of these chromosomal translocations are virtually diagnostic of certain tumors, particularly soft tissue and hematopoietic tumors. Other chromosomal changes can be suggestive of certain tumor types. While most translocations are now confirmed by the other molecular methods described below, traditional chromosomal karyotyping retains a minor role as an initial examination of the chromosomal complement of a neoplasm and an important tool for discovery of new chromosomal aberrations. Historically, the discovery of chromosomal translocations within specific tumor types is proportional to the number of cases karyotyped. More recently, this discovery modality has been supplanted by massively parallel sequencing techniques (NGS), in particular RNA sequencing discussed further below. The interpretation of complex karyotypes can be informed by additional methodologies discussed below such as spectral karyotyping (SKY) or multiplexed fluorescence in situ hybridization (mFISH).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here