Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Please see Chapter 23 for discussion.
Please see Chapter 23 for discussion.
An oncocyte is a large transformed epithelial cell with fine granular eosinophilic cytoplasm. Oncocytomas arises from distal tubules or collecting ducts of the kidney.
3% to 7% of all renal neoplasms.
Present in the sixth to seventh decade of life.
Male predilection (2:1).
3% are bilateral, 5% are multicentric.
75% are asymptomatic and incidentally diagnosed.
Uncommonly presents with flank mass, pain, or hematuria.
Well-defined solid mass with smooth margins and central stellate scar. This is nonspecific; renal cell carcinoma (RCC) with central necrosis can appear the same.
Noncontrast computed tomography (CT): isodense to hyperdense relative to normal renal parenchyma.
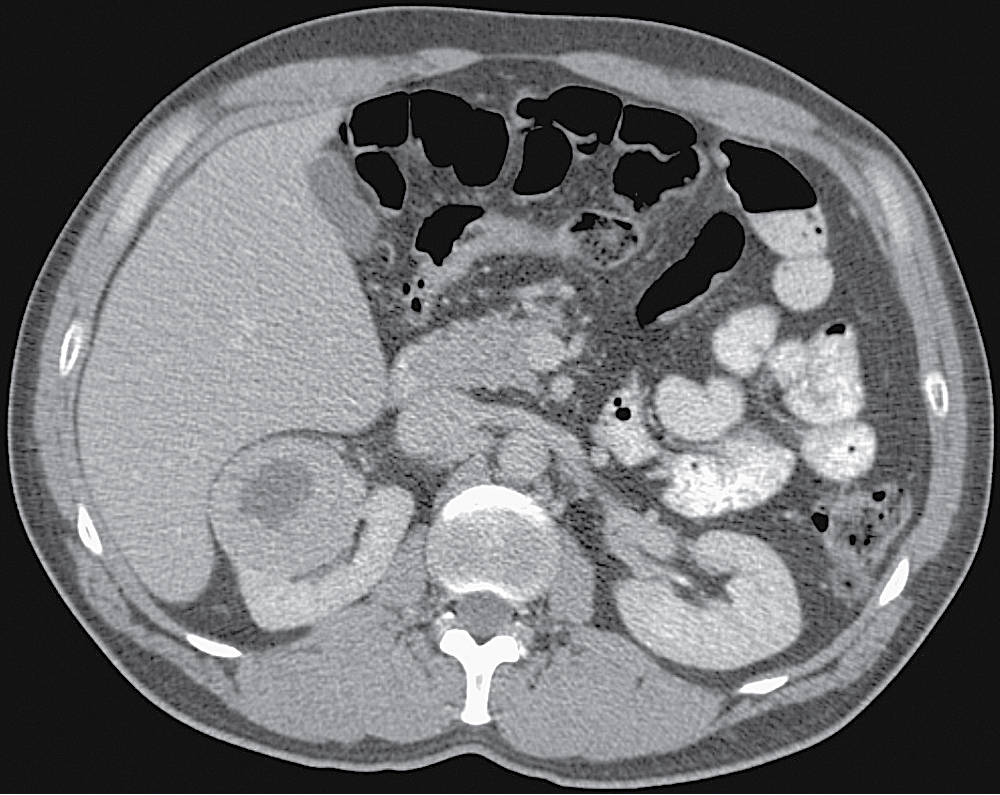
Nephrographic phase: hypodense relative to normal renal parenchyma ( Fig. 24.1 ).
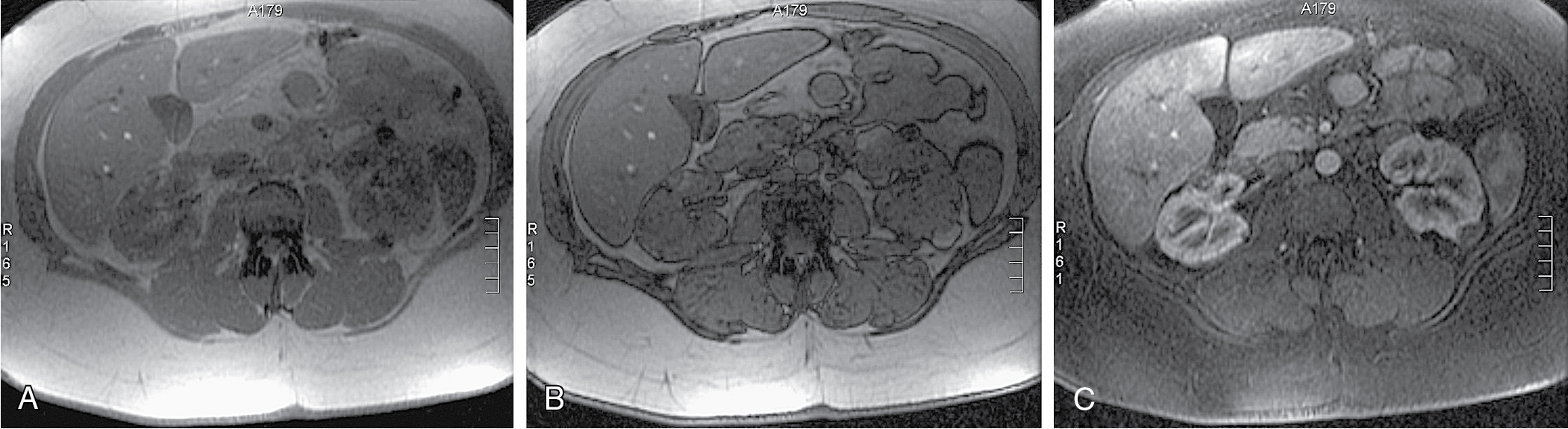
Low signal on T1-weighted image, high signal on T2-weighted image.
Shows homogeneous enhancement with contrast.
Central scar will show low T1 and T2 signal, in contrast to central necrosis, which has high T2 signal.
Central scar does not enhance ( Fig. 24.2 ).

Spoke wheel arrangement of vessels.
Homogeneous dense tumor blush.
Sharply demarcated from the kidney.
Main consideration is RCC.
Oncocytoma cannot be reliably distinguished from RCC on cross-sectional imaging. It is also difficult to distinguish from other oncocytic tumors (e.g., chromophobe RCC) on histological evaluation from needle biopsy. Therefore, treatment is typically with partial or total nephrectomy.
Benign renal tumor, belonging to the PEComa family (perivascular epithelioid cell tumors) of mesenchymal tumors. They are composed of varying amounts of blood vessels, fat, and smooth muscle.
Majority are sporadic (80%).
Female predilection (4:1).
20% associated with tuberous sclerosis (more often larger, multiple and bilateral).
Often incidental.
Risk of bleeding is proportional to size of lesion when larger than 4 cm.
Intratumoral or perirenal hemorrhage may cause mass effect leading to flank pain, nausea/vomiting, and fever.
Presence of intratumoral fat (<–20 HU) is nearly pathognomonic for angiomyolipoma (AML) ( Fig. 24.3 ).

About 5% of AMLs have insufficient fat to be recognized on CT. RCC cannot be entirely ruled out in this case.
Hemorrhage may obscure the fatty component of the lesion.
Variable areas of high signal on T1 and T2 depending on fat content.
Use fat suppression techniques and chemical shift imaging to distinguish intratumoral fat. India ink artifact at the mass/kidney interface within the renal mass suggests AML (note, however, that clear cell RCC can also show signal loss on opposed-phase imaging due to intracellular lipid content) ( Fig. 24.4 ).
Well-defined hyperechoic mass ( Fig. 24.5 ).
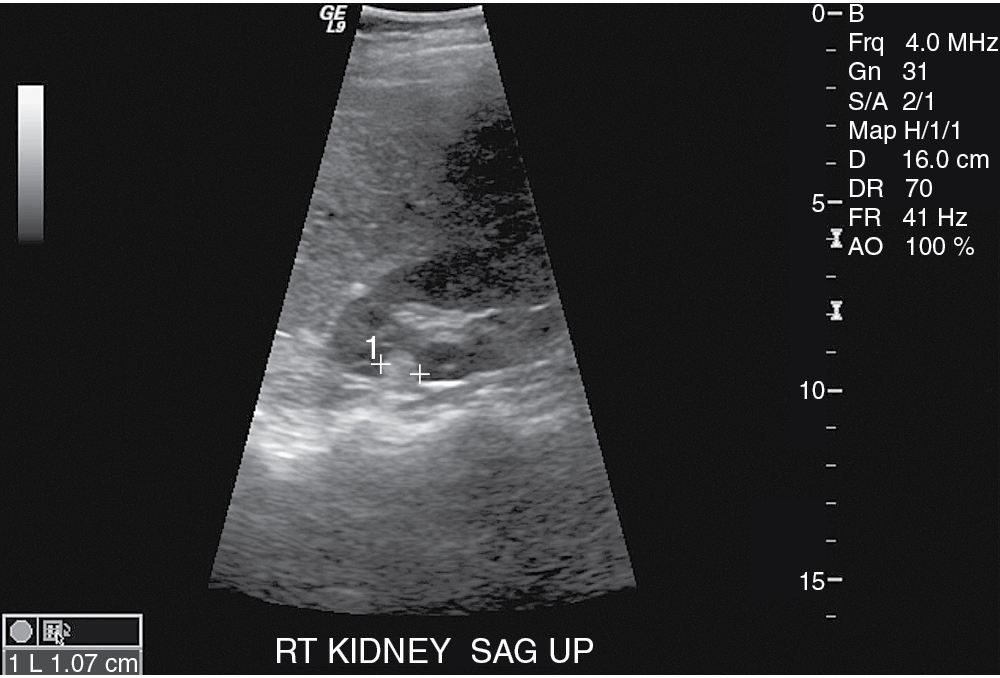
AML is more likely than RCC to have posterior acoustic shadowing.
Demonstrates clusters of saccular microaneurysms or macroaneurysms.
RCC with perirenal fat entrapment or fat necrosis.
Rare: myolipoma, liposarcoma, lipoma, oncocytoma, and Wilms tumor.
If small and asymptomatic, no treatment necessary.
Larger lesions at risk of hemorrhage → prophylactic embolization (>4 cm).
Renin-producing tumors of juxtaglomerular cells usually arising beneath the renal capsule.
Female predilection.
Patients younger than those with essential hypertension.
Hypertension.
Polydipsia.
Polyuria.
Hypokalemia secondary to hyperaldosteronism.
Nonenhanced CT: isodense relative to normal renal parenchyma.
Hypovascular on contrast-enhanced imaging.
Echogenic mass.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here