Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The social determinants of health (SDH) play a critical role in shaping how people access and interact with the healthcare system, subsequently impacting their health outcomes. A growing body of research demonstrates how SDH significantly shapes health outcomes and health disparities. This research is the result of thorough and thoughtful research designs and protocols, which aim to answer high-quality questions and whose results aim to improve health conditions on a population level. Studying the complex interplay between SDH and health is challenging due to its multifactorial nature and requires careful consideration of the chosen study design and outcomes.
When conducting research on addressing the SDH, it is essential to assess the level of the healthcare system at which the intervention or outcome will have an intended impact. At the systemic level, we investigate factors that influence policy and laws with widespread implications. Focusing on the hospital or community level, we are now focusing on social risk factors and, eventually, at the individual level, social needs. A socioecological model is helpful to develop for your research problem to better comprehend all levels of influence for a desired outcome.
As we rethink how to conduct surgical disparities research to improve the science and promote health equity, this chapter will focus on the critical elements of study design and potential outcome metrics to evaluate in research. Of note, the language and terminology used in the health equity space continue to evolve. The authors intend to be as inclusive as possible and use terminology that is accepted practice and consistent with the views of those by which the terms may impact. SDH are inherently neutral—they are not dependent on a direction—but define an association between an exposure and outcome. Research often emphasizes how negative drivers of SDH are associated with worse disparities in outcomes. However, when a population's needs are adequately met, SDH surgical research can shift social and societal conditions in a positive direction to improve subsequent downstream health outcomes. The focus of this chapter is not to be exhaustive, as there are degree programs in Public Health as well as Epidemiology, but rather to highlight essential methods all researchers working to create positive drivers of SDH.
The research question is so critical to study design, outcomes, and meaningful results that it should be briefly emphasized again. However, the previous chapter went into extensive detail on asking high-quality, impactful, theoretically informed SDH research questions. The research question is so foundational to the study design and designated outcomes that this chapter should always be read with others but only after researchers have read the previous chapter. SDH research questions are unique among surgical questions because they are framed within the context of community-level factors and public policy. Given this framing, the community of interest should be involved in asking surgical public health questions to involve all relevant stakeholders and ensure significance to the research population (see Community-Based Participatory Research section). This involvement can occur through a diverse research team, including diversity based on sociodemographic variables (race, ethnicity, gender, age, income, etc.) but also topic expertise. For example, a study on SDH and vascular surgery may include vascular surgeons. Still, researchers should also consider asking cardiologists, vascular medicine specialists, primary care physicians, nephrologists (if concerning vascular access for dialysis), and even vascular surgery patients. For example, a study developing a patient or surgeon survey should include psychometricians and pilot samples of patients/surgeons with subsequent interviews/focus groups. Like building a team for a survey, researchers should consider how they build their SDH research team. Including people with diverse perspectives can help develop specific and meaningful questions and solutions. Similarly, developing and supporting a diverse workforce is instrumental in promoting more equitable study design, as this workforce may have the lived experience to create meaningful questions.
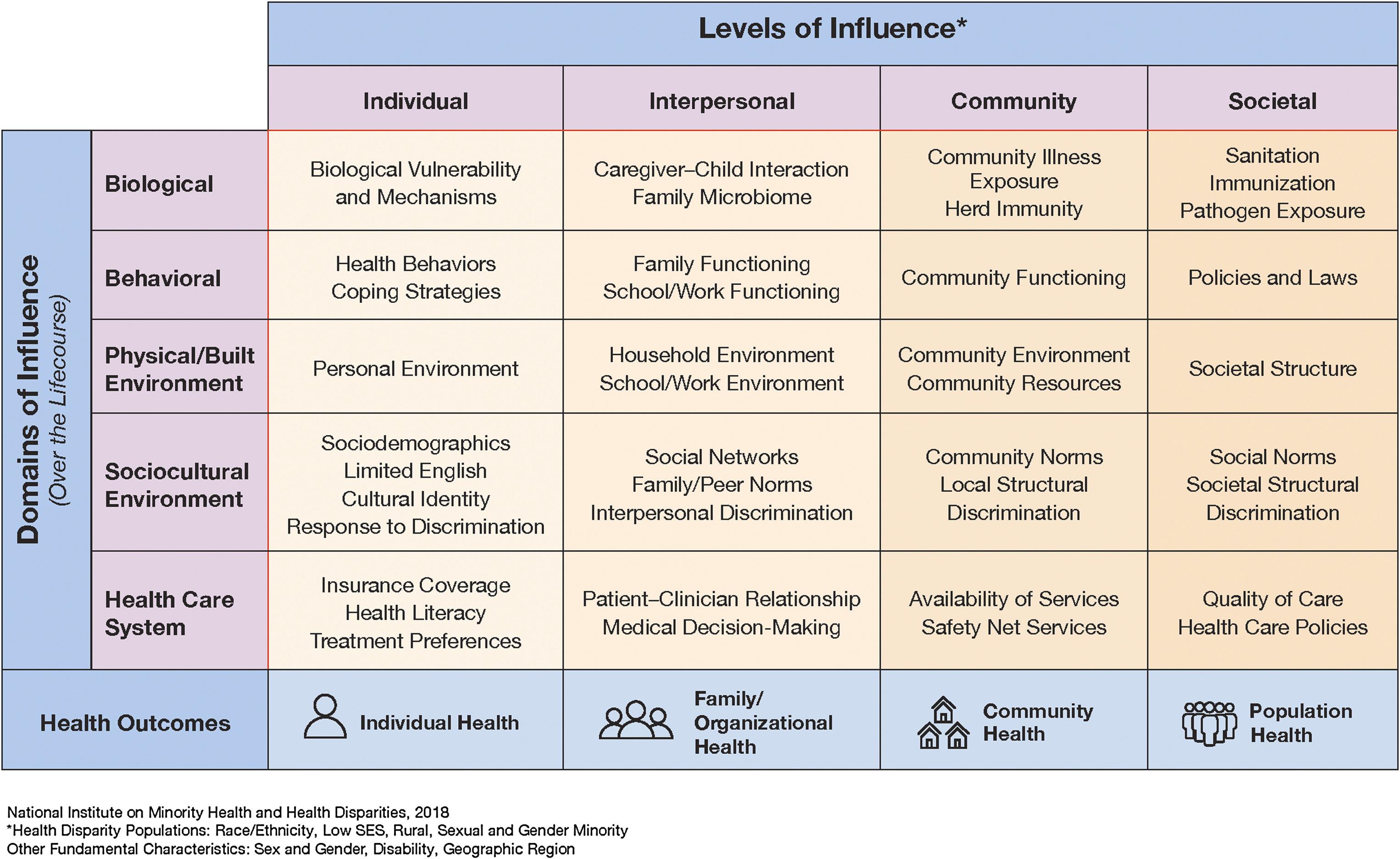
The National Institute on Minority Health and Health Disparities (NIMHHD) Research Framework ( Fig. 14.1 ) has an exemplar template for developing and expanding research questions focused on SDH. This framework highlights five domains of disparities research: behavioral, sociocultural environment, healthcare system, physical/built environment, and biological. Each of these domains is then considered on multiple levels of influence: individual, interpersonal, community, and societal. This resource can assist a researcher in evaluating potential levels and/or domains of influence when creating a research question, selecting a study population, and utilizing subsequent confounders/exposures.
Defining the population is integral to the overall study because it informs the research's results, impact, and generalizability. The more purposefully diverse and inclusive research population will improve broad generalizability and impact. Admittedly, there are restraints in diverse inclusion due to research funding and the specific availability of special populations within the local communities, which can be discussed in a study's limitations. However, SDH research must reflect the community of interest with equity in mind. A thoughtful selection of study participants is necessary to ensure that diverse perspectives are included. However, care should be taken when studying vulnerable populations, including children, individuals with disabilities, and those who are incarcerated. Funders (National Institutes of Health, private foundations, societal groups, etc.) also require consideration be made for special populations with thorough explanations for their inclusion/exclusion. Therefore, researchers should consider who is included and who is also consciously or subconsciously excluded due to implicit or explicit biases.
Diverse populations can help identify disparities and develop interventions toward health equity. There are common specific populations that need to be factored into study designs aimed at reducing health disparities due to SDH ( Table 14.1 ). Caution should be taken when discussing such populations as identification with the below-mentioned groups does not convey homogenous experiences or beliefs. , Furthermore, it is essential to recognize that within health-related research, race/ethnicity most likely serves as a proxy for racism (internalized, interpersonal, institutional, structural) and discrimination. Race is a crude proxy for the factors that mediate disparities in health outcomes.
| Racial/Ethnic | |
| Black/African American | Using the 2012–16 National Inpatient Sample, the authors found that compared with white women, black women who had mastectomy had longer length of stay, greater odds of complications, and were more likely to have autologous reconstruction. |
| Hispanic/Latino/Latinx | Using HCUP State Inpatient Database in New Jersey, authors found that among 22,971 hispanic patients undergoing emergency general surgery operations, there were statistically significant differences in perioperative outcomes between hispanic subgroups (central/South American, Puerto Rican, Mexican, and Cuban) . |
| Asian | Using the 2004–18 surveillance, epidemiology, and End Results database, researchers found multiple significant sociodemographic and medical risk factors for increased specific mortality of prostate cancer among Asian American men. |
| Indigenous | Given the low rates of cancer screening among American Indian men, these authors describe the Community-Based Participatory Research process and assessment of cancer screening while using text messaging among Hopi men. Researchers found that text messaging was more easily available than patient portals due to ease of access as well as decreased reliable internet. |
| Sex and Gender | |
| LGBTQ+ | Eleven patient-reported outcomes from the Patient-Reported Outcomes Measurement Information system (PROMIS) were administered to evaluate psychosocial outcomes after gender-affirming facial feminization surgery with reported improvement in anxiety, anger depression, and isolation. |
| Women | Among 1.8 million patients in the Nationwide Inpatient Sample, researchers found a preference of endovascular over surgical revascularization among women, who were older and more likely to have critical limb ischemia versus intermittent claudication. They also found women are at increased risk of 30-day mortality and early complications. |
| Geography | |
| Rural | This study demonstrated that rural geriatric surgical patients in New Hampshire are likely to receive care outside of their home county or be transferred, without differences in cost of care of unadjusted mortality. The researchers suggested further research into the specific reasons for transfers and which patients may benefit from remaining close to home. |
| Immigrants, refugees, and asylees | This study interviewed 35 women who had immigrated from east Asia regarding perceptions of breast reconstruction. Themes included lack of information regarding reconstruction, desire to be cancer free and done with treatment, and perceptions of plastic surgery. |
| Unhoused | Homeless patients living in Medicaid expansion states had lower rates of discharge against medical advice and decreased total index hospital charges after admissions for emergency general surgery. |
| Age | |
| Elderly | Mortality after major surgery was assessed among community-living older adults in the United States through the National Health and Aging Trends study data. Researchers found that 1-year morality rate was 12.4%, but three times higher for nonelective surgeries than elective surgeries, which can help guide patient discussions/expectations. |
| Children | This study explored glycemic control in severely obese adolescents with type 2 diabetes who underwent medical therapy or surgical therapy, finding that compared with medical therapy, surgical treatment was associated with better glycemic control and reduced weight. |
| Other | |
| Incarcerated or previously incarcerated | This article discusses the frequency of emergency general surgery or trauma visits within an incarcerated population across 12 centers. Patients were noted to have low follow-up after hospitalization, which was coupled with high rates of assault, mental health and substance use disorders, and self-harm. |
| Adults with disabilities | This study compared rates of kidney transplant and its outcomes among adults with and without intellectual and developmental disabilities (IDDs). Adults with IDD were half as likely to be evaluated and more than half as likely to receive a kidney transplant despite similar outcomes. |
| Veterans | Veterans who underwent total hip and knee arthroplasties at Veteran Affairs (VAs) health system had increased comorbidities overall compared with the general population (American college of Surgeons database matched), yet even after adjustment VA patients had increased postoperative complications, length of stay, and readmissions. |
Producing equitable research requires collecting data for these specific populations; you don't know what you don't measure. When using identity data, it should ideally be explicitly collected as self-identified. To implement health system change and enact new policies to promote equitable care, surgical researchers must recognize that this variable lacks construct validity and should seek to create targeted interventions that address true causes of disparities including, most notably, racism.
Community-based participatory research (CBPR) is a research approach that relies on active community member participation in tandem with research teams throughout the entirety of the research process. CBPR enables community partners to provide insight into the unique landscape of local health systems and is intended to build equitable relationships with researchers. Moreover, CBPR ensures researchers are studying access and outcome measures important to the community and provides opportunities to analyze healthcare structures and processes, which in turn leads to the identification of patient-centered solutions. CBPR is not a singular method or research design but rather an approach that can be applied to multiple types of methods and research designs. Incorporating community members can take various forms, including community advisory boards (CABs), patient and family advocacy councils (PFACs), and partnerships with community organizations.
CBPR has been demonstrated to address healthcare disparities in decision-making and quality of care. , CBPR has recently been utilized to reduce socioeconomic status disparities in kidney transplantation access (RaDIANT protocol) and breast cancer decision-making (NCT03136367). , Researchers should consider adding community members to the authorship list and allow them to critically review/edit manuscripts/publications.
To have a study population that will appropriately address the research needs at hand, participants must be recruited. There are a variety of mechanisms by which to recruit for study participation, including posters, video and radio advertisements, social media postings, mobile apps, handouts, emails, and brochures. Recruitment materials should be first and foremost approved by a local Institutional Review Board, but also culturally tailored with the help of community members (PFAC or CAB) to ensure that it effectively conveys the study's goal. Additionally, researchers should ensure that materials are translated appropriately or accessible for those with limited sensory capacity. Although over 8.7% of the US population has limited English proficiency (LEP), many research projects exclude patients with LEP due to systemic problems in communicating appropriately with patients with LEP. These challenges, however, should never prevent researchers from attempting to recruit patients with LEP; if a researcher actively excludes 8.7% of the US population, this significantly limits the generalizability of public health studies. Beyond language considerations, specific plans regarding time away from work, transportation, childcare, caregiving, and translation needs should be made ahead of time to decrease the participant burden.
Unfortunately, within the United States and medicine overall, certain populations have been taken advantage of for research purposes. Infamous examples include the Tuskegee Syphilis Study, Henrietta Lacks' biologic content usage, and forced sterilization of Black women. Understandably, distrust in the medical system persists in part due to this legacy. More recently, there has been distrust related to the COVID-19 global pandemic that stems from rooted racism within healthcare. To effectively recruit participants, the trustworthiness of the researchers and institution is paramount; PFACs and CABs may be particularly helpful surrounding systemic/institutional distrust.
The lived environment contextualizes the experiences of communities and patients and provides critical insight into health access and outcomes. The lived environment encompasses both human-made and natural environments where community members live that impact their health and well-being. Environmental determinants of health can be divided into built (human-made environment such as walkability of a town, food deserts, green spaces, proximity to highways, proximity to hospitals, housing, transportation) and natural (not purposefully built by humans such as air quality, water quality, local pollutants, climate change, extreme weather). There are also distinct needs for urban and rural communities that should be defined and considered when developing a study.
Environmental conditions may be challenging to quantify, but different indices have tried to compile aspects of the neighborhood environment to provide context to healthcare outcomes. There are multiple publicly available sociodemographic indices available online ( Table 14.2 ). One study from 2023 compared neighborhood deprivation index, social deprivation index (SDI), area deprivation index, and social vulnerability index on transplant populations, finding that “the choice of deprivation index affects the applicability of research findings across studies examining the relationship between social risk and clinical outcomes.”
| Index | Data source | Variables (Number) | Measurement Area | Example Surgical Study |
|---|---|---|---|---|
| Distressed Communities Index (DCI) |
ACS 5-Y | 7 | ZIP | Researchers highlight how DCI improves American college of Surgeon's NSQIP risk-adjustment to predict perioperative outcomes and cost. |
| Area Deprivation Index (ADI) |
ACS 5-Y | 17 | Census block | Lower ADI was associated with improved outcomes across five major common surgeries. However, researchers found ADI disproportionately favored white patients. |
| Social Vulnerability Index (SVI) |
US Census Data | 16 | Census tract | Researchers found that increased SVI was associated with decreased “textbook” outcomes after hepatopancreatic surgery. |
| Social Deprivation Index (SDI) |
ACS 5-Y | 7 | County, census tract, ZCTA, and PCSA | Researchers adjusted for sociodemographic factors by using the SDI, finding black non-hispanic patients were more likely to undergo emergency surgery than white non-hispanic patients with colorectal cancer. |
| Neighborhood Deprivation Index (NDI) | UW School of Medicine and Public Health via ACS | 13 | 9-digit ZIP | In a prospective longitudinal cohort study of bariatric surgery patients, researchers found that NDI level was not associated with differences in weight loss at 1 or 3 years. |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here