Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Sleep, with its counterpart of wakefulness, is a highly complex and intricately regulated neurobiologic system that both influences and is influenced by all physiologic systems in the body, as well as by the environment and sociocultural practices. The concept of sleep regulation is based on what is usually referred to as the “2-process model” because it requires the simultaneous operation of 2 basic, highly coupled processes that govern sleep and wakefulness. The homeostatic process (“Process S”), regulates the length and depth of sleep and is thought to be related to the accumulation of adenosine and other sleep-promoting chemicals (“somnogens”), such as cytokines, during prolonged periods of wakefulness. This sleep pressure appears to build more quickly in infants and young children, thus limiting the duration that wakefulness can be sustained during the day and necessitating periods of daytime sleep (i.e., naps). The endogenous circadian rhythms (“Process C”) influence the internal organization of sleep and the timing and duration of daily sleep–wake cycles and govern predictable patterns of alertness throughout the 24 hr day.
The “master circadian clock” that controls sleep–wake patterns, of which melatonin secretion is the principal biomarker, is located in the suprachiasmatic nucleus in the ventral hypothalamus. In addition, “circadian clocks” are present in virtually every cell in the body, which in turn govern the timing of multiple other physiologic systems (e.g., cardiovascular reactivity, hormone levels, renal and pulmonary functions). Because the human circadian clock is slightly longer than 24 hr, intrinsic circadian rhythms must be synchronized or “entrained” to the 24 hr day cycle by environmental cues called zeitgebers. The dark–light cycle is the most powerful of the zeitgebers; light signals are transmitted to the suprachiasmatic nucleus via the circadian photoreceptor system within the retina (functionally and anatomically separate from the visual system), which switch the pineal gland's production of the hormone melatonin off (light) or on (dark). Circadian rhythms are also synchronized by other external time cues, such as timing of meals and alarm clocks.
Sleep propensity, the relative level of sleepiness or alertness experienced at any given time during a 24 hr period, is partially determined by the homeostatic sleep drive , which in turn depends on the duration and quality of previous sleep and the amount of time awake since the last sleep period. Interacting with this sleep homeostat is the 24 hr cyclic pattern or rhythm characterized by clock-dependent periods of maximum sleepiness ( circadian troughs ) and maximum alertness ( circadian nadirs ). There are two periods of maximum sleepiness, one in the late afternoon (approximately 3:00-5:00 pm ) and one toward the end of the night (around 3:00-5:00 am ), and two periods of maximum alertness, one in mid-morning and one in the evening just before the onset of natural sleep, the so-called forbidden zone or second-wind phenomenon, which allows for the maintenance of wakefulness in the face of accumulated sleep drive.
There are significant health, safety, and performance consequences of failure to meet basic sleep needs, termed insufficient/inadequate sleep or sleep loss . Sufficient sleep is a biologic imperative, necessary for optimal brain and body functioning. Slow-wave sleep (SWS) (i.e., N3, delta, or deep sleep) appears to be the most restorative form of sleep; it is entered relatively quickly after sleep onset, is preserved in the face of reduced total sleep time, and increases (rebounds) after a night of restricted sleep. These restorative properties of sleep may be linked to the “glymphatic system,” which increases clearance of metabolic waste products, including β-amyloid, produced by neural activity in the awake brain. Rapid eye movement (REM) sleep (stage R or “dream” sleep) appears to be involved in numerous important brain processes, including completion of vital cognitive functions (e.g., consolidation of memory), promoting the plasticity of the central nervous system (CNS), and protecting the brain from injury. Sufficient amounts of these sleep stages are necessary for optimal cognitive functioning and emotional and behavioral self-regulation.
Partial sleep loss (i.e., sleep restriction) on a chronic basis accumulates in a sleep debt and over several days produces deficits equivalent to those seen under conditions of 1 night of total sleep deprivation. If the sleep debt becomes large enough and is not voluntarily repaid by obtaining sufficient recovery sleep, the body may respond by overriding voluntary control of wakefulness. This results in periods of decreased alertness, dozing off, and unplanned napping, recognized as excessive daytime sleepiness. The sleep-restricted individual may also experience very brief (several seconds) repeated daytime microsleeps, of which the individual may be completely unaware, but which nonetheless may result in significant lapses in attention and vigilance. There is also a relationship between the amount of sleep restriction and performance on cognitive tasks, particularly those requiring sustained attention and higher-level cognitive skills ( executive functions ; see Chapter 48 ), with a decay in performance correlating with declines in sleep amounts.
It has also been increasingly recognized that what may be globally described as “deficient” sleep involves alterations in both amount and timing of sleep. Misalignment of intrinsic circadian rhythms with extrinsic societal demands, such a shift work and early school start times, is associated with deficits in cognitive function and self-regulation, increased emotional and behavioral problems and risk-taking behaviors, and negative impacts on health, such as increased risk of cardiovascular disease, obesity, and metabolic dysfunction.
Insufficient quantity of sleep, mistimed sleep, and poor-quality sleep in children and adolescents frequently result in excessive daytime sleepiness and decreased daytime alertness levels. Sleepiness in children may be recognizable as drowsiness, yawning, and other classic “sleepy behaviors,” but can also manifest as mood disturbance, including complaints of moodiness, irritability, emotional lability, depression, and anger; fatigue and daytime lethargy, including increased somatic complaints (headaches, muscle aches); cognitive impairment, including problems with memory, attention, concentration, decision-making, and problem solving; daytime behavior problems, including hyperactivity, impulsivity, and noncompliance; and academic problems, including chronic tardiness related to insufficient sleep and school failure resulting from chronic daytime sleepiness.
Sleep disturbances, as well as many characteristics of sleep itself, have some distinctly different features in children from sleep and sleep disorders in adults. Changes in sleep architecture and the evolution of sleep patterns and behaviors reflect the physiologic/chronobiologic, developmental, and social/environmental changes that are occurring across childhood. These trends may be summarized as the gradual assumption of more adult sleep patterns as children mature:
Sleep is the primary activity of the brain during early development; for example, by age 2 yr, the average child has spent 9500 hr (approximately 13 mo) asleep vs 8000 hr awake, and between 2 and 5 yr, the time asleep is equal to the time awake.
There is a gradual decline in the average 24 hr sleep duration from infancy through adolescence, which involves a decrease in both diurnal and nocturnal sleep amounts. The decline in daytime sleep (scheduled napping) results in termination of naps typically by age 5 yr. There is also a gradual continued decrease in nocturnal sleep amounts into late adolescence; however, the typical adolescent still requires 8-10 hr of sleep per night.
There is also a decline in the relative percentage of REM sleep from birth (50% of sleep) through early childhood into adulthood (25–30%), and a similar initial predominance of SWS that peaks in early childhood, drops off abruptly after puberty (40–60% decline), and then further decreases over the life span. This SWS preponderance in early life has clinical significance; for example, the high prevalence of partial arousal parasomnias (sleepwalking and sleep terrors) in preschool and early school-age children is related to the relative increased percentage of SWS in this age-group.
The within-sleep ultradian cycle lengthens from about 50 min in the term infant to 90-110 min in the school-age child. This has clinical significance in that typically a brief arousal or awakening occurs during the night at the termination of each ultradian cycle. As the length of the cycles increase, there is a concomitant decrease in the number of these end-of-cycle arousals (night wakings).
A gradual shift in the circadian sleep–wake rhythm to a delayed (later) sleep onset and offset time, linked to pubertal stage rather than chronological age, begins with pubertal onset in middle childhood and accelerates in early to mid-adolescence. This biologic phenomenon often coincides with environmental factors, which further delay bedtime and advance wake time and result in insufficient sleep duration, including exposure to electronic “screens” (television, computer) in the evening, social networking, academic and extracurricular demands, and early (before 8:30 am ) high school start times.
Increasing irregularity of sleep–wake patterns is typically observed across childhood into adolescence; this is characterized by increasingly larger discrepancies between school night and non–school night bedtimes and wake times, and increased “weekend oversleep” in an attempt to compensate for chronic weekday sleep insufficiency. This phenomenon, often referred to as “social jet lag,” not only fails to adequately address performance deficits associated with insufficient sleep on school nights, but further exacerbates the normal adolescent phase delay and results in additional circadian disruption (analogous to that experienced by shift workers).
Table 31.1 lists normal developmental changes in children's sleep.
| AGE CATEGORY | SLEEP DURATION * AND SLEEP PATTERNS | ADDITIONAL SLEEP ISSUES | SLEEP DISORDERS |
|---|---|---|---|
| Newborn (0-2 mo) | Total sleep: 10-19 hr per 24 hr (average, 13-14.5 hr), may be higher in premature babies Bottle-fed babies generally sleep for longer periods (2-5 hr bouts) than breastfed babies (1-3 hr). Sleep periods are separated by 1-2 hr awake. No established nocturnal-diurnal pattern in 1st few wk; sleep is evenly distributed throughout the day and night, averaging 8.5 hr at night and 5.75 hr during day. |
American Academy of Pediatrics issued a revised recommendation in 2016 advocating against bed-sharing in the 1st yr of life, instead encouraging proximate but separate sleeping surfaces for mother and infant for at least the 1st 6 mo and preferably 1st yr of life. Safe sleep practices for infants:
|
Most sleep issues perceived as problematic at this stage represent a discrepancy between parental expectations and developmentally appropriate sleep behaviors. Newborns who are extremely fussy and persistently difficult to console, as noted by parents, are more likely to have underlying medical issues such as colic, gastroesophageal reflux, and formula intolerance. |
| Infant (2-12 mo) | Recommended sleep duration (4-12 mo) is 12-16 hr (note that there is great individual variability in sleep times during infancy). | Sleep regulation or self-soothing involves the infant's ability to negotiate the sleep–wake transition, both at sleep onset and following normal awakenings throughout the night. The capacity to self-soothe begins to develop in the 1st 12 wk of life and is a reflection of both neurodevelopmental maturation and learning. Sleep consolidation, or “sleeping through the night,” is usually defined by parents as a continuous sleep episode without the need for parental intervention (e.g., feeding, soothing) from the child's bedtime through the early morning. Infants develop the ability to consolidate sleep between 6 wk and 3 mo. |
Behavioral insomnia of childhood; sleep-onset association type Sleep-related rhythmic movements (head banging, body rocking) |
| Toddler (1-2 yr) | Recommended sleep amount is 11-14 hr (including naps). Naps decrease from 2 to 1 nap at average age of 18 mo. |
Cognitive, motor, social, and language developmental issues impact sleep. Nighttime fears develop; transitional objects and bedtime routines are important. |
Behavioral insomnia of childhood, sleep-onset association type Behavioral insomnia of childhood, limit-setting type |
| Preschool (3-5 yr) | Recommended sleep amount is 10-13 hr (including naps). Overall, 26% of 4 yr olds and just 15% of 5 yr olds nap. |
Persistent cosleeping tends to be highly associated with sleep problems in this age-group. | Behavioral insomnia of childhood, limit-setting type |
| Sleep problems may become chronic. | Sleepwalking, sleep terrors, nighttime fears/nightmares, obstructive sleep apnea syndrome | ||
| Middle childhood (6-12 yr) | Recommended sleep amount is 9-12 hr. | School and behavior problems may be related to sleep problems. | Nightmares |
| Media and electronics, such as television, computer, video games, and the Internet, increasingly compete for sleep time. Irregularity of sleep–wake schedules reflects increasing discrepancy between school and non–school night bedtimes and wake times. |
Obstructive sleep apnea syndrome | ||
| Insufficient sleep | |||
| Adolescence (13-18 yr) | Recommended sleep amount is 8-10 hr. Later bedtimes; increased discrepancy between sleep patterns on weekdays and weekends |
Puberty-mediated phase delay (later sleep onset and wake times), relative to sleep-wake cycles in middle childhood Earlier required wake times Environmental competing priorities for sleep |
Insufficient sleep Delayed sleep–wake phase disorder Narcolepsy Restless legs syndrome/periodic limb movement disorder |
* All recommended sleep amounts from Paruthi S, Brooks LJ, D'Ambrosio C, et al: Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. J Clin Sleep Med 12:785–786, 2016.
Childhood sleep problems may be conceptualized as resulting from (1) inadequate duration of sleep for age and sleep needs (insufficient sleep quantity); (2) disruption and fragmentation of sleep (poor sleep quality) as a result of frequent, repetitive, and brief arousals during sleep; and (3) misalignment of sleep–wake timing with circadian rhythms or CNS-mediated hypersomnia (excessive daytime sleepiness and increased sleep needs). Insufficient sleep is usually the result of difficulty initiating ( delayed sleep onset ) or maintaining sleep ( prolonged night wakings ), but, especially in older children and adolescents, may also represent a conscious lifestyle decision to sacrifice sleep in favor of competing priorities, such as homework and social activities. The underlying causes of delayed sleep onset/prolonged night wakings or sleep fragmentation may in turn be related to primarily behavioral factors (e.g., bedtime resistance resulting in shortened sleep duration) or medical causes (e.g., obstructive sleep apnea causing frequent, brief arousals).
Certain pediatric populations are relatively more vulnerable to acute or chronic sleep problems. These include children with medical problems, such as chronic illnesses or pain conditions (e.g., cystic fibrosis, asthma, idiopathic juvenile arthritis) and acute illnesses (e.g., otitis media); children taking stimulants s (e.g., psychostimulants, caffeine), sleep-disrupting medications (e.g., corticosteroids), or daytime-sedating medications (some anticonvulsants, α-agonists); hospitalized children; and children with a variety of psychiatric disorders, including attention-deficit/hyperactivity disorder (ADHD), depression, bipolar disorder, and anxiety disorders. Children with neurodevelopmental disorders such as autism, intellectual disability, blindness, and some chromosomal syndromes (e.g., Smith-Magenis, fragile X) have especially high rates of sleep disturbances for a wide variety of reasons. They may have comorbid medical issues or may be taking sleep-disrupting medications, may be more prone to nocturnal seizures, may be less easily entrained by environmental cues and thus more vulnerable to circadian disruption, and are more likely to have psychiatric and behavioral comorbidities that further predispose them to disrupted sleep.
Insomnia is defined as difficulty initiating and/or maintaining sleep that occurs despite age-appropriate time and opportunity for sleep and results in some degree of impairment in daytime functioning for the child and/or family (ranging from fatigue, irritability, lack of energy, and mild cognitive impairment to effects on mood, school performance, and quality of life). Insomnia may be of a short-term and transient nature (usually related to an acute event) or may be characterized as long-term and chronic. Insomnia is a set of symptoms with many possible etiologies (e.g., pain, medication, medical/psychiatric conditions, learned behaviors). As with many behavioral issues in children, insomnia is often primarily defined by parental concerns rather than by objective criteria, and therefore should be viewed in the context of family (maternal depression, stress), child (temperament, developmental level), and environmental (cultural practices, sleeping space) considerations.
While current terminology ( Diagnostic and Statistical Manual of Mental Disorders, 5th edition, 2015; International Classification of Sleep Disorders, 3rd edition, 2014) groups most types of insomnia in both children and adults under a single category of Chronic Insomnia Disorder, the descriptor of Behavioral Insomnia of Childhood and its subtypes (Sleep Onset Association and Limit Setting) remains a useful construct, particularly for young children (0-5 yr) in clinical practice. One of the most common presentations of insomnia found in infants and toddlers is the sleep-onset association type. In this situation the child learns to fall asleep only under certain conditions or associations, which typically require parental presence, such as being rocked or fed, and does not develop the ability to self-soothe. During the night, when the child experiences the type of brief arousal that normally occurs at the end of an ultradian sleep cycle or awakens for other reasons, the child is not able to get back to sleep without those same associations being present. The infant then “signals” the parent by crying (or coming into the parents' bedroom, if the child is ambulatory) until the necessary associations are provided. The presenting complaint is typically one of prolonged night waking requiring caregiver intervention and resulting in insufficient sleep (for both child and parent).
Management of night wakings should include establishment of a set sleep schedule and bedtime routine and implementation of a behavioral program. The treatment approach typically involves a program of rapid withdrawal (extinction) or more gradual withdrawal (graduated extinction) of parental assistance at sleep onset and during the night. Extinction (“cry it out”) involves putting the child to bed at a designated bedtime, “drowsy but awake,” to maximize sleep propensity and then systematically ignoring any protests by the child until a set time the next morning. Although it has considerable empirical support, extinction is often not an acceptable choice for families. Graduated extinction involves gradually weaning the child from dependence on parental presence; typically, the parent leaves the room at “lights out” and then returns or “checks” periodically at fixed or successively longer intervals during the sleep–wake transition to provide brief reassurance until the child falls asleep. The exact interval between checks is generally determined by the parents' tolerance for crying and the child's temperament. The goal is to allow the infant or child to develop skills in self-soothing during the night, as well as at bedtime. In older infants and young children, the introduction of more appropriate sleep associations that will be readily available to the child during the night (transitional objects, such as a blanket or toy), in addition to positive reinforcement (stickers for remaining in bed), is often beneficial. If the child has become habituated to awaken for nighttime feedings (learned hunger), these feedings should be slowly eliminated. Parents must be consistent in applying behavioral programs to avoid inadvertent, intermittent reinforcement of night wakings. They should also be forewarned that crying behavior often temporarily escalates at the beginning of treatment ( postextinction burst ).
Bedtime problems, including stalling and refusing to go to bed, are more common in preschool-age and older children. This type of insomnia is frequently related to inadequate limit setting and is often the result of parental difficulties in setting limits and managing behavior in general and the inability or unwillingness to set consistent bedtime rules and enforce a regular bedtime. The situation may be exacerbated by the child's oppositional behavior. In some cases the child's resistance at bedtime is the result of an underlying problem in falling asleep that is caused by other factors (medical conditions such as asthma or medication use; a sleep disorder such as restless legs syndrome; anxiety) or a mismatch between the child's intrinsic circadian rhythm (“night owl”) and parental expectations regarding an “appropriate” bedtime.
Successful treatment of limit-setting sleep problems generally involves a combination of parent education regarding appropriate limit setting, decreased parental attention for bedtime-delaying behavior, establishment of bedtime routines, and positive reinforcement (sticker charts) for appropriate behavior at bedtime. Other behavioral management strategies that have empirical support include bedtime fading , or temporarily setting the bedtime closer to the actual sleep-onset time and then gradually advancing the bedtime to an earlier target bedtime. Older children may benefit from being taught relaxation techniques to help themselves fall asleep more readily. Following the principles of healthy sleep practices for children is essential ( Table 31.2 ).
Have a set bedtime and bedtime routine for your child.
Bedtime and wake-up time should be about the same time on school nights and non–school nights. There should not be more than about 1 hr difference from one day to another.
Make the hour before bed shared quiet time. Avoid high-energy activities, such as rough play, and stimulating activities, such as watching television or playing computer games, just before bed.
Don ' t send your child to bed hungry. A light snack (e.g., milk and cookies) before bed is a good idea. Heavy meals within 1 hr or 2 of bedtime, however, may interfere with sleep.
Avoid products containing caffeine for at least several hours before bedtime. These include caffeinated sodas, coffee, tea, and chocolate.
Make sure your child spends time outside every day, whenever possible, and is involved in regular exercise.
Keep your child 's bedroom quiet and dark. A low-level night light is acceptable for children who find completely dark rooms frightening.
Keep your child 's bedroom at a comfortable temperature during the night (<24°C [75°F]).
Don ' t use your child 's bedroom for time-out or punishment.
Keep the television set out of your child 's bedroom. Children can easily develop the bad habit of “needing” the television to fall asleep. It is also much more difficult to control your child's viewing if the set is in the bedroom.
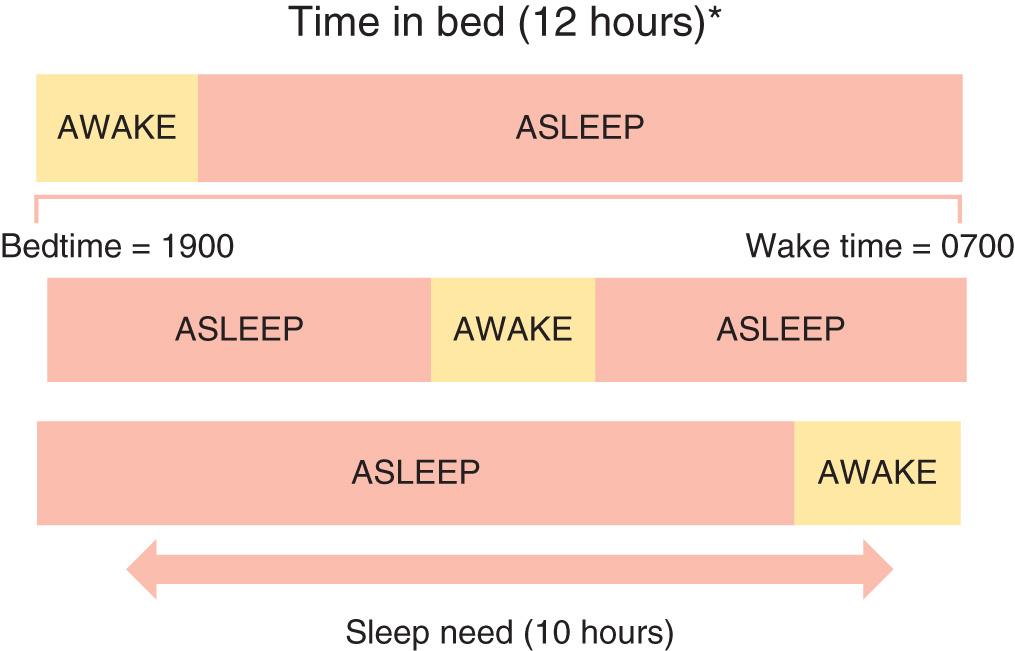
A 3rd type of childhood insomnia is related to a mismatch between parental expectations regarding time in bed and the child's intrinsic sleep needs. If, as illustrated in Fig. 31.1 , a child's typical sleep time is 10 hr but the “sleep window” is set for 12 hr (7 pm to 7 am ), the result is likely to be a prolonged sleep onset of 2 hr, an extended period of wakefulness during the night, or early morning waking (or a combination); these periods are usually characterized by “normal” wakefulness in the child that is not accompanied by excessive distress. This situation is important to recognize because the solution—reducing the time in bed to actual sleep time—is typically simple and effective.
Another form of insomnia that is more common in older children and adolescents is often referred to as psychophysiologic, primary, or learned insomnia. Primary insomnia occurs mainly in adolescents and is characterized by a combination of learned sleep-preventing associations and heightened physiologic arousal resulting in a complaint of sleeplessness and decreased daytime functioning. A hallmark of primary insomnia is excessive worry about sleep and an exaggerated concern of the potential daytime consequences. The physiologic arousal can be in the form of cognitive hypervigilance , such as “racing” thoughts; in many individuals with insomnia, an increased baseline level of arousal is further intensified by this secondary anxiety about sleeplessness. Treatment usually involves educating the adolescent about the principles of healthy sleep practices ( Table 31.3 ), institution of a consistent sleep–wake schedule, avoidance of daytime napping, instructions to use the bed for sleep only and to get out of bed if unable to fall asleep ( stimulus control ), restricting time in bed to the actual time asleep ( sleep restriction ), addressing maladaptive cognitions about sleep, and teaching relaxation techniques to reduce anxiety.
Wake up and go to bed at about the same time every night. Bedtime and wake-up time should not differ from school to non–school nights by more than approximately 1 hr.
Avoid sleeping in on weekends to “catch up” on sleep. This makes it more likely that you will have problems falling asleep.
If you take naps , they should be short (no more than 1 hr) and scheduled in the early to mid-afternoon . However, if you have a problem with falling asleep at night, napping during the day may make it worse and should be avoided.
Spend time outside every day. Exposure to sunlight helps to keep your body's internal clock on track.
Exercise regularly. Exercise may help you fall asleep and sleep more deeply.
Use your bed for sleeping only. Don't study, read, listen to music, or watch television on your bed.
Make the 30-60 minutes before bedtime a quiet or wind-down time . Relaxing, calm, enjoyable activities, such as reading a book or listening to calm music, help your body and mind slow down enough to let you get to sleep. Don't study, watch exciting/scary movies, exercise, or get involved in “energizing” activities just before bed.
Eat regular meals, and don ' t go to bed hungry . A light snack before bed is a good idea; eating a full meal within 1 hr before bed is not.
Avoid eating or drinking products containing caffeine from dinnertime to bedtime. These include caffeinated sodas, coffee, tea, and chocolate.
Do not use alcohol. Alcohol disrupts sleep and may cause you to awaken throughout the night.
Smoking (e.g., cigarettes) disturbs sleep. Although you should not smoke at all, if you do, do not smoke at least 2 hr before bed .
Do not use sleeping pills, melatonin, or other nonprescription sleep aids to help you sleep unless specifically recommended by your doctor. These can be dangerous, and the sleep problems often return when you stop taking the medicine.
Behavioral treatments for insomnia, even in young children, appear to be highly effective and well tolerated. Several studies have failed to demonstrate long-term negative effects of behavioral strategies such as “sleep training” on parent–child relationships and attachment, psychosocial-emotional functioning, and chronic stress. In general, hypnotic medications or supplements such as melatonin are infrequently needed as an adjunct to behavioral therapy to treat insomnia in typically developing and healthy children.
Sleep-related breathing disorder (SRBD ) in children encompasses a broad spectrum of respiratory disorders that occur exclusively in sleep or that are exacerbated by sleep, including primary snoring and upper airway resistance syndrome, as well as apnea of prematurity (see Chapter 122.2 ) and central apnea (see Chapter 446.2 ). Obstructive sleep apnea syndrome (OSAS) , the most important clinical entity within the SRBD spectrum, is characterized by repeated episodes of prolonged upper airway obstruction during sleep despite continued or increased respiratory effort, resulting in complete ( apnea ) or partial ( hypopnea ; ≥30% reduction in airflow accompanied by ≥3% O 2 desaturation and/or arousal) cessation of airflow at the nose and/or mouth, as well as in disrupted sleep. Both intermittent hypoxia and the multiple arousals resulting from these obstructive events likely contribute to significant metabolic, cardiovascular, and neurocognitive-neurobehavioral morbidity.
Primary snoring is defined as snoring without associated ventilatory abnormalities on overnight polysomnogram (e.g., apneas or hypopneas, hypoxemia, hypercapnia) or respiratory-related arousals and is a manifestation of the vibrations of the oropharyngeal soft tissue walls that occur when an individual attempts to breathe against increased upper airway resistance during sleep. Although generally considered nonpathologic, primary snoring in children may still be associated with subtle breathing abnormalities during sleep, including evidence of increased respiratory effort, which in turn may be associated with adverse neurodevelopmental outcomes.
OSAS results from an anatomically or functionally narrowed upper airway; this typically involves some combination of decreased upper airway patency (upper airway obstruction and/or decreased upper airway diameter), increased upper airway collapsibility (reduced pharyngeal muscle tone), and decreased drive to breathe in the face of reduced upper airway patency (reduced central ventilatory drive) ( Table 31.4 ). Upper airway obstruction varies in degree and level (i.e., nose, nasopharynx/oropharynx, hypopharynx) and is most frequently caused by adenotonsillar hypertrophy, although tonsillar size does not necessarily correlate with degree of obstruction, especially in older children. Other causes of airway obstruction include allergies associated with chronic rhinitis or nasal obstruction; craniofacial abnormalities, including hypoplasia or displacement of the maxilla and mandible; gastroesophageal reflux with resulting pharyngeal reactive edema (see Chapter 349 ); nasal septal deviation ( Chapter 404 ); and velopharyngeal flap cleft palate repair. Reduced upper airway tone may result from neuromuscular diseases, including hypotonic cerebral palsy and muscular dystrophies (see Chapter 627 ), or hypothyroidism ( Chapter 581 ). Reduced central ventilatory drive may be present in some children with Arnold-Chiari malformation (see Chapter 446 ); rapid-onset obesity with hypothalamic dysfunction, hypoventilation, and autonomic dysregulation ( Chapter 60.1 ); and meningomyelocele ( Chapter 609.4 ). In other situations the etiology is mixed; individuals with Down syndrome (see Chapter 98.2 ), because of their facial anatomy, hypotonia, macroglossia, and central adiposity, as well as the increased incidence of hypothyroidism, are at particularly high risk for OSAS, with some estimates of prevalence as high as 70%.
Anterior nasal stenosis
Choanal stenosis/atresia
Deviated nasal septum
Seasonal or perennial rhinitis
Nasal polyps, foreign body, hematoma, mass lesion
Adenotonsillar hypertrophy
Macroglossia
Cystic hygroma
Velopharyngeal flap repair
Cleft palate repair
Pharyngeal mass lesion
Micrognathia/retrognathia
Midface hypoplasia (e.g., trisomy 21, Crouzon disease, Apert syndrome)
Mandibular hypoplasia (Pierre Robin, Treacher Collins, Cornelia de Lange syndromes)
Craniofacial trauma
Skeletal and storage diseases
Achondroplasia
Storage diseases (e.g., glycogen; Hunter, Hurler syndromes)
Although many children with OSAS are of normal weight, an increasingly large percentage are overweight or obese, and many of these children are school-age or younger (see Chapter 60 ). There is a significant correlation between weight and SRBD (e.g., habitual snoring, OSAS, sleep-related hypoventilation). Although adenotonsillar hypertrophy also plays an important etiologic role in overweight/obese children with OSAS, mechanical factors related to an increase in the amount of adipose tissue in the throat (pharyngeal fat pads), neck (increased neck circumference), and chest wall and abdomen can increase upper airway resistance, worsen gas exchange, and increase the work of breathing, particularly in the supine position and during REM sleep. A component of blunted central ventilatory drive in response to hypoxia/hypercapnia and hypoventilation may occur as well (see Chapter 446.3 ), particularly in children with morbid or syndrome-based (e.g., Prader-Willi) obesity. Overweight and obese children and adolescents are at particularly high risk for metabolic and cardiovascular complications of SRBD, such as insulin resistance and systemic hypertension. Morbidly obese children are also at increased risk for postoperative complications as well as residual OSAS after adenotonsillectomy.
Overall prevalence of parent-reported snoring in the pediatric population is approximately 8%; “always” snoring is reported in 1.5–6%, and “often” snoring in 3–15%. When defined by parent-reported symptoms, the prevalence of OSAS is 4–11%. The prevalence of pediatric OSAS as documented by overnight sleep studies using ventilatory monitoring procedures (e.g., in-lab polysomnography, home studies) is 1–4% overall, with a reported range of 0.1–13%. Prevalence is also affected by the demographic characteristics such as age (increased prevalence between 2 and 8 yr), gender (more common in boys, especially after puberty), race/ethnicity (increased prevalence in African American and Asian children), history of prematurity, and family history of OSAS.
The upregulation of inflammatory pathways, as indicated by an increase in peripheral markers of inflammation (e.g., C-reactive protein, interleukins), appears to be linked to metabolic dysfunction (e.g., insulin resistance, dyslipidemia, alterations in neurohormone levels such as leptin) in both obese and nonobese children with OSAS. Systemic inflammation and arousal-mediated increases in sympathetic autonomic nervous system activity with altered vasomotor tone may be key contributors to increased cardiovascular risk due to alterations in vascular endothelium in both adults and children with OSA. Other potential mechanisms that may mediate cardiovascular sequelae in adults and children with OSA include elevated systemic blood pressure and ventricular dysfunction. Mechanical stress on the upper airway induced by chronic snoring may also result in both local mucosal inflammation of adenotonsillar tissues and subsequent upregulation of inflammatory molecules, most notably leukotrienes.
One of the primary mechanisms by which OSAS is believed to exert negative influences on cognitive function appears to involve repeated episodic arousals from sleep leading to sleep fragmentation and sleepiness. Equally important, intermittent hypoxia may lead directly to systemic inflammatory vascular changes in the brain. Levels of inflammatory markers such as C-reactive protein and interleukin-6 are elevated in children with OSAS and are also associated with cognitive dysfunction.
The clinical manifestations of OSAS may be divided into sleep-related and daytime symptoms. The most common nocturnal manifestations of OSAS in children and adolescents are loud, frequent, and disruptive snoring; breathing pauses; choking or gasping arousals; restless sleep; and nocturnal diaphoresis. Many children who snore do not have OSAS, but few children with OSAS do not snore (caregivers may not be aware of snoring in older children and adolescents). Children, like adults, tend to have more frequent and more severe obstructive events in REM sleep and when sleeping in the supine position. Children with OSAS may adopt unusual sleeping positions, keeping their necks hyperextended to maintain airway patency. Frequent arousals associated with obstruction may result in nocturnal awakenings but are more likely to cause fragmented sleep.
Daytime symptoms of OSAS include mouth breathing and dry mouth, chronic nasal congestion or rhinorrhea, hyponasal speech, morning headaches, difficulty swallowing, and poor appetite. Children with OSAS may have secondary enuresis, postulated to result from the disruption of the normal nocturnal pattern of atrial natriuretic peptide secretion by changes in intrathoracic pressure associated with OSAS. Partial arousal parasomnias (sleepwalking and sleep terrors) may occur more frequently in children with OSAS, related to the frequent associated arousals and an increased percentage of SWS.
One of the most important but frequently overlooked sequelae of OSAS in children is the effect on mood, behavior, learning, and academic functioning. The neurobehavioral consequences of OSAS in children include daytime sleepiness with drowsiness, difficulty in morning waking, and unplanned napping or dozing off during activities, although evidence of frank hypersomnolence tends to be less common in children compared to adults with OSA (except in very obese children or those with severe disease). Mood changes include increased irritability, mood instability and emotional dysregulation, low frustration tolerance, and depression or anxiety. Behavioral issues include both “internalizing” (i.e., increased somatic complaints and social withdrawal) and “externalizing” behaviors, including aggression, impulsivity, hyperactivity, oppositional behavior, and conduct problems. There is substantial overlap between the clinical impairments associated with OSAS and the diagnostic criteria for ADHD, including inattention, poor concentration, and distractibility (see Chapter 49 ).
Many of the studies that have looked at changes in behavior and neuropsychologic functioning in children after treatment (usually adenotonsillectomy) for OSAS have largely documented significant improvement in outcomes, both short term and long term, including daytime sleepiness, mood, behavior, academics, and quality of life. However, most studies failed to find a dose-dependent relationship between OSAS in children and specific neurobehavioral-neurocognitive deficits, suggesting that other factors may influence neurocognitive outcomes, including individual genetic susceptibility, racial/ethnic background, environmental influences (e.g., passive smoking exposure), and comorbid conditions, such as obesity, shortened sleep duration, and other sleep disorders.
The 2012 revised American Academy of Pediatrics clinical practice guidelines provide excellent information for the evaluation and management of uncomplicated childhood OSAS ( Table 31.5 ). No physical examination findings are truly pathognomonic for OSAS, and most healthy children with OSAS appear normal; however, certain physical examination findings may suggest OSAS. Growth parameters may be abnormal (obesity, or less frequently, failure to thrive), and there may be evidence of chronic nasal obstruction (hyponasal speech, mouth breathing, septal deviation, “adenoidal facies”) as well as signs of atopic disease (i.e., “allergic shiners”). Oropharyngeal examination may reveal enlarged tonsils, excess soft tissue in the posterior pharynx, and a narrowed posterior pharyngeal space, as well as dental features consistent with obstruction (e.g., teeth crowding, narrow palate, short frenulum). Any abnormalities of head position, such as forward head posture, and facial structure, such as retrognathia, micrognathia, and midfacial hypoplasia, best appreciated by inspection of the lateral facial profile, increase the likelihood of OSAS and should be noted. In severe cases the child may have evidence of pulmonary hypertension, right-sided heart failure, and cor pulmonale; systemic hypertension may occur, especially in obese children.
As part of routine health maintenance visits, clinicians should inquire whether the child or adolescent snores. If the answer is affirmative or if a child or adolescent presents with signs or symptoms of OSAS, clinicians should perform a more focused evaluation. (Evidence Quality: Grade B; Recommendation Strength: Recommendation.)
If a child or adolescent snores on a regular basis and has any of the complaints or findings of OSAS, clinicians should either (1) obtain a polysomnogram (Evidence Quality: Grade A; Recommendation Strength: Recommendation) or (2) refer the patient to a sleep specialist or otolaryngologist for a more extensive evaluation (Evidence Quality: Grade D; Recommendation Strength: Option.)
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here