Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The glenohumeral joint is the most mobile joint in the body with large arcs of motion in multiple distinct planes. Owing to limited osseous contribution to stability, the shoulder relies on the precise balance of a number of different soft-tissue stabilizers, including the deltoid, the biceps brachii, the scapular stabilizers, the rotator cuff musculature, the glenoid labrum, and associated glenohumeral ligaments. Sports, particularly overhead throwing, can subject the shoulder to a wide variety of forces that can put each of these structures at risk. A spectrum of injuries to the superior labrum, often described as SLAP (superior labrum anterior and posterior) lesions, have been well described. Although nonoperative management can and should be attempted, SLAP lesions may ultimately require surgical intervention.
Since its initial description, numerous techniques have been proposed for repair of SLAP lesions. In particular, a variety of implantable anchor devices have been used, progressing from metal through tack to knot-tied to knotless. In spite of those variations, the essential components of the surgical technique have remained the same: 1) careful debridement of nonviable, granulation tissue; 2) meticulous preparation of a biological healing surface on the superior and posterior-superior glenoid rim; 3) firm attachment of the detached labrum to the adjacent glenoid rim; and 4) thorough treatment of any concomitant shoulder pathology.
SLAP lesions are classically associated with chronic repetitive overhead activity, but they may also be noted after a single traumatic event, such as a fall on an outstretched arm or a single overhead throw.
The predominant patient complaint is shoulder pain, which may be slowly progressive or significantly worsened following a single throw.
Pain associated with SLAP lesions is often described as deep within the joint or on the posterior aspect of the shoulder joint.
Associated symptoms may include a palpable and/or audible click or pop with glenohumeral motion.
Overhead athletes, such as pitchers, may experience decreased velocity and/or control with throwing.
Physical examination of the symptomatic shoulder should focus on methodical inspection, palpation, range-of-motion assessment, and strength and stability testing, as well as provocative maneuvers, with comparison with the contralateral extremity.
Inspection is often unremarkable, although the overhead-throwing athlete may exhibit greater muscle mass in the dominant throwing extremity. Scapular dyskinesia should also be assessed with attention to elevation of the medial border, protraction, and depression seen in the throwing shoulder.
Palpation of both upper extremities should be performed with a consistent sequence: sternoclavicular joint, clavicle, acromioclavicular joint, acromion, scapular spine, inferior and superior scapular fossae, deltoid muscle mass, anterior and posterior glenohumeral joint lines, and bicipital groove. SLAP lesions may present with pain along the posterior glenohumeral joint line distal and medial to the posterolateral corner of the acromion as well as tenderness of the long head of the biceps tendon along its course anteriorly within the bicipital groove.
Range of motion is often unaffected with isolated injury to the superior labrum. However, it is important to assess the range of motion of both shoulders in multiple planes, including forward flexion, abduction, internal rotation, and external rotation at both neutral position and 90 degrees of abduction. The arc of motion at 90 degrees of abduction is often shifted in the throwing athlete’s dominant shoulder compared with the nondominant shoulder. However, if the total arc of motion is 25 degrees less in the dominant shoulder or if deficits of internal rotation in the scapular plane are greater than 25 degrees compared with the contralateral side, a diagnosis of glenohumeral internal rotation deficit should be entertained in addition to possible labral pathology.
Strength testing should be conducted to assess all rotator cuff muscles as well as the larger muscles of the shoulder girdle.
Stability testing should be carried out, including an assessment of anterior glide with the arm in neutral position and maximum external rotation and posterior glide with the arm in neutral position and maximum internal rotation.
Numerous provocative tests have been proposed for diagnosing a SLAP tear, including the following: clunk, resisted supination external rotation, crank, biceps load, anterior slide, relocation, Mayo shear, forced shoulder abduction and elbow flexion, O’Brien active compression, and modified dynamic labral shear tests. However, no single test or combination of tests has been shown to reliably predict the presence of a superior labral tear. Recent studies have suggested that a combination of O’Brien active compression test ( Fig. 44.1A, B, C, D ) and the modified dynamic labral shear tests ( Fig. 44.2A, B ) may have the highest sensitivity, specificity, and positive predictive value for identifying pathology of the superior labrum.


Additional provocative tests to assess for any concomitant shoulder pathology should be carried out and include the following: 1) Neer and Hawkins tests to identify any weakness or inflammation of the rotator cuff, 2) apprehension/relocation test to identify any anterior instability, 3) posterior glide test to identify any posterior instability, 4) sulcus sign to identify any inferior instability, 5) Speed and Yergason tests to identify any long head of the biceps injury or inflammation, and 6) crossover test to identify any acromioclavicular joint inflammation or arthrosis.
After completion of the shoulder examination, an assessment of the entire kinetic chain should be carried out, especially in the overhead-throwing athlete. Weakness anywhere along the chain may result in increased forces across the glenohumeral joint during throwing. The dynamic Trendelenburg test ( Fig. 44.3A, B, C, D ) can be useful for revealing lower extremity and pelvic musculature weakness. This test requires the athlete to perform a single-leg squat test bilaterally. Kinetic chain weakness is suggested by a combination of hip adduction, contralateral downward pelvic tilt, and trunk rotation or “corkscrewing.”

Imaging is an important adjunct to history and physical examination for the challenging diagnosis of superior labral injury.
Asymptomatic changes may be present on all types of imaging, particularly in the overhead-throwing athlete.
Routine plain radiographs should be obtained in a standard series of views: anteroposterior view of the shoulder in both internal and external rotation, scapular-Y view, and axillary view. These are often unremarkable, but they may provide information regarding the position of the humeral head relative to the glenoid, bony morphology of the humeral head, glenoid and acromion, and arthrosis of the acromioclavicular joint, as well as the presence or absence of intratendinous/intramuscular calcification.
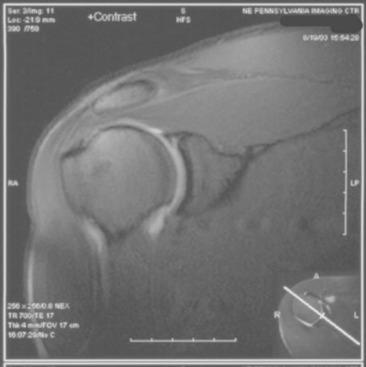
Magnetic resonance imaging (MRI), particularly with the addition of gadolinium arthrography, is considered the gold standard for evaluation of the glenoid labrum. Nonpathologic, meniscoid-like variants of the superior labrum may be noted on MRI/magnetic resonance arthrography (MRA). Fluid/dye extravasation between the superior labrum and the superior glenoid rim with separation of the labrum from its glenoid attachment at or posterior to the biceps root is considered to be most consistent with a SLAP lesion ( Fig. 44.4 ). Additionally, paralabral cysts are often associated with labral pathology, and their presence should increase suspicion for the presence of a SLAP tear. Studies have noted that the extent of a shoulder labral lesion demonstrated by MRI/MRA may correlate poorly with the extent of the lesion encountered at the time of surgery.
Ultrasound has been shown to be highly accurate in diagnosing a variety of shoulder abnormalities, such as rotator cuff pathology, but it may be less sensitive in detecting labral tears.
Changes noted on all forms of imaging should always be correlated with the patient’s history and physical examination when determining optimal treatment.
Nonoperative management should be considered as an initial treatment in the majority of patients with a presumed SLAP tear.
Nonoperative treatment includes a variety of measures.
Rest from any provocative activities, especially overhead sport/work, is maintained for 3–6 weeks, depending on the severity of symptoms.
Heat/ice contrast may benefit during the initial inflammatory phase.
Nonsteroidal antiinflammatory medications for 7–14 days may also provide pain relief if the patient’s medical history allows their use.
Intraarticular corticosteroid injection may ease the early synovitic response.
Biologic treatments such as platelet-rich plasma, stem cells, and combinations have been proposed, but no long-term evidence is currently available to strongly support their use.
Range-of-motion exercises, including gentle passive, active assisted, and active motion, begin once pain has diminished. Particular attention is directed to the posterior soft tissues in order to address any contracture.
Progressive strengthening exercises for rotator cuff and scapular stabilization are carried out.
The kinetic chain is evaluated, and any deficiencies in the core, trunk, and lower extremities should also be addressed.
A progressive tossing/throwing program may be initiated at 3–6 weeks, beginning with gentle tossing at 30 feet and progressively increasing to 180 feet on flat ground. At this point, pitchers may begin throwing from a mound, first with fastballs at increasing effort, followed by off-speed pitches.
Return to sport with nonoperative treatment may begin at 6–12 weeks.
If symptoms persist or worsen in spite of a well-managed nonoperative program in a compliant patient, operative treatment may be considered.
Open treatment of SLAP lesions is largely historical, owing to the greater disruption of the surrounding soft-tissue envelope and difficulty accessing the posterosuperior aspect of the glenoid and labrum.
Arthroscopic treatment of SLAP lesions has become the gold standard. All arthroscopic treatment should begin with a thorough diagnostic arthroscopy to define the type and extent of the SLAP lesion as well as to identify any concomitant pathology. The precise operative treatment is dependent on the type of SLAP tear identified on diagnostic arthroscopy.
SLAP tears were initially classified on the basis of their morphologic appearance into four discrete types. Type I is labral fraying without detachment; type II is detachment of the superior labrum; type III is a bucket handle tear of the superior labrum; and type IV is superior labral tearing with extension into the biceps tendon. Since that time, a variety of additional types have been proposed by numerous authors and represent the four originally described types in conjunction with a variety of concomitant labral, rotator cuff, and biceps pathologies.
Type I SLAP tears are often treated with simple debridement; type II tears are often repaired; type III tears may be treated with a combination of excision and repair; type IV tears may be treated with a combination of excision and repair extending into the biceps tendon; and types V through X tears are often repaired on the basis of specific pattern of injury.
Type II SLAP tears are the most common type of SLAP injury to be surgically treated.
Some surgeons have advocated biceps tenodesis or tenotomy as an alternative or adjunct to SLAP repair in certain patient populations, such as nonthrowing athletes, nonathletes, and older patients with superior labral pathology unresponsive to nonoperative treatment.
The remainder of this chapter focuses on surgical repair of type II SLAP tears. The general principles of repair of a type II SLAP lesion include the following: debridement of any frayed margin of labrum, removal of any fibrous scar tissue, preparation of the superior glenoid rim to healthy bleeding bone, firm reattachment of the superior labrum to the prepared glenoid, and treatment of any concomitant shoulder pathology.
The labrum is a fibrocartilaginous structure that forms the rim of the glenohumeral joint and is contiguous with the glenohumeral ligaments and capsule.
Nonpathologic variants of the glenoid labrum exist and can complicate the diagnosis of a SLAP lesion. Both the sublabral foramen and the meniscoid-type labrum must be carefully distinguished from a pathologic SLAP lesion; this can be accomplished via careful review of preoperative imaging in conjunction with a thorough diagnostic arthroscopy at the time of surgery.
The labrum functions to deepen the otherwise shallow concavity of the glenoid and create cavity compression in order to prevent subluxation or frank dislocation of the humerus through the impressive range of motion of the shoulder joint. The superior labrum serves as the anchor for the long head of the biceps brachii, and this structure is often involved, if not implicated, in SLAP lesions.
Several mechanisms for injury to the superior labrum have been proposed. Some authors have suggested that biceps contraction during the follow-through phase of overhead throwing can apply a traction-avulsion force to the superior labrum, generating a tear. Others have suggested a “peel-back” mechanism in which the humeral head rolls over the superior labrum during the late cocking and early acceleration phases of throwing, causing injury. Still others have suggested that SLAP tears may occur from a combination of both traction and peel-back forces during the entire throwing mechanism. However, the precise pathoanatomic mechanism remains controversial.
Elite-level throwing athletes who have severe initial symptoms with an appropriate history, clear-cut physical examination findings, and easily identified labral tears on imaging studies.
Throwing athletes who have symptoms recalcitrant to a well-coordinated nonoperative program for a minimum of 6–12 weeks.
Nonathletes who have persistent symptoms recalcitrant to a well-coordinated nonoperative program that interfere with daily activities, work, or sleep for a minimum of 12 weeks.
Shoulder arthroscopy can be performed in both the lateral decubitus and beach chair positions. Although both positions have inherent advantages and disadvantages, the authors generally prefer lateral decubitus positioning for the repair of SLAP lesions.
A regional block (i.e., interscalene block) can be performed preoperatively to supplement intraoperative anesthesia as well as assist with postoperative analgesia.
General anesthesia is induced with the patient in the supine position on a standard operating room table over a draw sheet and a vacuum beanbag.
After induction of anesthesia, the patient is placed in the lateral decubitus position with the operative extremity facing up ( Fig. 44.5 ).
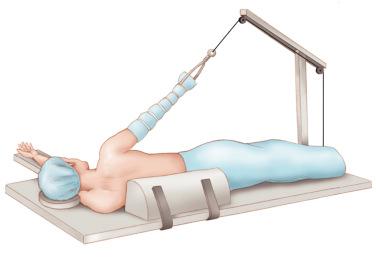
An axillary roll is placed within the axilla of the nonoperative upper extremity. Once the patient is in satisfactory position, the vacuum beanbag is suctioned. Additional buttress side supports are placed along the anterior and posterior thorax to maintain the patient perpendicular to the table. The patient’s head position is checked to ensure neutral flexion/extension and adequate protection of the ear on the decubitus side. Additionally, pillows should be used to cushion both legs after placing them in slight hip and knee flexion, with particular attention to the peroneal nerve.
Finally, an abduction pulley or pole is used to position the operative extremity in approximately 30 degrees of abduction and approximately 30 degrees of forward flexion. Gentle traction with 10–15 pounds of suspended weight (depending on the patient’s body habitus) is applied to the operative arm to distract the joint.
The arthroscopic equipment (including video, light source, pump, and power shaver unit) is placed facing the patient’s chest.
Ensure the patient’s chest is adequately stabilized by the beanbag and side supports.
Ensure the patient’s chest and trunk are perpendicular to the table so that the arthroscopic equipment is freely movable both anteriorly and posteriorly.
With the shoulder in approximately 30 degrees of abduction and approximately 30 degrees of forward flexion, the glenohumeral joint is optimally positioned for superior labral repair.
The amount of traction can be increased according to the size and habitus of the patient.
Lateral decubitus positioning can allow more comfortable and unrestricted instrumentation and visualization, particularly for injuries of the posterosuperior aspect of the labrum.
Failure to adequately stabilize the patient may result in increased mobility of the chest and trunk, making instrumentation more challenging.
Failure to maintain the patient perpendicular to the table can result in restricted motion of the surgical instruments and arthroscope either anteriorly or posteriorly.
Failure to apply adequate traction can result in inadequate joint distraction and thereby limit both visualization and instrumentation.
Vacuum beanbag
Buttress side supports
Abduction pulley with in-line traction and suspended weight (arm holder)
30-degree arthroscopic camera and light source
Fluid pump and suction systems
Standard shoulder arthroscopy instrumentation
Implant of choice
Arthroscopic suture management instrumentation: passing, retrieving, and knot-tying devices
Sling/shoulder immobilizer
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here