Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Skeletally immature bone contains growth plates, or physes, that represent the primary site of longitudinal bone growth. This area of rapidly growing cartilage transitions to bone by a process called endochondral ossification. Due to the nature of this rapid development, physes have much less tensile strength than the surrounding bony epiphysis and metaphysis, thereby rendering the physis more vulnerable to injury as a result of compressive and shearing forces. Injuries to the growth plate are characterized by rapid healing and remodeling but also have the potential for growth arrest or disturbance.
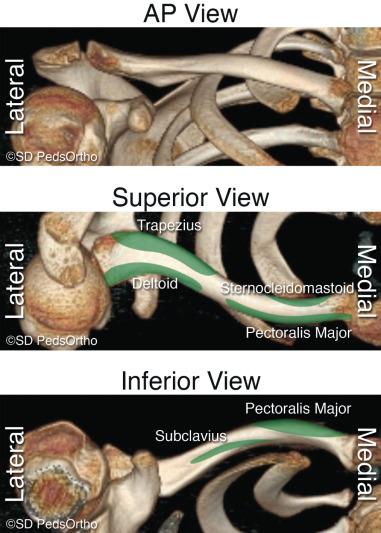
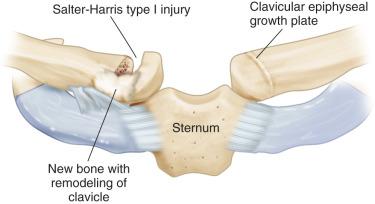
The clavicle forms by intramembranous ossification during the fifth gestational week from two different ossification centers in the diaphysis of the bone. The medial physis of the clavicle is the most important, providing up to 80% of the longitudinal growth of this bone. The medial epiphysis is one of the last in the body to ossify, appearing between 12 and 19 years of age and fusing to the shaft of the clavicle at age 22 to 25 years. The lateral clavicular epiphysis is rarely visualized radiographically, ossifying and fusing during a period of a few months at approximately 19 years of age ( Fig. 133.1 ).
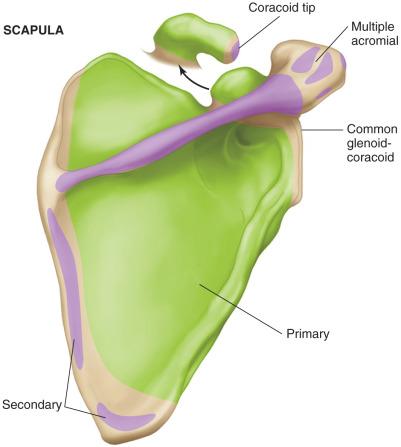
The four primary anatomic components of the scapula are the body, glenoid, acromion, and coracoid. The body of the scapula is oriented at a 30- to 45-degree angle to the coronal plane of the body, and it forms by intramembranous ossification through multiple ossification centers that are highly variable in terms of number and position. The glenoid has an average of 5 degrees of superior tilt and retroversion of 3 to 9 degrees in relationship to the long axis of the scapula. The base of the coracoid and upper glenoid develop from a common physis that ossified at approximately 10 years of age. A variable ossification center can appear at puberty at the tip of the coracoid and may be mistaken as an avulsion fracture. The acromion ossifies through several centers that appear by puberty and fuse by the age of 22 years. Failure of fusion of one of the acromial physes can result in an unfused os acromiale, which may have future clinical implications ( Fig. 133.2 ).
The humerus is completely ossified throughout its diaphyseal and metaphyseal portions at birth, with the secondary ossification center for the head appearing 6 months after birth. The secondary ossification center for the greater tuberosity appears by age 3 years, followed by the secondary center for the lesser tuberosity approximately 2 years later. By age 5 to 7 years, the three proximal ossification centers of the humeral head, greater tuberosity, and lesser tuberosity coalesce to become a single proximal ossification center. The proximal humeral physis usually closes between 18 and 22 years of age and accounts for approximately 80% of longitudinal growth of the humerus. The head forms an upward head shaft angle between 130 and 140 degrees and is in 25 to 30 degrees of retroversion as it relates to the humeral epicondyles ( Fig. 133.3 ).

Clavicle fractures account for 8% to 15% of all skeletal injuries in children. Despite these injuries being extremely common, little historical attention in the literature had been focused on this topic. The principal reason for this was the belief of Rang and others that “if the two ends of a clavicle fracture are in the same room they will heal and remodel adequately.” These fractures can be classified as either lateral, midshaft, or medial, with midshaft fractures occurring most frequently.
Over the past 10 years, a renewed interest in the clavicle has occurred, largely driven by several clinical trials showing the benefits of surgical stabilization of displaced clavicle fractures in adults. As a result, many have begun to apply these principles to adolescent and even pediatric patients. Two recent studies have shown a more than doubling of pediatric clavicle fractures being fixed surgically over the past 10 years. This trend is likely occurring as a result of several factors, including the lack of literature in this younger patient population, fear that a mismanaged clavicle fracture may lead to a less satisfactory functional outcome, parental and patient pressure to return young athletes to the sports field quickly, and differing reimbursement regimens for nonoperative versus operative management.
Most clavicle fractures occur as a result of a direct fall on the shoulder with the arm at the side, but less commonly a fracture may occur as a result of a direct blow or a fall on an outstretched hand. Sports participation, especially contact sports including football, rugby, wrestling, and hockey, are responsible for the largest percentage of these fractures in adolescence. However, with our nation's increased interest in extreme sports such as bike motocross (BMX), motorcycle racing, and mixed martial arts (MMA), these higher-energy fractures are being seen more frequently.
The examination of a child or adolescent with a clavicle fracture is relatively straightforward given the superficial nature of the bone. Typically, the patient will present with the arm being held in an adducted position close to the body with the opposite hand supporting the injured extremity. The skin should be inspected for an open fracture or significant tenting which has the rare chance to erode through the skin with severe angulation. Limb- and life-threatening concerns, although extremely rare, can occur and need to be identified immediately. These include vascular injuries (subclavian vessels), neurologic injuries (brachial plexus), and injuries to the mediastinal structures (esophagus, trachea, pleura, lung) by angulated or displaced fragments.
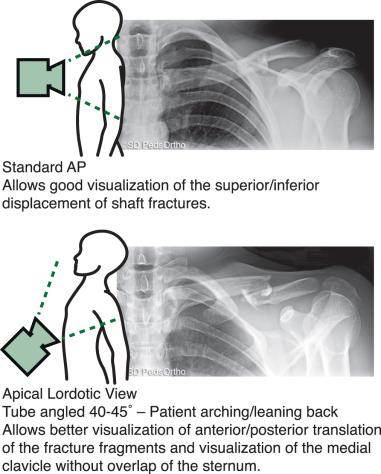
Almost all midshaft clavicle fractures can be adequately identified with a single anteroposterior (AP) view. Typically, a second view, such as an apical lordotic view or 30-degree cephalic tilt view, is obtained, which can provide further information as to the fracture's displacement, shortening, or comminution ( Fig. 133.4 ).
Nearly all mildly displaced clavicle fractures can be treated with either a sling or a figure-of-eight brace. A theoretical advantage of the figure-of-eight brace is that it potentially pulls the shoulders back, minimizing fracture fragment overlap. A practical advantage is that it frees the extremity, making simple daily tasks such as computing easier. In contrast, practical advantages of the sling include its ease of use, its ubiquitous availability, and its cost effectiveness. Two clinical trials failed to show significant outcome differences between slings and figure-of-eight braces. As a result, there is a bias with most surgeons preferring slings. When a nonoperative approach is used, the fracture is protected for 4 to 6 weeks, with contact sports avoided for another 6 weeks. As in most injuries, half the treatment consists of educating the parents about the normal course: An unsightly lump may appear with fracture healing (callus) and will potentially persist for a year while remodeling progresses ( Fig. 133.5 ).

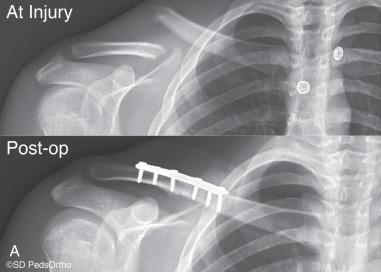
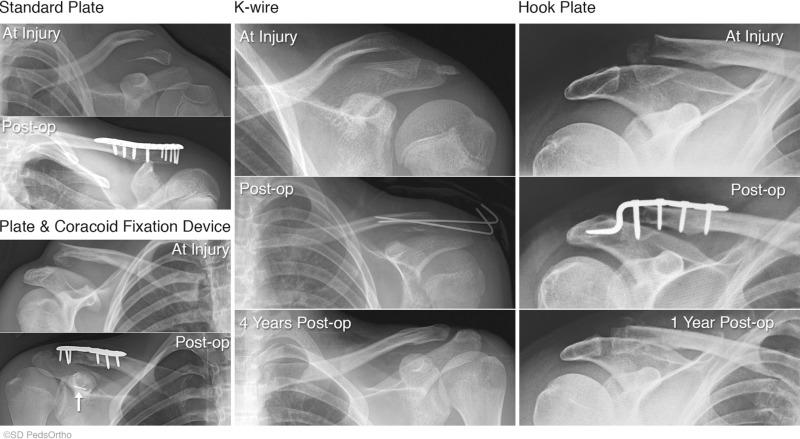
For the rare midshaft clavicle fracture requiring surgery, fixation can be achieved with a precontoured plate or an intramedullary device. To date, no study has compared the results of these two implants in the pediatric population, but there are case series reporting good outcomes with both approaches ( Fig. 133.6 ). Theoretical advantages of plate fixation are that it can be used with all fracture patterns (even severe comminution), and it creates a rigid construct enabling early mobilization and rapid return to sports. The primary advantages of intramedullary devices are that they potentially minimize the scar length, lessen any infraclavicular numbness, and are potentially less prominent and symptomatic. When plate fixation is selected, the use of a precontoured plate may lessen the need for implant removal. After surgery, a sling is used for comfort for 1 to 2 weeks, allowing early hand, elbow, and shoulder motion exercises. Strengthening exercises are initiated at approximately 6 weeks, when interval healing is appreciated on radiographs. For noncontact sports, it is reasonable to return patients as early as 6 weeks if the patient has no pain, full range of motion (ROM), and good strength. For higher-risk sports and activities, a longer period upwards of 3 months may be necessary to minimize the chance of a refracture. Anecdotally, we have found that patients with displaced fractures undergoing surgical fixation can return to sports faster, but certainly, we do not want to advocate that this as justification for operative intervention. Implants are routinely left in place but may need to be removed in as many as 40% of cases.
Historic data examining pediatric and adolescent patients with midshaft fractures would suggest that these fractures heal reliably with few residual symptoms. However, these studies did not take into account the amount of fracture shortening or displacement and did not look at patient-reported outcomes or formal strength testing. Two current studies have examined functional outcomes and strength testing in patients with displaced midshaft clavicle fractures, and good outcomes were achieved with nonoperative treatment, with no major functional deficits. However, a separate study by Vander Have et al. showed that symptomatic malunions can occur in adolescent patients and may be as high as 20%. Currently, optimal surgical indications in this patient population have yet to be clarified. When surgical intervention is pursued, good outcomes have been almost uniformly reported.
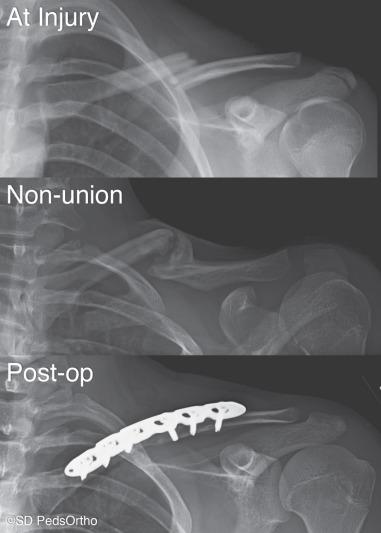
Complications are uncommon but can occur both with operative and nonoperative treatment. The most common complications of nonoperative treatment include symptomatic malunions, refracture (especially fractures with residual angulation), and the rare nonunion (<15 having been reported in the literature) ( Fig. 133.7 ). The most common complications of surgical intervention are implant related (10% to 40%), but nonunions, refractures, infections, and neurovascular injuries have also been reported.
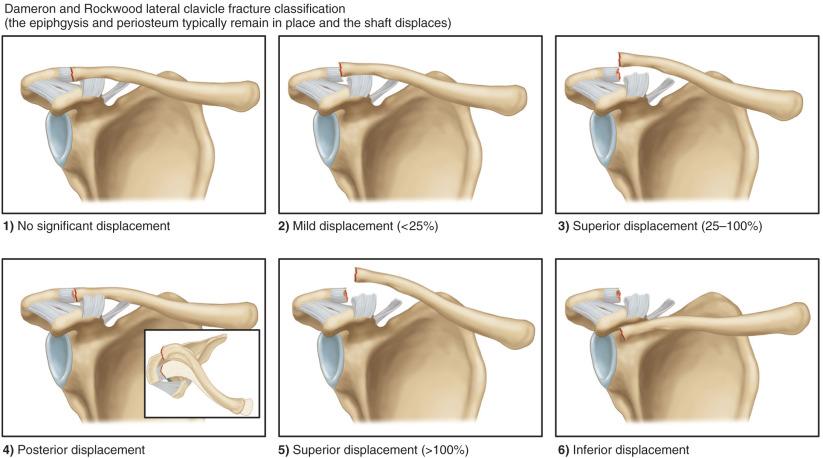
Although injuries to the distal clavicle in children are similar in many ways to the adult acromioclavicular (AC) joint injury, the distinct differences are a reflection of the developmental anatomy of the distal clavicle. The distal clavicle is surrounded by a thick periosteal sleeve that is continuous laterally with the AC joint capsule and inferiorly with the coracoclavicular ligaments. The physis of the distal clavicle lies within the periosteal sleeve medial to the attachment of the AC joint capsule. The epiphysis, which is rarely apparent radiographically, is tightly bound to the AC joint; failure in the skeletally immature athlete therefore usually occurs through the physis as opposed to an adultlike dislocation through the AC joint. Classification of distal clavicle injuries is based on the degree of disruption of the periosteal sleeve and the direction and degree of displacement of the shaft fragment (see Fig. 133.8 ).
Typically, the athlete has a history of a fall on the point of the shoulder. The blow directed to the top of the scapula can lead to disruption of the periosteal sleeve and fracture through the physis. There is immediate pain, and the athlete may relate a feeling of instability. Transient symptoms of numbness or dysesthesia are occasionally experienced, similar to that of a brachial plexus stinger or burner. The injury may occur with an indirect mechanism, such as a fall on an outstretched, adducted arm that drives the humeral head into the acromion.
On inspection, the amount of deformity relates to the degree of injury. Mild type I and type II injuries may demonstrate only localized swelling, whereas type III and type V injuries are characterized by clinically significant deformity caused by the displaced distal clavicle shaft. Type II and III injuries may appear fairly benign when visualized from the front, but, when inspected from above, the deformity of the displaced clavicle posterior into the trapezius can be recognized. The athlete often supports the affected arm with the opposite hand and resists shoulder ROM. Tenderness to palpation over the distal clavicle is uniformly present. Acutely, muscle strength testing is limited by pain. Neurologic testing should be performed to rule out brachial plexus involvement. In less severe cases, the cross-arm adduction test is usually positive. This test is performed by positioning the shoulder into flexion of 90 degrees followed by bringing the arm across the chest into adduction. Pain referable to the AC joint region is a positive test finding.
In the case of injury to the distal clavicular physis, routine AP views may be overpenetrated; a special Zanca view may therefore be indicated ( Fig. 133.9 ). This view is performed by angling the beam 10 to 15 degrees toward the head and using only 50% of the standard AP shoulder penetration. The distal clavicular epiphysis is rarely visualized on plain films because it appears and fuses over a short period at approximately 19 years of age. Distal physeal injury is therefore inferred by the degree of shaft displacement in relation to the acromion and coracoid. Comparison views of the opposite shoulder can often be useful, particularly when trying to determine the normal coracoclavicular distance. The axillary lateral view is important to differentiate a type IV injury by demonstrating the posterior position of the shaft fragment in relation to the acromion. Stress views of the shoulder are not necessary in assessing distal clavicular physeal injury.

Injuries to the distal clavicular physis represent Salter-Harris type I injuries, and healing is virtually always the rule. The periosteal sleeve remains in continuity with the AC joint capsule and the coracoclavicular ligaments; stability is achieved when the periosteal sleeve fills with healing new bone. Even in cases with large degrees of displacement, remodeling potential in this injury is significant and residual deformity is unusual. Nonoperative treatment is therefore acceptable in most type I, II, and III cases of distal clavicular physeal fracture. In younger patients with greater degrees of remodeling potential, even cases of type V injury should be considered for nonoperative treatment. Nonoperative treatment includes a short period of immobilization and supportive care with ice and analgesics followed by a progressive rehabilitation and return to play (RTP) program. Type I or II injuries may be able to return as early as 1 to 2 weeks but typically take 4 to 6 weeks, whereas type III and type V injuries treated nonoperatively will normally take 6 weeks or longer.
Surgical treatment for fractures of the distal clavicular physis is reserved for type IV injuries, type VI injuries, and type V injuries in adolescents who have less remodeling capability. The procedure includes reduction of the displaced shaft fragment and repair of the periosteal sleeve versus fixation with plates and screws, Kirschner wires, or coracoclavicular fixation devices ( Fig. 133.10 ). After surgery a sling is used for 2 weeks, allowing early hand and elbow motion and shoulder pendulum exercises. Between 2 and 6 weeks gentle shoulder motion progresses, but lifting is not allowed. Progressive strengthening and functional activities are then initiated as tolerated. After surgical treatment, RTP follows complete radiographic healing and rehabilitation, which may require 10 to 12 weeks.
Because of the great potential for healing and remodeling of this fracture in this age group, results for treatment of an injury to the distal clavicular physis are almost uniformly good. Several reports in the literature for both surgical and nonoperative treatment demonstrate good results.
Although most distal clavicle fractures heal uneventfully with nonoperative treatment, occasionally a nonunion will be identified, especially in an older adolescent patient with a type IV or V fracture that is button-holed through the trapezius muscle. The primary complication of surgical treatment is related to the implants either being symptomatic given the superficial nature of the distal clavicle or inadequate fixation resulting in loss of reduction, which is not uncommon given the small size of the lateral fracture fragment.
Injuries to the medial end of the clavicle represent between 1% and 6% of all clavicular injuries in skeletally immature patients. These fractures are classified according to the anatomic position of the shaft fragment in relation to the epiphysis and sternum. The shaft can be displaced either anteriorly or posteriorly as it penetrates the periosteal sleeve that remains attached medially to the epiphysis and joint capsule. Although anterior displacement is the most common type of injury, posterior displacement is the most important to recognize because of potential impingement of structures within the mediastinum. Most of these physeal fractures are characterized as Salter-Harris type I and II injuries ( Fig. 133.11 ).
Injury to the medial clavicle can occur as a result of either direct or indirect forces, with the indirect mechanism being most common. A typical history given by the athlete includes a fall with the athlete's opposite shoulder on the ground while several other players pile on top of the shoulder, applying significant compressive force directly to the medial clavicle. The less common direct mechanism may occur when a force is applied directly to the anteromedial aspect of the clavicle during contact sports, resulting in a fracture through the physis. If displacement results, the shaft fragment would penetrate the periosteal tube posteriorly and potentially become retrosternal, with possible injury to structures within the mediastinum. Most athletes with medial clavicular physeal fracture have immediate pain with a specific traumatic episode. It is important to elicit any symptoms of impingement on mediastinal structures if a posterior displacement is suspected. Symptoms of shortness of breath, choking, difficulty swallowing, or any neurologic or vascular symptoms should be of concern to the examiner.
In a nondisplaced injury to the medial physis, the ligaments of the joint and periosteal sleeve are intact. The patient reports pain with ROM of the upper extremity. The area is typically swollen and tender to palpation, but instability and crepitus are absent. In a more severe injury to the physis with displacement of the shaft fragment, swelling, and severe pain with any movement of the arm are common. The injured arm is often supported with the normal arm, and the head may be tilted toward the side of the dislocated joint because of spasm of the surrounding musculature. Swelling may be substantial, disguising the position of the displaced shaft fragment. Careful palpation of the shaft in relation to the epiphysis and sternum should be performed in an attempt to discern anterior versus posterior displacement. In suspected posterior displacement, careful examination of the upper extremity should document neurologic status and adequacy of pulses or any venous congestion that may be present. Breathing difficulties, voice changes, or a choking sensation should be noted. If the patient demonstrates some or all of these signs and symptoms of mediastinal impingement, treatment becomes a relative emergency and should be promptly instituted.
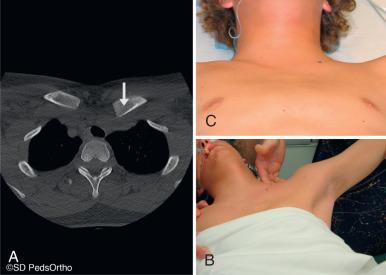
Plain radiographs of the medial clavicle, including the AP and lateral views, can be difficult to interpret because of overlap with other structures, including sternum, ribs, and spine. A special oblique view, known as the serendipity view, has proven to be the most valuable plain radiographic technique. With the patient supine in the center of the x-ray table, the tube is tilted at a 40-degree angle off the vertical, centered directly on the sternum. This view demonstrates a side-to-side comparison of the medial clavicle and sternoclavicular joint and allows evaluation of potential displacement or fracture. In cases with suspected posterior displacement, a computed tomography (CT) scan may be necessary to confirm the fracture/dislocation and the degree and location of displacement ( Fig. 133.12 ).

As is the case of all fractures involving physes, the expectation for rapid healing and significant remodeling in fractures of the medial clavicle is the rule. With this in mind, treatment of these fractures will be generally more conservative than in cases of sternoclavicular joint dislocation. Conclusive data regarding recognition, treatment, and specific outcomes are limited to case reports and small series, but results of treatment for this injury are generally good by whatever means. Treatment is based on both the degree and direction of displacement of the shaft fragment, with special attention to cases with posterior position of the shaft fragment that may result in impingement of mediastinal structures. In physeal fractures with mild to moderate displacement in either direction, treatment is always by observation and supportive care. If significant anterior displacement of the medial physeal injury is recognized, closed reduction can be considered. If attempted, closed reduction should be performed with the patient under general anesthesia and positioned supine with a pad between the shoulders. While applying lateral traction on the arm, direct pressure is applied to the anteriorly displaced clavicle while the shoulder is pushed posteriorly. The reduction is maintained by placing the patient in a figure-of-eight splint for 2 to 4 weeks. If the clavicle fracture is unstable, the deformity is accepted, and healing and remodeling of the fracture will usually correct any residual deformity. Some clinicians suggest that benign neglect can be successful for all fractures with anterior displacement.
In athletes who demonstrate posterior displacement of the medial physeal fracture, closed reduction should be performed with the patient under general anesthesia ( Fig. 133.13 ). Of note, many surgeons prefer to have a general surgeon or cardiothoracic surgeon available for these procedures. With the patient in the supine position and a pad placed between the shoulders, traction is applied to the abducted arm, which is then slowly brought into extension. It may be necessary to apply lateral and anterior traction to the medial clavicle either manually or with a percutaneous towel clip to accomplish reduction. The reduction is usually stable, with the shoulders held back in a figure-of-eight dressing or strap. If the posterior physeal injury cannot be easily reduced closed, and if the patient has no symptoms of impingement of the mediastinal structures, the injury can be treated expectantly. Healing and remodeling commonly result in a stable clavicle with no long-term sequelae. Open reduction of a medial clavicular physeal injury is indicated for cases of irreducible posterior displacement in a patient with signs and symptoms of compression of the mediastinal structures. Reduction performed through an open approach is usually accomplished without difficulty. Reduction is maintained by repairing the thick periosteal tube and maintaining the patient in a figure-of-eight brace as for closed reduction. Successful results for the open treatment of posteriorly displaced medial clavicular physeal fractures in young athletes have been reported.
Acute complications associated with medial clavicular physeal fracture are primarily limited to impingement of mediastinal structures. Long-term issues related to malunion are unusual in the skeletally immature patient because of the great propensity for remodeling of the physeal fracture with time. Many complications have been previously reported with the use of metallic implants for fixation of fractures and dislocations in this area. Pin breakage and migration have led most authors to recommend that metal not be used in the medial clavicle and sternoclavicular joint.
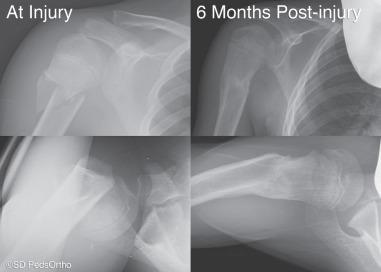
Although fractures involving the upper extremities are the most common injuries in young athletes, the incidence of proximal humeral physeal injuries has been reported to range between 2% and 7%. Despite this relatively low incidence, these injuries can be serious in terms of time lost from participation. Fractures involving the proximal humeral physis usually occur as a result of high-energy sports such as football, soccer, hockey, skiing, skateboarding, and BMX riding. Fractures of the proximal humeral physis can be classified by location and the degree of displacement ( Fig. 133.14 ). In addition, fracture stability is important in the treatment algorithm and depends on the degree of initial displacement and the degree of initial trauma. When the physis is involved, these fractures can also be described using the Salter-Harris outlined in Fig. 133.15 .
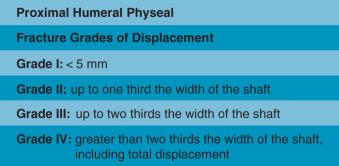
Fractures through the proximal humeral physis typically occur in adolescent males as they near skeletal maturity. Salter-Harris type I fractures are less common and tend to occur in athletes younger than 12 years of age. In adolescent athletes 12 years and older, most fractures are Salter-Harris type II fractures. These fractures tend to occur as the result of direct or indirect mechanisms. Falls directly onto the shoulder or a blunt force or strike are responsible for most direct mechanisms, whereas indirect trauma tends to result from a fall on an outstretched hand with the arm abducted and externally rotated.
Athletes with nondisplaced fractures often present with only minimal swelling and tenderness localized over the proximal humerus. Motion and resisted rotation are limited because of pain. When greater degrees of physeal displacement are present, considerable bleeding into the soft tissues can produce marked swelling. The athlete reports pain with any motion and usually holds the extremity adducted to the chest, supported at the elbow and forearm with the opposite hand. The neurologic and vascular status of the upper extremity must be assessed to rule out injury to any peripheral nerves, the brachial plexus, or vascular structures.
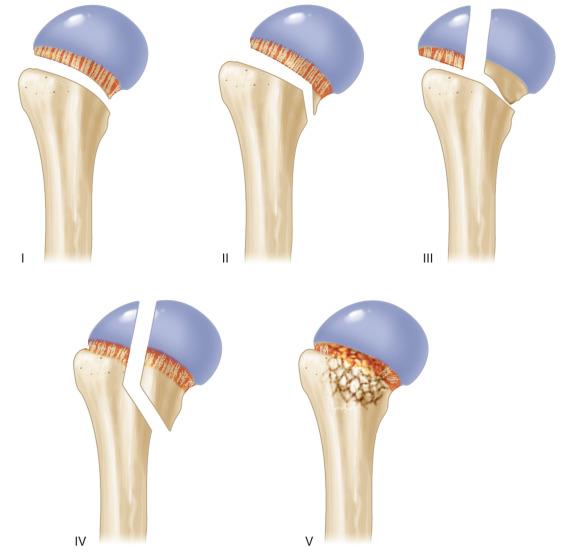
Routine radiographs of the shoulder, including the AP view and axillary lateral view, should be obtained if possible. Frequently, an axillary lateral view is challenging in these situations because the patient is unable to elevate the arm secondary to pain. In such cases a transthoracic lateral, a scapular Y view, or a clear view may be helpful to properly and safely evaluate the shoulder ( Fig. 133.16 ). Occasionally, a CT scan will be necessary to better evaluate an intra-articular fracture, to identify a lesser tuberosity fracture, or to better identify the degree of displacement or comminution if present. All radiographs should be scrutinized for a pathologic fracture because unicameral and aneurysmal bone cysts (UBCs and ABCs, respectively) are not infrequent in this patient group ( Fig. 133.17 ).

The proximal humeral physis contributes approximately 80% of the longitudinal growth of the humerus, thus allowing great potential for remodeling after fracture. The younger the athlete, the greater the potential for remodeling, and the need for anatomic alignment is less important. However, in the adolescent athlete with less growth remaining, adequate time to remodel the deformity may not remain. The dilemma for the treating physician then becomes when to use aggressive treatment for these fractures. Although no absolute criteria exist in the literature as to what amount of displacement or angulation can be tolerated before closed reduction or surgical intervention is necessary, several authors have made recommendations. Some have suggested surgery for fractures with angulation greater than 40 degrees or 50% displacement regardless of age. Others have suggested that the patient's age should be factored into decision-making, with angulation up to 75, 60, and 45 degrees being acceptable in patients younger than 7 years, 8 to 11 years, and 12 years or older, respectively.
In cases of nondisplaced to mildly displaced or angulated fractures, treatment is usually successful without attempting reduction of the fracture ( Fig. 133.18 ). Initial protection in a sling or shoulder immobilizer followed by rehabilitation is usually all that is necessary to obtain a good result. Most authors reserve attempts at closed reduction for displaced fractures. The argument for reduction of the fragments is that it decreases the degree of shortening and varus deformity that develops if the malalignment is allowed to persist. Various closed methods have been advocated to realign the fracture fragments into a more anatomic position. Closed reduction can be performed under anesthesia by bringing the distal shaft fragment into flexion with some abduction and external rotation to align it with the flexed, abducted, and externally rotated proximal epiphyseal fragment. After closed reduction, options to maintain position without internal fixation include a sling, brace, cast, or olecranon pin skeletal traction, but this a treatment more of historical interest.
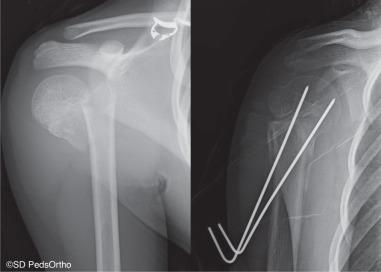
Indications for operative treatment include inability to gain an adequate closed reduction or inability to maintain anatomic closed reduction. Most authors prefer a closed technique when possible, followed by percutaneous pin fixation under fluoroscopic control. This has been shown to be a highly effective method of maintaining an unstable reduction. Typically two to three smooth or threaded tip pins are passed from the metaphysis retrograde across the fracture into the humeral head ( Fig. 133.19 ). This technique has the advantage of maintaining fracture alignment with the arm in the normal position, supported only with a sling or brace. The pins can be removed within 2 to 4 weeks due to the rapid healing of the physeal fracture. Retrograde nailing with elastic nails has gained popularity, particularly in fractures involving the metaphysis. On occasion, an open reduction is necessary when a satisfactory reduction cannot be obtained by a closed manipulation or in cases of open fractures or vascular injuries. Failure to obtain adequate closed reduction is more common in Salter-Harris type III and IV injuries and occasionally in cases of Salter-Harris I and II fractures in which the periosteum or the biceps tendon has become interposed in the fracture site. Fixation after open reduction can include smooth or threaded tip pins, screws, retrograde nails, or contoured plate fixation. Screws and plate fixation would only be used in athletes very near skeletal maturity. Many reports have cited the success of open reduction and fixation in these difficult cases, with most patients returning to sports without limitations typically at approximately 12 weeks.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here