Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
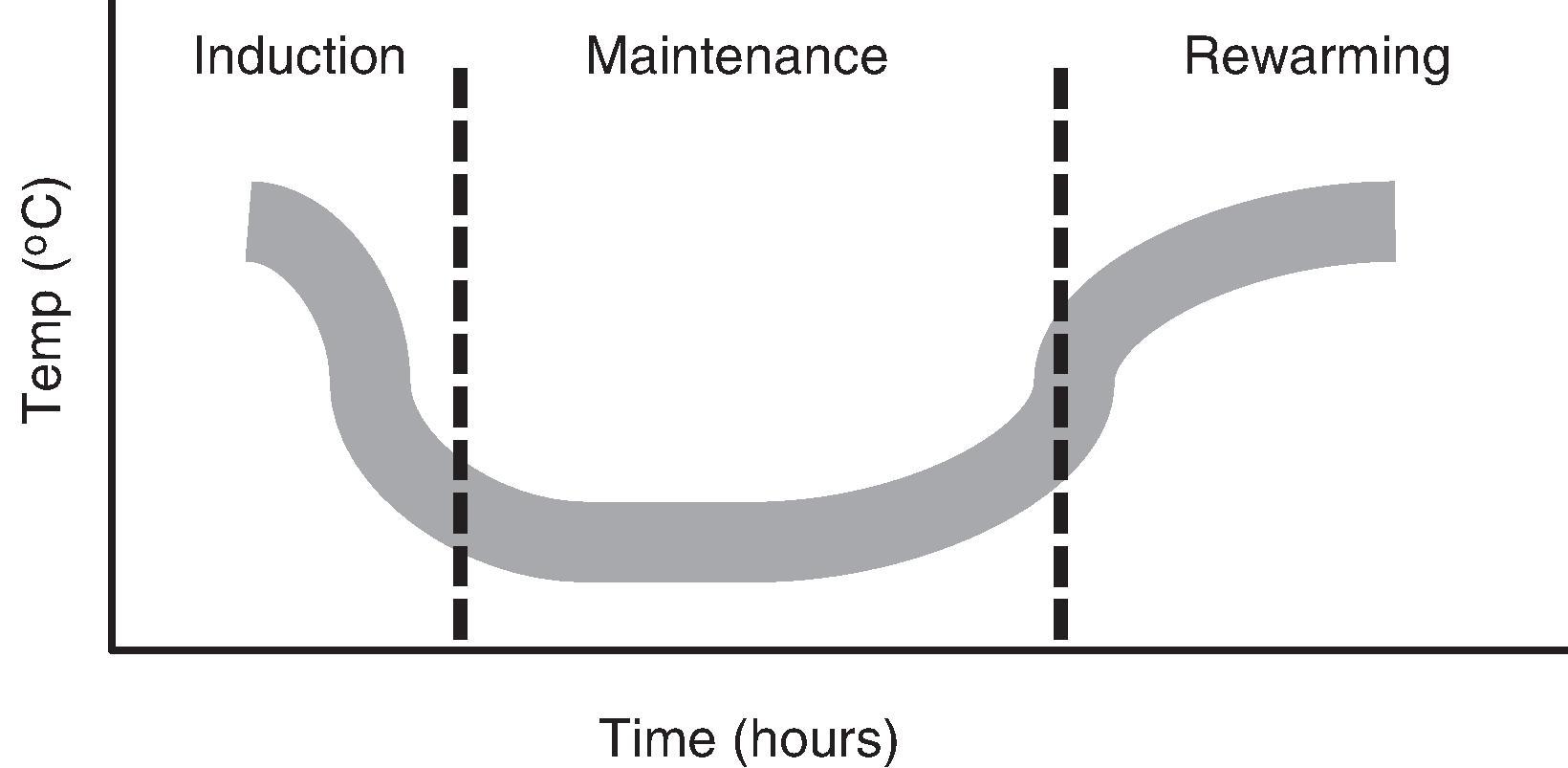
More than 500,000 people experience cardiac arrest in the United States each year, and approximately half of these occur in the hospital environment. Resuscitation attempts are unsuccessful in the majority of cardiac arrest victims, although as many as 30% to 45% of patients achieve the restoration of circulatory function (return of spontaneous circulation [ROSC]). Even among those who are successfully resuscitated, many have a guarded prognosis secondary to neurologic injury that often results in crippling long-term disabilities for cardiac arrest survivors. Neurologic outcomes from cardiac arrest have improved over the past decade through the use of therapeutic hypothermia (increasingly referred to by the more broad term of targeted temperature management [TTM]), and protocols for this therapy have been implemented in a wide variety of hospital environments. TTM after cardiac arrest involves three phases of care: induction, maintenance, and rewarming ( Fig. 34.1 ), and each phase requires commitment of time and resources as well as potential exposure to specific adverse effects. Therefore the risks and benefits of TTM use have to be considered carefully in light of the published evidence, which remains more robust for out-of-hospital arrest in contrast to in-hospital arrest.
In this chapter, we will review the therapeutic options and approach to TTM induction and maintenance, discuss the current evidence regarding the use of TTM in cardiac arrest patients, and evaluate to what extent such evidence extends to the perioperative or intraoperative setting.
Before TTM is induced, patients are typically sedated and often managed with neuromuscular blockade (NMB) to avoid shivering, although the additive benefit of NMB remains unclear. It is generally held that shivering can occur during TTM induction until a patient’s core temperature falls below 33°C, when the brainstem shivering reflex appears to become attenuated. Shivering has a number of potentially deleterious effects, including increased metabolic rate, increased risk for rhabdomyolysis and secondary acute tubular necrosis, and heat generation, which, in turn, can slow the desired rate of therapeutic cooling. A number of pharmacologic options exist for sedation and paralysis, and there are no convincing data that specific agents are preferred over others. An understanding of pharmacology during postarrest TTM is limited, but some data support that benzodiazepine metabolism may be altered with reduction of core body temperature, resulting in higher than expected drug levels in the cooled patient; this may result in more prolonged mechanical ventilation and a longer duration in the critical care environment.
Varied devices to facilitate induction of TTM exist, including intravascular and external modalities. Intravascular methods include the use of cooling catheters and the administration of chilled intravenous (IV) fluids. External options include the use of water-filled cooling blankets and hydrogel pads that are applied to the skin. Consensus has grown that “closed-loop” TTM devices (with ongoing temperature-sensing input and automatically controlled adjustment of temperature output) are superior to simple TTM methods that involve direct contact with ice or cooling fans. A combination of methods can be used; for example, chilled fluids are often used in TTM protocols as an initial “booster” to start the cooling process while either intravascular or external TTM devices are prepared and applied. Observational studies have confirmed that for the majority of postarrest patients (e.g., not including those with renal failure), bolus administration of 1 to 2 L of chilled saline is safe and carries little risk for pulmonary edema, despite the concern for postarrest myocardial depression. This is a useful approach in some cases for accelerating the cooling process because laboratory trials have shown that more rapid attainment of the goal temperature (32°C–34°C) is associated with improved survival rates and neurologic outcomes; indeed, recent cohort data have supported this time sensitivity and have suggested that a “door-to-TTM initiation” time of less than 2 hours was associated with better clinical outcomes. , Chilled saline or ice packs alone, however, have limited utility, except perhaps in the prehospital setting as a bridge to hospital care because temperature control during the required 12- to 24-hour maintenance is problematic. Prior work has shown that overcooling and undercooling are common unless a thermostat-driven device is used to maintain 32°C to 34°C. During induction and maintenance, continuous temperature measurement should be established via an esophageal, bladder, or rectal probe. Most commercially available TTM devices can receive temperature input from such probes and control the rate of cooling or warming accordingly.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here