Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Individuals with differences of sexual development lack concordance of various aspects of gender. These aspects include chromosomal sex (46,XX, 46,XY, or other), gonadal or reproductive sex (ovaries, fallopian tubes, and uterus vs. testes, seminal vesicles, prostate gland, and ejaculatory ducts), genital sex (vagina and clitoris vs. scrotum and penis), and gender-specific behavior. Depending on chromosomal sex, most patients can be classified as incompletely masculinized 46,XY males, virilized 46,XX females, and patients with abnormalities of sex chromosomes, such as individuals with mixed gonadal dysgenesis. Many conditions can cause differences of sexual development ( Table 214-1 ).
| VIRILIZATION OR SEX REVERSAL IN XX FEMALES | MICROPENIS |
|---|---|
Virilizing forms of congenital adrenal hyperplasia
Maternal or exogenous androgens
Mutations in genes affecting gonadal differentiation
Structural/idiopathic |
Panhypopituitarism (combined pituitary hormone deficiency) [ PROP1, FGF8, PROKR2, WDR1 ] Septo-optic dysplasia [ HESX1, FGFR1 ] Isolated hypogonadotropic hypogonadism [ GNRH1, GNRHR, KISS1, KISS1R, TAC3, TACR3 ] Other syndromes, including hypogonadotropic hypogonadism
Vanishing testes (may also cause ambiguous genitalia) |
| UNDERVIRILIZATION OR SEX REVERSAL IN XY MALES | OTHER SYNDROMES AFFECTING REPRODUCTIVE SYSTEMS |
Biosynthetic defects
Androgen insensitivity (1:20,000) [ AR ]: complete or partial
Exposure to 5α-reductase inhibitors, other endocrine disruptors |
Chromosomal aneuploidy
Persistent müllerian duct syndrome in XY males
Mayer-Rokitansky-Küster-Hauser syndrome (vaginal atresia) (1:6000) |
∗ Frequencies of relatively common (at least 1:20,000) diseases are noted in parentheses. When causative genetic mutations have been identified, the affected locus is noted in square brackets.
At 4 to 5 weeks’ gestation, the gonadal primordia (gonadal ridges) develop from the coelomic epithelium overlying the medial surface of the mesonephros (primitive kidneys; Fig. 214-1 ). These primitive gonads are identical in both sexes. Germ cells form at 3 to 4 weeks’ gestation and migrate through the gut mesentery into the gonads at this early bipotential stage. This first stage of gonadal development is controlled by homeobox genes.
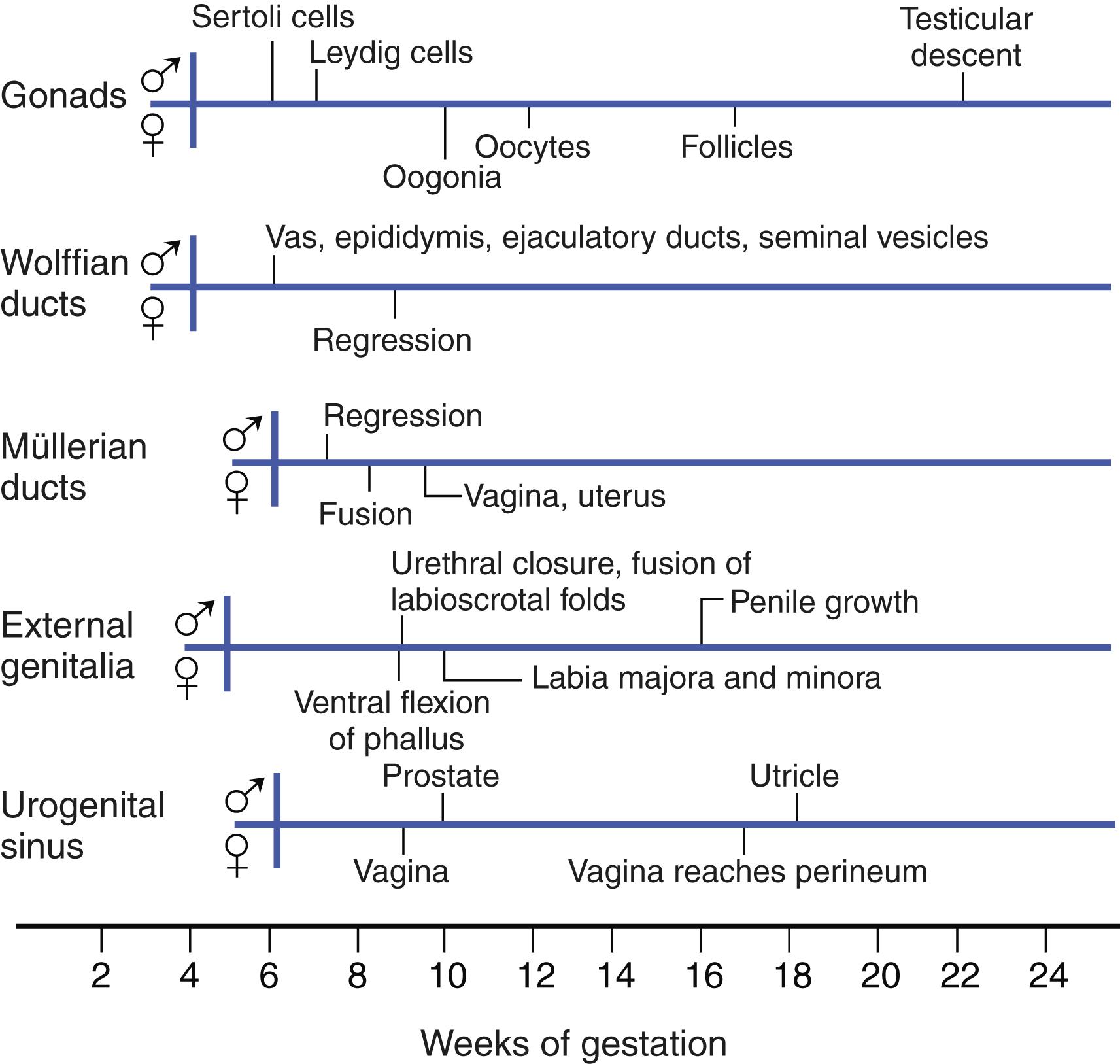
During the seventh week, XY male gonads begin to differentiate under the influence of testis-determining genes. The first to be expressed is SRY , which is the key gene on the Y chromosome that controls male differentiation. Sertoli cells surround germ cells to form testis cords, which nourish primordial germ cells and direct them into the pathway for male gametogenesis. Recruitment of endothelial cells leads to development of a testis-specific vasculature that is required for normal organization of the testis.
Steroidogenic cells develop from the mesonephros and migrate into the developing adrenal cortex and testis at 8 weeks. In the testis, they become Leydig cells, which secrete the testosterone required for subsequent male reproductive development. In the first trimester, testosterone secretion is mainly under the control of human chorionic gonadotropin (HCG), but it subsequently requires luteinizing hormone (LH) secreted by the fetal anterior pituitary.
Ovaries are recognizable at approximately 10 weeks. Ovarian development requires the active participation of several signaling pathways that repress expression of testis-specific genes and promote ovarian development.
The reproductive tracts are derived from intermediate mesoderm. The male reproductive tract develops from the mesonephric (wolffian) ducts, and the female reproductive tract develops from the paramesonephric (müllerian) ducts ( Fig. 214-2 ). Both sets of ducts are present in normal embryos.
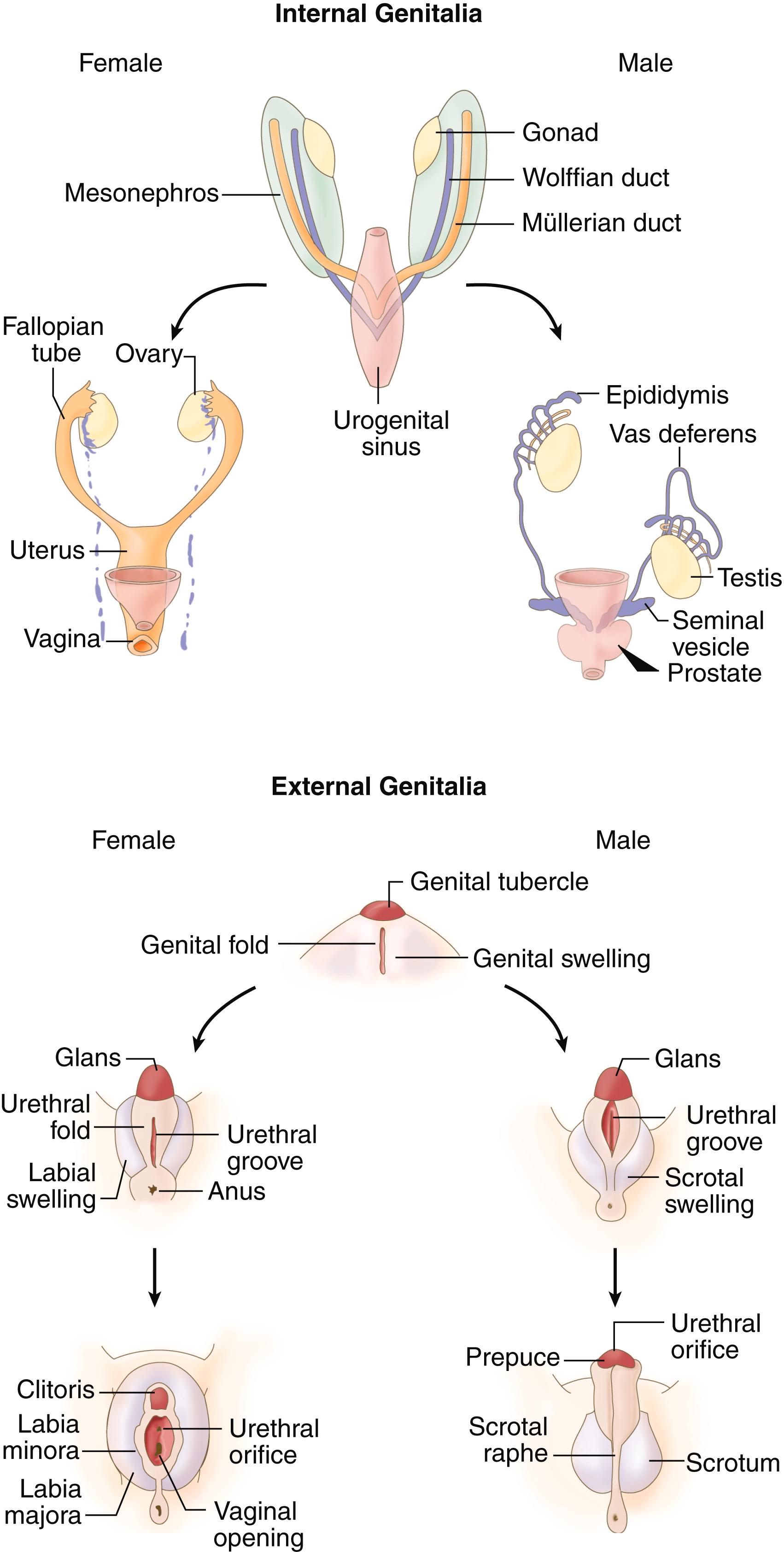
Development of wolffian or müllerian structures depends on the presence or absence of normally functioning testes, respectively. The Sertoli cells secrete antimüllerian hormone starting when the testes differentiate. Antimüllerian hormone induces regression of müllerian structures between 8 and 12 weeks’ gestation. In its absence, development of the müllerian ducts proceeds, and the female internal structures (fallopian tubes, uterus, cervix, and upper vagina) are formed.
Development of the structures derived from the wolffian ducts, including the epididymis, ductus deferens, ejaculatory ducts, and seminiferous tubules, requires high local concentrations of testosterone secreted from Leydig cells of the testis beginning at approximately 7 weeks’ gestation. In the absence of testosterone, wolffian ducts regress. Levels of testosterone in the circulation are insufficient to develop wolffian structures. In conditions in which the gonads develop asymmetrically (e.g., ovotesticular disorders of sexual development or mixed gonadal dysgenesis; see later), wolffian structures develop asymmetrically as well. Development of wolffian structures requires an intact androgen receptor.
External genital structures are also bipotential in early gestation and consist of the genital tubercle, genital folds (later, urethral-labial folds), and genital swelling (later, labioscrotal folds) (see Fig. 214-2 ). Differentiation to male genitalia occurs from approximately 8 to 14 weeks’ gestation under the influence of dihydrotestosterone, which must interact with an intact androgen receptor. The genital tubercle becomes the glans penis; the genital folds fuse to become the shaft of the penis and penile urethra, and the labioscrotal folds (derived from the genital swelling) fuse to become the scrotum. Without androgens, these structures become the clitoris, labia minora, and labia majora, respectively.
Many forms of genital ambiguity result from defects in steroid biosynthesis in the testes or adrenal cortex or from defective steroid metabolism in the placenta or in target tissues ( E-Fig. 214-1 ). Steroid biosynthesis in the testes and adrenals begins with the importation of cholesterol into mitochondria, a highly regulated process controlled largely by the steroidogenic acute regulatory (StAR) protein. Levels of StAR are controlled within the adrenals by adrenocorticotropic hormone (ACTH) and within the testis by HCG during the first trimester and by LH later in pregnancy.
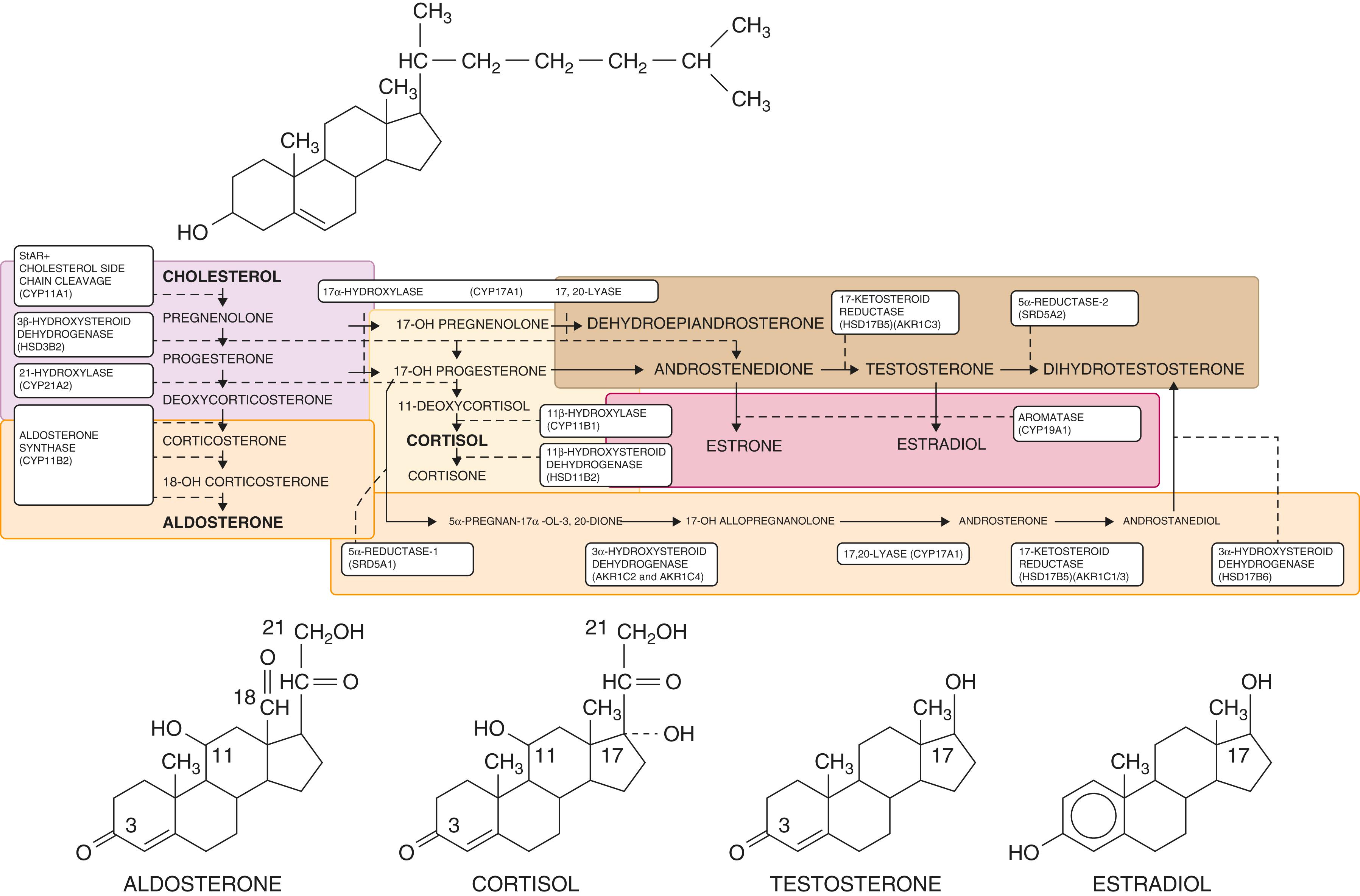
Within mitochondria, the side chain of cholesterol is cleaved between carbons 20 and 22 by the cholesterol side-chain cleavage enzyme (CYP11A1), which is a cytochrome P-450 enzyme. The product is pregnenolone, which is transported to the endoplasmic reticulum. Some pregnenolone is converted by 17α-hydroxylase (CYP17A1) to 17-hydroxypregnenolone. Both 17-hydroxypregnenolone and the remaining pregnenolone are converted by 3β-hydroxysteroid dehydrogenase (HSD3B2) to 17-hydroxyprogesterone and progesterone, respectively. The side chain of 17-hydroxypregnenolone is cleaved by the 17,20-lyase activity of CYP17A1 to dehydroepiandrosterone (DHEA). DHEA may also be converted to androstenedione by HSD3B2.
All the preceding steps can occur in the adrenal cortex, in Leydig cells of the testis, and (after puberty) in theca cells of ovarian follicles. Subsequent biosynthetic steps are specific to different glands. In the adrenal cortex, 17-hydroxyprogesterone is converted by 21-hydroxylase (CYP21A2) to 11-deoxycortisol, which is then converted in mitochondria to cortisol by 11β-hydroxylase (CYP11B1). Additionally, progesterone is converted to deoxycorticosterone by CYP21A2, which is then converted to aldosterone by aldosterone synthase (CYP11B2).
In Leydig cells of the testis, androstenedione is converted to testosterone by 17-ketosteroid reductase (17β-hydroxysteroid dehydrogenase type 3 [HSD17B3]); the same reaction occurs in theca cells of the ovary, catalyzed by 17β-hydroxysteroid dehydrogenase type 1 (HSD17B1). In granulosa cells of the ovary (after puberty), androstenedione and testosterone are converted by aromatase (CYP19A1) to estrone and estradiol, respectively. In the skin of the developing male external genitalia, steroid 5α-reductase (SRD5A2) converts testosterone to a more potent androgen, 5-dihydrotestosterone.
The placenta is a steroid-synthesizing and steroid-metabolizing tissue as well; it has high steroid sulfatase activity that converts DHEA sulfate from the fetal adrenal gland back to DHEA. DHEA is then successively converted by 3β-hydroxysteroid dehydrogenase type 1 (HSD3B1) and aromatase (CYP19A1) to androstenedione and estrone, respectively, which are then converted to estradiol by HSD17B1.
Genital ambiguity in genetic females is usually the result of exposure to excessive levels of androgens. Virilizing congenital adrenal hyperplasia, which is the most common cause of genital ambiguity in female infants, occurs in 1 in 16,000 births.
Conversely, severe deficiencies of androgens, if present early in gestation, cause ambiguous or female-appearing external genitalia in male infants. Usually, müllerian structures such as the uterus, cervix, and upper vagina are not present because the testes are able to secrete antimüllerian hormone. Thus individuals with these conditions have a short vagina ending in a blind pouch.
The fundamental defect among patients with any form of congenital adrenal hyperplasia is inadequate synthesis of cortisol (see E-Fig. 214-1 ). Inefficient cortisol synthesis signals the hypothalamus and pituitary to increase corticotropin-releasing hormone and ACTH, respectively ( Chapter 204 ). Consequently, the adrenal glands become hyperplastic, and steroid precursors accumulate proximal to the block in biosynthesis. In some conditions, these precursors can be converted to androgens.
Lipoid hyperplasia results from mutations in the STAR gene. Cholesterol is not imported efficiently into mitochondria and thus accumulates in cells. Steroid biosynthesis is drastically reduced because of the lack of substrate, and the lipid accumulation quickly kills steroid-synthesizing cells in both the adrenals and the testes. Thus affected male patients are born as phenotypically female because they cannot synthesize testosterone. Affected female patients may undergo transient spontaneous puberty because human ovarian granulosa cells do not synthesize steroid hormones (and thus do not accumulate cholesterol) until puberty. Both sexes have adrenal insufficiency and are unable to synthesize either cortisol or aldosterone. A nearly identical but rare phenotype results from mutations in the CYP11A1 gene that encodes the cholesterol side-chain cleavage enzyme itself.
Severe mutations in the CYP17A1 gene prevent the synthesis of any sex hormones. Affected male patients have female-appearing external genitalia but have no müllerian structures because the testes synthesize antimüllerian hormone. Affected female patients remain sexually infantile without hormone replacement. Milder mutations result in ambiguous genitalia in male patients. Although cortisol synthesis is also abolished, even severely affected individuals are able to synthesize corticosterone, which is an active glucocorticoid, as well as aldosterone, so they do not develop adrenal insufficiency. On the contrary, they secrete excessive amounts of deoxycorticosterone, which has mineralocorticoid activity, and are therefore prone to developing hypertension.
Whereas most CYP17A1 mutations affect both the hydroxylase and lyase activities, rare mutations can affect the lyase activity alone. Additionally, mutations in an accessory electron transfer protein, cytochrome b 5 , or the genes for two aldoketo reductases ( AKR1C2 and AKR1C4 ) can result in the same phenotype as 17,20-lyase deficiency (i.e., deficient androgen synthesis with normal cortisol synthesis).
Severe mutations in the HSD3B2 gene prevent the synthesis of aldosterone, cortisol, testosterone, and estrogens. Because DHEA, a weak androgen, is synthesized and secreted at high levels, some degree of phallic growth is present. Thus affected male patients have severely ambiguous genitalia, but affected female patients may have clitorimegaly. Both sexes develop adrenal insufficiency if they are untreated.
Many children with premature adrenarche (early development of axillary and pubic hair), as well as many women with polycystic ovary syndrome, have elevated levels of DHEA. However, mutations in HSD3B2 are rarely, if ever, found in such individuals, who instead have an imbalance in the relative levels of HSD3B2 and CYP17 activity within the adrenal cortex.
More than 90% of cases of congenital adrenal hyperplasia are caused by 21-hydroxylase deficiency that results from mutations in the CYP21A2 gene. CYP21A2 and a highly homologous pseudogene, CYP21A1P , are located within the major histocompatibility complex on chromosome 6p21.3, a genomic region noteworthy for a high rate of recombination. More than 90% of all mutations are the result of intergenic recombination between CYP21A2 and CYP21A1P . Most are transfers of deleterious mutations from CYP21A1P to CYP21A2 , whereas 20% are net deletions of CYP21A2 resulting from unequal meiotic crossover.
In patients with 21-hydroxylase deficiency, the adrenals produce excess 17-hydroxyprogesterone, 17-hydroxypregnenolone, and progesterone, which are further metabolized to DHEA and androstenedione. Once secreted, these substances are further metabolized to active androgens (testosterone and dihydrotestosterone) and, to a lesser extent, to estrogens (estrone and estradiol). Progesterone and 17-hydroxyprogesterone can also be metabolized to dihydrotestosterone by the alternative “backdoor” pathway ( E-Fig 214-1 ). Additionally, the adrenal gland can synthesize physiologically relevant quantities of 11-hydroxylated and 11-keto-androgens.
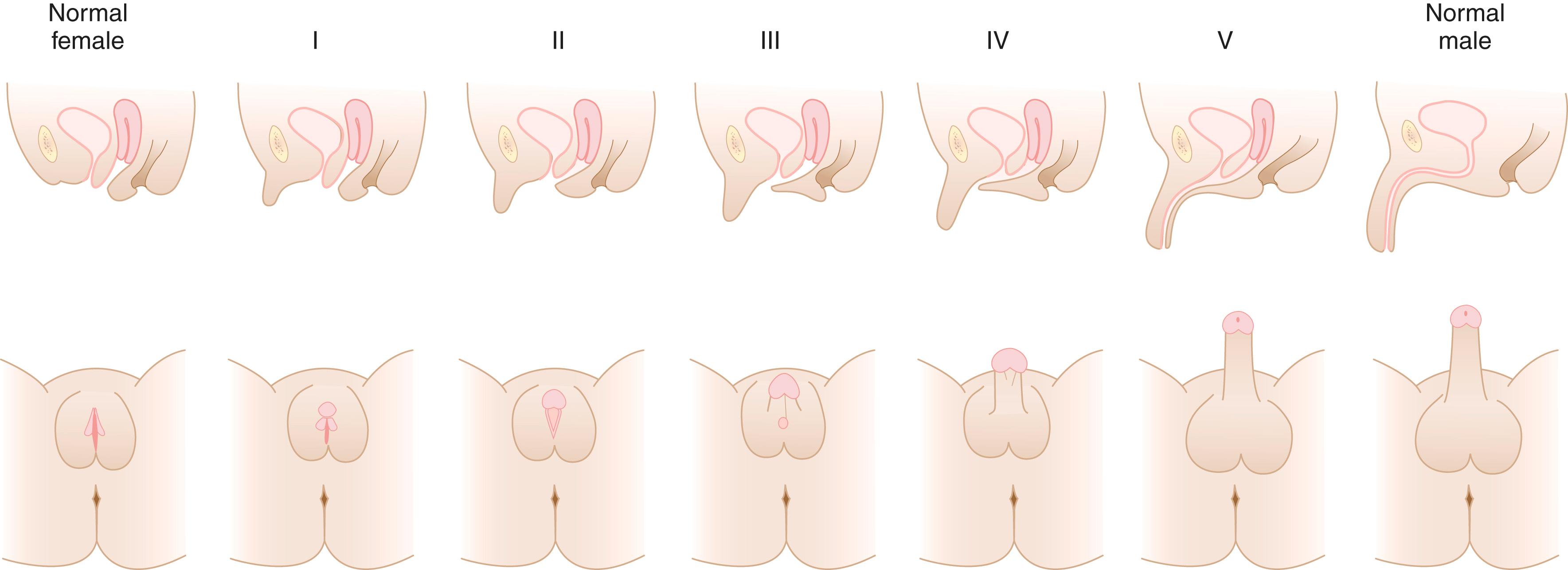
Adrenal secretion of excess androgen precursors does not significantly affect male sexual differentiation. In affected female patients, the urogenital sinus is in the process of septation when the fetal adrenal begins to produce excess androgens, which function to prevent the formation of separate vaginal and urethral canals. Further adrenal-derived androgens interact with androgen receptors in genital skin and induce clitoral enlargement, promote fusion of the labial folds, and cause rostral migration of the urethral/vaginal perineal orifice. However, internal wolffian structures such as the prostate gland and spermatic ducts are usually not virilized, presumably because development of the wolffian ducts requires markedly higher local concentrations of testosterone than the external genitalia. Nevertheless, severely affected female patients occasionally have some development of typically male internal genital structures.
Thus the typical result in severely affected girls is ambiguous or male-appearing external genitalia with perineal hypospadias and chordee, but without palpable testes ( Fig. 214-3 ). The severity of virilization is often quantitated using a five-point scale developed by Prader ( Fig. 214-4 ). The degree of genital ambiguity in female patients with classic congenital adrenal hyperplasia is correlated with the severity of enzymatic compromise conferred by each patient’s mutations.

Most patients (75%) cannot synthesize sufficient aldosterone to maintain sodium balance and are termed salt wasters . These patients are predisposed to episodic and potentially life-threatening hyponatremic dehydration. Patients with sufficient aldosterone production to prevent salt wasting and who have signs of prenatal virilization and/or markedly increased production of hormonal substrates of 21-hydroxylase (e.g., 17-hydroxyprogesterone) are termed simple virilizers . A mild nonclassic form occurs in 1/200 to 1/500 individuals and may cause postnatal androgen excess but not prenatal virilization.
Patients with 11β-hydroxylase deficiency have mutations in the CYP11B1 gene, with elevated levels of deoxycorticosterone and 11-deoxycortisol, as well as earlier cortisol precursors such as 17-hydroxyprogesterone. These patients secrete excess adrenal androgens, with consequences similar to those seen in 21-hydroxylase deficiency. However, patients with 11β-hydroxylase deficiency synthesize aldosterone normally and do not have problems with salt wasting. Instead, they are likely to become hypertensive as a result of elevated levels of deoxycorticosterone and its metabolites.
Lipoid hyperplasia, 17-hydroxylase/17,20 lyase deficiency, and HSD3B2 deficiency affect the biosynthesis of both corticosteroids and sex hormones. In contrast, two enzymatic defects affect only androgen biosynthesis. They have similar phenotypes. Affected male patients are born with ambiguous genitalia, but they virilize at puberty and often reassign themselves to a male gender if they were raised as females. They have absent müllerian structures as a result of the secretion of antimüllerian hormone by the testes.
This disorder is caused by mutations in the HSD17B3 gene. Although testosterone is not synthesized well, secretion of androstenedione, an active androgen, is unimpaired. Because several other isozymes have 17-ketosteroid reductase activity in other tissues, some testosterone is invariably synthesized, especially at puberty, when circulating levels of androstenedione increase.
Patients with 5α-reductase deficiency resulting from mutations in the SRD5A2 gene synthesize entirely normal amounts of testosterone, but they cannot synthesize adequate amounts of dihydrotestosterone, which is the most potent naturally occurring androgen. This enzyme is not expressed at high levels in the testes (circulating levels of dihydrotestosterone are relatively low); instead, it is expressed in genital skin. Internal wolffian structures do not require this enzyme and are intact; high testosterone levels at puberty induce significant phallic growth without 5α-reductase activity.
Mutations in CYP19A1 cause aromatase deficiency in both the fetus and the placenta. The placenta can convert DHEA sulfate to androstenedione and testosterone normally, but it cannot convert these androgens to estrone and estradiol. These androgens accumulate in both the fetal and maternal circulations and virilize both the mother and the affected fetus if it is female. Affected male infants are phenotypically normal. Affected female patients virilize further at puberty if they are untreated. The lack of aromatase activity within bone leads to tall stature in both sexes (because estrogens are required to close the growth plates) and later to osteoporosis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here