Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Cardioembolic stroke is a major etiology accounting for one-fifth of all ischemic strokes.
Recent advances in technology have enabled us to monitor heart rhythm remotely and detect paroxysmal atrial fibrillation.
Atrial cardiopathy is an area of further investigation as a risk factor for cardioembolic stroke, especially in patients with cryptogenic stroke.
CLOSE, Gore-REDUCE, DEFENSE-PFO, and RESPECT trials have shown that device closure of patent foramen ovale (PFO) is superior to medical therapy in preventing recurrent stroke in carefully selected patients.
Newer oral anticoagulants have shown equal or superior efficacy to warfarin in preventing ischemic stroke in nonvalvular atrial fibrillation, expanding treatment options for this patient population.
Reversal agents for newer oral anticoagulants are available.
Cardioembolic stroke is a major stroke subtype accounting for one-fifth of all ischemic strokes. , Advanced imaging technology has enabled us to easily identify potential cardiac sources of emboli. Since the underlying cardiac condition is often evident before stroke occurs and antithrombotic therapies are notably effective, cardiogenic emboli to the brain are among the most preventable causes of stroke.
With a thorough cardiac evaluation, a potential source of cardiogenic emboli can be identified in at least 30% of all patients with ischemic stroke. , However, potential cardioembolic sources often coexist with other cardiovascular disease risk factors. During the past two decades, new and better noninvasive cardiac imaging became available; therefore, new potential cardioembolic sources have been recognized. This situation is reflected in the increased frequency of cardioembolic stroke over time. Aggregate data from stroke registries conducted between 1988 and 1994 show mean frequency of cardioembolic stroke to be 20% (range, 17%–28%). , , Data from later stroke registries (1995–2001) showed a higher mean prevalence of cardioembolic stroke, at 25% (range 16%–38%).
Cardioembolic stroke is caused by a variety of cardiac disorders, each with a unique natural history and a variable response to antithrombotic therapy ( Fig. 64.1 ). The embolic material originating from the heart and proximal aorta can be quite diverse. The thrombi may be composed of varying proportions of platelets and fibrin, cholesterol fragments, tumor particles, or bacterial clusters. The natural history and response to antithrombotic therapy of each of these conditions are unique, and, consequently, each source of cardioembolic stroke should be considered separately. Therefore, cardioembolic stroke is not a single disease but a syndrome with diverse causes (see Fig. 64.1 ).
The incidence of ischemic stroke associated with cardioembolic sources varies greatly. Cardioembolic sources of stroke can be divided according to their stroke risk potential as “major-risk sources,” for which the risk for stroke is well established, or “minor-risk sources,” for which the risk for stroke has been incompletely established ( Table 64.1 ). The major-risk cardioembolic sources carry a substantial annual risk of emboli and a high risk of recurrence, and, usually, antithrombotic therapy is warranted for stroke prevention. Conversely, the so-called minor sources of emboli can cause stroke but have a low or uncertain risk of embolism and are more often coincidental than causal; thus, antithrombotic therapy is usually reserved for selected cases.
| Atrial | Valvular | Ventricular | |
|---|---|---|---|
| Major-risk sources | Atrial fibrillation Left atrial thrombus Left atrial myxoma Sustained atrial flutter |
Mitral stenosis Prosthetic cardiac valves Infective endocarditis calcification Marantic endocarditis |
Left ventricular thrombus (mobile or protruding) Recent anterior wall myocardial infarction Nonischemic dilated cardiomyopathy |
| Minor-risk sources | Patent foramen ovale Atrial septal aneurysm |
Mitral valve prolapse Calcific aortic stenosis Mitral annular Giant Lambl’s excrescences Fibroelastoma |
Left ventricular regional wall abnormalities Congestive heart failure Akinetic ventricular wall segment |
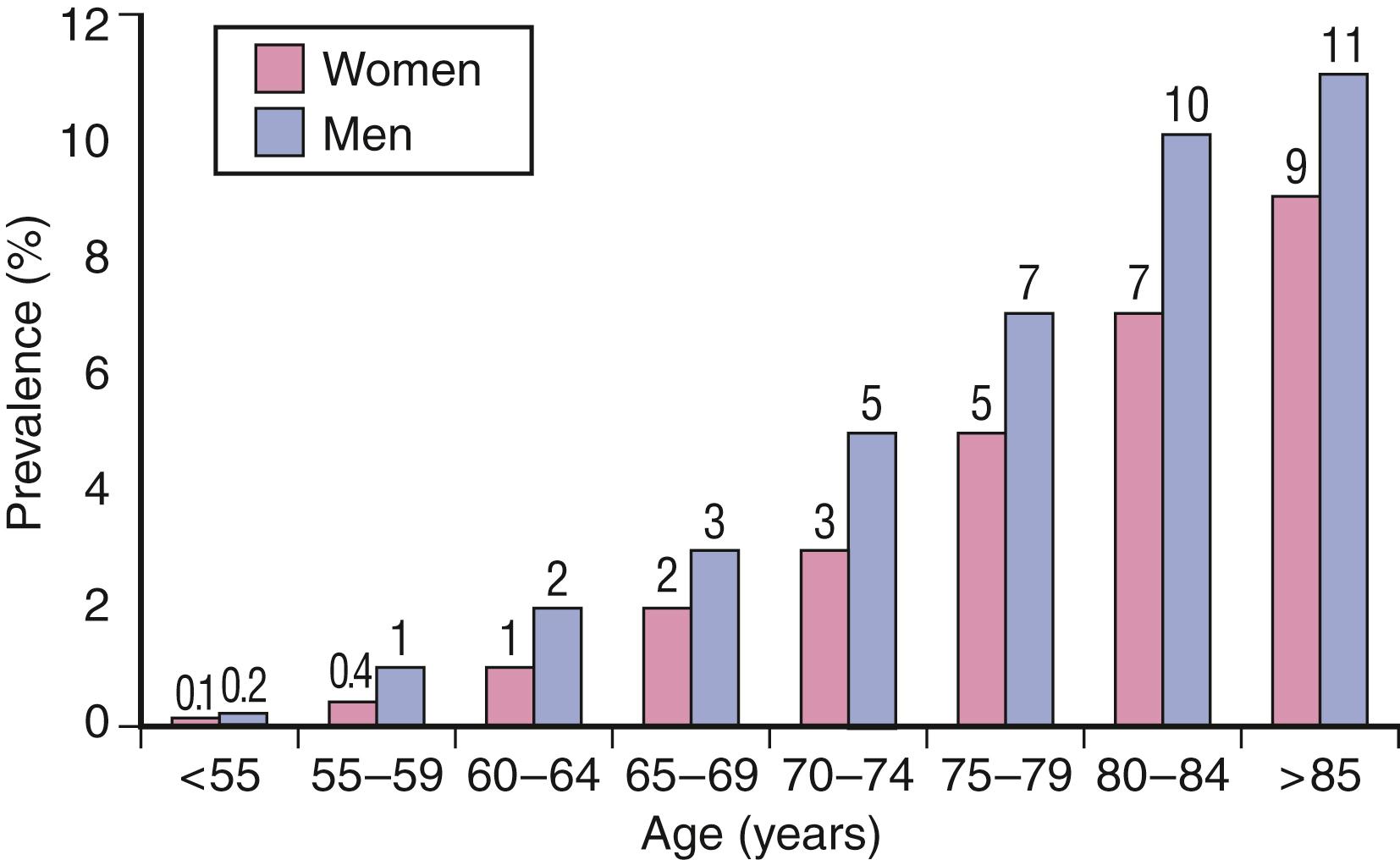
Atrial fibrillation (AF) is the most common cardiac arrhythmia, affecting 0.7%–0.9% of the general population of the United States (2.5 million people). , Its prevalence increases with age, being present in approximately 5% of persons at age 65 years and in 10% at age 80 years. AF is equally distributed in men and women, and the mean age of individuals affected is approximately 75 years ( Fig. 64.2 ). ,
The first-detected episode can proceed along different pathways. It can be self-limited without any recurrence, in which case it is termed “lone AF.” It can adopt a recurrence pattern with intervening sinus rhythm, termed as “paroxysmal AF.” If it persists for 7 days, it is termed “persistent.” These forms of AF are proposed by the American College of Cardiology (ACC)/American Heart Association (AHA)/European Society of Cardiology (ESC). It is important to note that the AF duration and its persistence can evolve over time either caused by ongoing pathophysiologic process or treatment. AF can be further divided into valvular versus nonvalvular AF. Valvular AF is defined as AF secondary to structural heart disease involving the valves, commonly the mitral valve. Nonvalvular AF is defined as AF without evidence of structural valvular heart disease preferably screened by an echocardiogram.
Nonvalvular AF is the etiology in 25% of all ischemic strokes. , , Older age is a major risk and AF is the diagnosed etiology in more than one-third of patients older than 70 years with ischemic stroke. The risk of ischemic stroke increases fivefold (from 1% to 5% per year) in elderly patients (mean age, 70 years) with nonvalvular AF, and approximately 18-fold in patients with AF and rheumatic mitral stenosis. AF accounts for approximately one-half of presumed cardioembolic strokes. Patients with AF are typically older and have large middle cerebral artery strokes associated with a high mortality rate during the first 30 days ( Table 64.2 ). ,
| Study | Mean Age (Years) | Stroke Rate %/Year AF | Stroke Rate %/Year Non-AF | Increased Relative Risk |
|---|---|---|---|---|
| Framingham (United States) (Wolf et al., 1991) | 70 | 4.1 | 0.7 | ×6 |
| Shibata (Japan) (Nakayama, 1997) | 65 | 5.0 | 0.9 | ×6 |
| Reykjavik (Iceland) (Onundarson, 1987) | 52 | 1.6 | 0.2 | ×7 |
Stroke associated with AF is attributed to embolism of thrombus from the left atrium (LA), the pathogenesis of which is complex. Thrombus most frequently forms in the left atrial appendage (LAA) and is a result of stasis, endothelial dysfunction, and a hypercoagulable state. Stasis results from the decreased emptying of the LAA due to loss of organized mechanical contraction during the cardiac cycle, as evidenced by the reduced LAA flow velocities. Moreover, AF seems to promote a hypercoagulable state and has been associated with biochemical markers of coagulation and platelet activation.
AF alone, however, may not be enough to promote thrombi formation. Other factors may also contribute, because associated cardiovascular disease and age appear to influence the stroke risk in AF and, hence, also influence the formation of atrial appendage thrombi. This variable risk is reflected by the wide range of stroke risk in patients with AF (“lone AF”), a phenomenon not observed with other “high-risk” conditions. Temporal variation in factors that influence thrombus formation may explain the intermittency of embolism in different patients with AF and even within each patient. Embolic events are intermittent in AF, sometimes separated by years. A balance between the formation and inhibition of clot is likely present in the atrial appendage of such patients. This balance is influenced by atrial size, appendage flow velocities, and coagulation factors; thus, the type and intensity of antithrombotic therapy required to inhibit appendage thrombi may differ among patients with AF and, over time, for the same patient. In summary, complex electrophysiologic and thromboembolic processes lead to embolic events in AF.
The overall incidence of ischemic stroke among people with AF is approximately 5% per year. The rate of stroke varies widely, however, ranging from 0.5% per year in young patients with “lone AF” to 12% per year in those with prior transient ischemia attack (TIA) or stroke. This variation depends on coexisting cardiovascular disorders. , , Therefore, identification of subgroups of patients with AF with relatively high vs low absolute rates of stroke is important for selecting prophylactic antithrombotic therapy. Different scores have been developed and validated to predict this risk in an individual.
The CHADS2 score is widely used as the most reliable scheme of stratification that allows the separation of AF patients according to the risk of stroke. This scheme was validated in an independent cohort. The acronym stands for:
C = congestive heart failure (1 point)
H = hypertension (1 point)
A = age older than 75 (1 point)
D = diabetes mellitus (DM)(1 point)
S2 = history of stroke or TIA (2 points)
In a large validation cohort, the estimated risk of stroke per year based on CHADS2 score is shown in Table 64.3 . A limitation of the CHADS2 score applies to secondary prevention in patients with prior stroke or TIA and no other risk factors. Therefore, the CHA2DS2-VASc index was recently developed to further refine the risk calculation of CHADS2 by including additional variables of vascular disease, age > 65, and female gender. ,
| CHADS2 Score ∗ | Risk | Stroke Rate (%/Year) |
|---|---|---|
| 0 | Low | 0.5 |
| 1 | Low | 1.5 |
| 2 | Moderate | 2.5 |
| 3 | High | 5 |
| 4 | High | 6 |
| 5–6 | Very high | 7 |
∗ For CHADS2 (congestive heart failure, hypertension, age older than 75 year, diabetes mellitus) score and validation, see Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: Results from the national registry of atrial fibrillation. JAMA 2001;285:2864–2870. Level of Evidence Class I.
The score is calculated as below:
C = congestive heart failure (1 point)
H = hypertension (1 point)
A2 = age older than 75 (2 point)
D = DM (1 point)
S2 = history of stroke or TIA (2 points)
V = vascular disease (previous myocardial infarction, peripheral artery disease, aortic plaque) (1 point)
Age = 65–74 (1 point)
Sex = female (1 point)
The estimated risk of stroke per year based on CHA2DS2-VASc score is shown in Table 64.4 . ,
| CHA2DS2-VASc Score ∗ | Risk | Stroke Rate (% per Year) |
|---|---|---|
| 0 | Low | 0 |
| 1 | Low | 1.3 |
| 2 | Moderate | 2.2 |
| 3 | Moderate | 3.2 |
| 4 | High | 4 |
| 5 | High | 6.7 |
| 6 | Very high | 9.8 |
| 7 | Very high | 9.6 |
| 8 | High | 6.7 |
| 9 | Very high | 15.2 |
∗ For CHA2DS2-VASc (congestive heart failure, hypertension, age older than 65 years, diabetes mellitus, vascular disease and sex) score and validation, see Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: The Euro Heart Survey on atrial fibrillation. Chest . 2010;137:263–272. Level of Evidence Class IIa.
The short-term risk of stroke recurrence after an acute stroke in patients with AF is approximately 5% in 2 weeks, which is a value much lower than previously considered.
The goal of anticoagulation is to prevent ischemic events but also to minimize the risk of bleeding related to anticoagulation. In this regard, the HAS-BLED score was developed to predict risk of hemorrhage in patients on anticoagulation.
The score is calculated as below:
H = history of uncontrolled hypertension (>160 mm Hg)
A = abnormal renal/liver function (one point for presence of renal or liver impairment, maximum two points)
S = stroke (previous history, particularly lacunar)
B = bleeding history or predisposition (anemia)
L = labile international normalized ratio (INR) (i.e., therapeutic time in range, 60%)
E = elderly (>65 years)
D = drugs/alcohol concomitantly (antiplatelet agents, nonsteroidal anti-inflammatory drugs; one point for drugs plus one point for alcohol excess, maximum two points)
The estimated risk of bleeding events per 100 patient-years based on the HAS-BLED score is shown in Table 64.5 . ,
| HAS-BLED Score ∗ | Bleeding Risk (% per 100 Patient-Years) |
|---|---|
| 0 | 1.2 |
| 1 | 2.8 |
| 2 | 3.6 |
| 3 | 6.0 |
| 4 | 9.5 |
| 5 | 7.4 |
∗ For HAS-BLED (hypertension, abnormal renal/liver function, stroke, bleeding history or predisposition, labile international normalized ratio, elderly, drugs/alcohol concomitantly) score and validation see Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: The Euro Heart Survey. Chest . 2010;138:1093–1100. Level of Evidence Class IIb.
The risk of stroke recurrence as highlighted above makes it imperative to diagnose AF promptly to provide effective stroke prevention therapy. Paroxysmal AF (PAF) is a major hindrance in achieving this goal and has been suggested as a cause for cryptogenic strokes. Brief asymptomatic PAF events may remain undetected by traditional methods of screening. Recent technological advances have made it possible to perform long-term invasive and noninvasive cardiac rhythm monitoring up to months or even years after a stroke. The diagnostic yield of these monitoring strategies is high (an average of 11.5%; 95% confidence interval [CI], 8.9%–14.3%) and enables detection of AF in a large number of cryptogenic stroke patients. The CRYSTAL-AF study showed high yield of AF detection with insertable cardiac monitor (ICM). AF detection was 8.9% of patients at 6 months (hazard ratio (HR], 6.4; 95% CI, 1.9–21.7; P < .001) and 12.4% at 12 months (HR, 7.3; 95% CI, 2.6–20.8; P < .001) in the ICM group versus 1.4% of patients at 6 months and 2.0% at 12 months in the control group.
The Asymptomatic Stroke and Atrial Fibrillation Evaluation in Pacemaker Patients (ASSERT) trial showed an association between brief runs (>6 minutes) of subclinical AF and stroke/systemic embolism risk (HR, 2.49; 95% CI, 1.28–4.85; P = .007). In this study, there was no temporal association between subclinical AF and stroke or systemic embolism. This challenges the concept that AF is the direct cause of stroke in all patients with this dysrhythmia and argues that, perhaps, atrial dysfunction or “cardiopathy” is the direct cause and AF may be a manifestation. In fact, authors have suggested that fibrotic changes in the atrium detected on cardiac magnetic resonance imaging with late gadolinium enhancement may be the precursor to the development of AF and may constitute the underlying thrombogenic substrate leading to embolic events.
Recent studies have suggested that ischemic stroke can occur in patients with atrial cardiopathy without the electrocardiogram (ECG) signature of AF. For instance, left atrial enlargement has been shown to be associated with increased risk of first ischemic stroke, recurrent embolic stroke, and nonlacunar infarcts, and these associations were independent of AF. In addition, studies have shown that left atrial abnormality on ECG manifested as increased p-wave terminal force in lead V1 (PTFV1) has also been shown to be associated with ischemic stroke and brain infarcts, particularly those related to embolism, after adjusting for baseline and incident AF. Moreover, serum markers of atrial dysfunction had similar associations. For instance, N-terminal pro b-type natriuretic peptide (NT-proBNP) is a marker of atrial strain that, in several epidemiologic and population-based cohorts has been also proven to be associated with incident ischemic stroke, , particularly those related to embolism, after adjusting for AF. Since these biomarkers are also associated with incident AF, it remains unclear if these associations were mediated by subclinical AF, particularly because patients in these studies did not undergo continuous monitoring, and more studies are needed to answer this questions.
Nevertheless, patients with atrial cardiopathy may be a subgroup of patients who may benefit from anticoagulation. A post-hoc analysis of the Warfarin-Aspirin Recurrent Stroke Study (WARSS) showed that while warfarin was not superior for prevention of recurrent stroke or death in patients with noncardioembolic stroke, patients with NT-proBNP >750 pg/mL (a biomarker of atrial cardiopathy) had a lower risk of stroke or death with warfarin versus aspirin (HR, 0.30; 95% CI, 0.12–0.84). In addition, the NAVIGATE-ESUS trial showed no benefit of rivaroxaban over aspirin in recurrent stroke reduction patients with embolic stroke of undetermined source (ESUS) (HR, 1.07; 95% CI, 0.87–1.33; P = .52) but with a higher risk of major hemorrhage (HR, 2.72; 95% CI, 1.68–4.39; P < .001). A post-hoc analysis of NAVIGATE-ESUS showed a benefit of rivaroxaban over aspirin in patients with moderate-to-severe left atrial enlargement (HR,0.26; 95% CI, 0.07–0.94). The AtRial Cardiopathy and Antithrombotic Drugs In prevention After cryptogenic stroke (ARCADIA) trial is currently randomizing patients with cryptogenic stroke and evidence of atrial cardiopathy by one of its biomarkers (NT-prBNP >250 pg/mL, severe left atrial enlargement, or PTFV1 >5000 μV×ms) to apixaban versus aspirin to investigate whether apixaban would reduce the risk of stroke or death in this patient population. In addition, the cutoffs of the atrial biomarkers that portend an increased risk of stroke remain unclear and will be investigated in ARCADIA.
The efficacy of antithrombotic therapies to prevent stroke in nonvalvular AF has been well established by randomized clinical trials. An aggregate analysis showed that anticoagulation with warfarin reduces ischemic stroke by 64% in comparison with the rate in untreated patients, and an efficacy analysis indicated an even greater benefit. Warfarin was effective in preventing disabling stroke by 59% and nondisabling stroke by 61%. The absolute risk reduction in all strokes from the use of warfarin was 2.7% per year for primary prevention (number needed to treat [NNT] for 1 year to prevent one stroke = 37) and 8.4% per year for secondary prevention (NNT = 12). When only ischemic strokes were considered, adjusted-dose warfarin was associated with a 67% relative risk reduction (RRR) (95% CI, 54%–77%). In addition, the increase in the rate of major bleeding among elderly patients with AF undergoing anticoagulation in these trials was only 0.3%–2.0% per year with a target INR of 1.5–4.0. The risk of major hemorrhage in elderly patients with AF who are taking oral anticoagulants seems to be related to the intensity of anticoagulation, patient age, and fluctuation in INR.
The efficacy of aspirin, with doses ranging from 50 to 1300 mg/day, for stroke prevention in patients with AF has been tested in eight trials, which included 4876 participants. Comparing aspirin alone with placebo or no treatment, aspirin was associated with a 19% reduction in incidence of stroke (95% CI, 1%–35%). For primary prevention, there was an absolute risk reduction of 0.8% per year (NNT = 125) and for secondary prevention trials a reduction of 2.5% per year (NNT = 40). When only ischemic strokes are considered, aspirin results in a 21% reduction in strokes (95% CI, 1%–38%). When all antiplatelet agents are considered, stroke was reduced by 22% (95% CI, 6%–35%).
Eight trials compared warfarin and other vitamin K antagonists with various dosages of aspirin, other antiplatelet agents in three trials, and aspirin combined with low-fixed-dose warfarin in two trials. For the 11 trials that compared adjusted-dose warfarin with antiplatelet therapy alone, warfarin was associated with a 37% reduction in strokes (95% CI, 23%–48%). In the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE-W), anticoagulation therapy was superior to the combination clopidogrel plus aspirin (RRR, 40%; 95% CI, 18–56%). The risk of intracranial hemorrhage with adjusted-dose warfarin was double that with aspirin. The absolute risk increase, however, was small (0.2% per year).
Unquestionably, warfarin is highly efficacious for preventing stroke in patients with AF and relatively safe for selected patients. Aspirin offers less benefit, possibly by decreasing noncardioembolic strokes in these patients. The choice of antithrombotic prophylaxis is based on the risk stratification (see Tables 64.3 and 64.4 ). Long-term anticoagulation cannot be recommended for all unselected patients with AF, because most of them would not experience strokes even if untreated. Patients with AF with a relatively low risk of subsequent stroke would not substantially benefit from the use of warfarin, because the absolute risk reduction would be small (RRR, 1% per year). In these patients, anticoagulation may not be warranted. On the contrary, patients with AF who have a high risk for ischemic stroke (higher than 7%) because of a history of hypertension, prior TIA or stroke, or ventricular dysfunction would have a significantly lower stroke rate if they received anticoagulation.
High-risk patients who are good candidates for anticoagulation realize remarkable benefit from warfarin. For high-risk patients 75 years or younger, a target INR of 2.5 (range, 2.0–3.0) is effective and safe; for those older than 75 years, choosing a slightly lower target (INR 2.0–2.5), with the hope of minimizing bleeding complications, appears appropriate. Patients younger than 60 years with “lone AF” may not require long-term anticoagulation and, because their intrinsic risk for stroke is small, aspirin may be sufficient.
PAF, with underlying causes similar to those in sustained or constant AF, constitutes between 25% and 60% of all cases of AF. Epidemiologic data have suggested that the risk of stroke for patients with PAF is intermediate between those of patients with constant AF and patients with sinus rhythm. However, when data are controlled for stroke risk factors, PAF involves a stroke risk similar to that of constant AF. The risk-benefit ratio for antithrombotic therapy in patients with PAF has not been evaluated in clinical trials. Therefore, the recommendations are based on indirect data from AF trials, so the approach to patients with PAF should be the same as that to patients with sustained AF.
The risks and benefits of combination of an oral anticoagulant and an antiplatelet agent compared with an oral anticoagulant alone for secondary prevention of cardioembolic stroke have not been clearly established. Turpie et al. studied young patients with prosthetic valves and showed a significant reduction of embolic events in those assigned to combination therapy and no significant increase in the incidence of intracerebral hemorrhage (ICH; seven patients vs. three patients, respectively). However, in view of the occurrence of only a few events and the patients’ ages, these results cannot be generalized to different groups of patients (i.e., elderly with established cerebrovascular disease).
Recent meta-analyses comparing warfarin plus antiplatelet with warfarin alone in different populations found that the addition of antiplatelets to warfarin significantly increased the risk of ICH especially in elderly populations, and the risk-benefit ratio of combination therapy was higher for elderly patients with prior ischemic strokes than for young patients with prosthetic valvular disease. , This becomes a major issue in patients who undergo coronary artery stenting and require dual-antiplatelet therapy for drug-eluting stents, and also have indication for anticoagulation due to atrial fibrillation. The WOEST trial addressed this particular dilemma and found that the risk of bleeding complications is highest with triple therapy and recommended using clopidogrel with warfarin in patients with coronary stents and need for anticoagulation.
Although warfarin is highly efficacious in preventing systemic emboli in AF patients, its use is restricted by the narrow therapeutic window, multiple drug interactions, and the need for permanent INR monitoring. Consequently, owing to the inherent limitations for the use of oral anticoagulants in patients with AF, there is a need to develop and test novel antithrombotic agents with a much safer profile and wider therapeutic window than warfarin.
Recently, three new oral anticoagulants dabigatran, rivaroxaban, apixaban, and edoxaban have been approved by the US Food and Drug Administration (FDA) for use in nonvalvular, atrial fibrillation patients ( Table 64.6 ). ,
| Drug | Target | Dosing | Onset (h) | Half-Life (h) | Antidote |
|---|---|---|---|---|---|
| Apixaban | Factor Xa | Twice a day | 3 | 12 | Yes |
| Rivaroxaban | Factor Xa | Once a day | 3 | 9 | Yes |
| Dabigatran | Thrombin | Twice a day | 1–2 | 12–17 | Yes |
| Edoxaban | Thrombin | Once a day | 1–2 | 10–14 | Yes |
Dabigatran etexilate is an oral pro-drug that is converted to dabigatran, a direct, competitive inhibitor of factor IIa (thrombin). The Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) compared open-label warfarin with two fixed, blinded doses of dabigatran (110 or 150 mg twice daily) in patients with AF and at least one additional stroke risk factor (previous stroke or TIA, left ventricular ejection fraction <40%, New York Heart Association heart failure classification of II or higher, age ≥75 years, or age 65–74 years plus diabetes mellitus, hypertension, or coronary artery disease). The primary outcome was stroke or systemic embolism; secondary outcomes included stroke, systemic embolism, and death. The primary safety outcome was major hemorrhage. A net clinical benefit was defined as an unweighted composite of stroke, systemic embolism, pulmonary embolism, myocardial infarction, death, or major hemorrhage.
For the primary outcome of stroke or systemic embolism, both dabigatran 110 mg twice daily (1.53% per year) and dabigatran 150 mg twice daily (1.11% per year) were noninferior to warfarin (1.69% per year); dabigatran 150 mg twice daily was also superior to warfarin (RR, 0.66; 95% CI, 0.53–0.82). Compared with warfarin, the risk of hemorrhagic stroke was lower with both dabigatran 110 mg twice daily (RR, 0.31; 95% CI, 0.17–0.56) and dabigatran 150 mg twice daily (RR, 0.26; 95% CI, 0.14–0.49).
Major bleeding in RE-LY was lower with dabigatran 110 mg twice daily (2.71% per year; RR, 0.80; 95% CI, 0.69–0.93), but similar for dabigatran 150 mg twice daily (3.11% per year; RR, 0.93; 95% CI, 0.81–1.07) compared with warfarin (3.36% per year). The rate of gastrointestinal bleeding was higher with dabigatran 150 mg twice daily (1.51% per year) than with warfarin (1.02% per year) or dabigatran 110 mg twice daily (1.12% per year; P < .05). Rates of life-threatening and intracranial bleeding, respectively, were higher with warfarin (1.80% and 0.74%) than with either dabigatran 110 mg twice daily (1.22% and 0.23%) or dabigatran 150 mg twice daily (1.45% and 0.30%).
It is interesting to note that FDA only approved the 150 mg twice-daily dose and the 75 mg twice-daily regimen for patients with low creatinine clearance (15–30 mL/min). This decision raised comment in the medical community, since the 110 mg twice-daily dose was approved both in Canada and Europe. Moreover, the 110 mg twice-daily dose showed better safety profile in terms of bleeding events, as mentioned earlier. The 75 mg twice-daily dose was approved only on pharmacokinetic and pharmacodynamics modeling. The FDA responded to this concern by highlighting the superiority of the 150 mg twice-daily dose over warfarin, assuming normal renal function.
Measuring the anticoagulant effect of dabigatran is difficult. Activated partial thromboplastin time, endogenous thrombin potential lag time, thrombin time, and Ecarin clotting time can be used. Ecarin clotting time is a clinical assay, which can be used to measure the thrombin activity and, subsequently, is affected by thrombin inhibitors.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here